1. Uhry Z, Belot A, Colonna M, Bossard N, Rogel A, Iwaz J, et al. National cancer incidence is estimated using the incidence/mortality ratio in countries with local incidence data: is this estimation correct? Cancer Epidemiol. 2013; 37:270–277. PMID:
23312453.
2. Kim JC. Genopathogenesis of Colorectal Cancer. J Korean Surg Soc. 2005; 69:189–198.
3. Berstad P, Loberg M, Larsen IK, Kalager M, Holme O, Botteri E, et al. Long-term lifestyle changes after colorectal cancer screening: randomised controlled trial. Gut. 2015; 64:1268–1276. PMID:
25183203.
4. Sun J, Kato I. Gut microbiota, inflammation and colorectal cancer. Version 2. Genes Dis. 2016; 3:130–143. PMID:
28078319.
5. Chen HM, Yu YN, Wang JL, Lin YW, Kong X, Yang CQ, et al. Decreased dietary fiber intake and structural alteration of gut microbiota in patients with advanced colorectal adenoma. Am J Clin Nutr. 2013; 97:1044–1052. PMID:
23553152.
6. Rowland IR. The role of the gastrointestinal microbiota in colorectal cancer. Curr Pharm Des. 2009; 15:1524–1527. PMID:
19442169.
7. Wang T, Cai G, Qiu Y, Fei N, Zhang M, Pang X, et al. Structural segregation of gut microbiota between colorectal cancer patients and healthy volunteers. ISME J. 2012; 6:320–329. PMID:
21850056.
8. Zhu Q, Gao R, Wu W, Qin H. The role of gut microbiota in the pathogenesis of colorectal cancer. Tumour Biol. 2013; 34:1285–1300. PMID:
23397545.
9. Ley RE, Peterson DA, Gordon JI. Ecological and evolutionary forces shaping microbial diversity in the human intestine. Cell. 2006; 124:837–848. PMID:
16497592.
10. Saleh M, Trinchieri G. Innate immune mechanisms of colitis and colitis-associated colorectal cancer. Nat Rev Immunol. 2011; 11:9–20. PMID:
21151034.
11. Peters BA, Dominianni C, Shapiro JA, Church TR, Wu J, Miller G, et al. The gut microbiota in conventional and serrated precursors of colorectal cancer. Microbiome. 2016; 4:69. PMID:
28038683.
12. Sanapareddy N, Legge RM, Jovov B, McCoy A, Burcal L, Araujo-Perez F, et al. Increased rectal microbial richness is associated with the presence of colorectal adenomas in humans. ISME J. 2012; 6:1858–1868. PMID:
22622349.
13. Sze MA, Baxter NT, Ruffin MT 4th, Rogers MAM, Schloss PD. Normalization of the microbiota in patients after treatment for colonic lesions. Microbiome. 2017; 5:150. PMID:
29145893.
14. Gallimore AM, Godkin A. Epithelial barriers, microbiota, and colorectal cancer. N Engl J Med. 2013; 368:282–284. PMID:
23323906.
15. Grivennikov SI, Wang K, Mucida D, Stewart CA, Schnabl B, Jauch D, et al. Adenoma-linked barrier defects and microbial products drive IL-23/IL-17-mediated tumour growth. Nature. 2012; 491:254–258. PMID:
23034650.
16. Nakatsu G, Li X, Zhou H, Sheng J, Wong SH, Wu WK, et al. Gut mucosal microbiome across stages of colorectal carcinogenesis. Nat Commun. 2015; 6:8727. PMID:
26515465.
17. Feng Q, Liang S, Jia H, Stadlmayr A, Tang L, Lan Z, et al. Gut microbiome development along the colorectal adenoma-carcinoma sequence. Nat Commun. 2015; 6:6528. PMID:
25758642.
18. Magoč T, Salzberg SL. FLASH: fast length adjustment of short reads to improve genome assemblies. Bioinformatics. 2011; 27:2957–2963. PMID:
21903629.
19. Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010; 7:335–336. PMID:
20383131.
20. Flemer B, Lynch DB, Brown JM, Jeffery IB, Ryan FJ, Claesson MJ, et al. Tumour-associated and non-tumour-associated microbiota in colorectal cancer. Gut. 2017; 66:633–643. PMID:
26992426.
21. Kasai C, Sugimoto K, Moritani I, Tanaka J, Oya Y, Inoue H, et al. Comparison of human gut microbiota in control subjects and patients with colorectal carcinoma in adenoma: terminal restriction fragment length polymorphism and next-generation sequencing analyses. Oncol Rep. 2016; 35:325–333. PMID:
26549775.
22. Sinha R, Ahn J, Sampson JN, Shi J, Yu G, Xiong X, et al. Fecal microbiota, fecal metabolome, and colorectal cancer interrelations. PLoS One. 2016; 11:e0152126. PMID:
27015276.
23. Mima K, Nishihara R, Qian ZR, Cao Y, Sukawa Y, Nowak JA, et al. Fusobacterium nucleatum in colorectal carcinoma tissue and patient prognosis. Gut. 2016; 65:1973–1980. PMID:
26311717.
24. Cong J, Zhu H, Liu D, Li T, Zhang C, Zhu J, et al. A pilot study: changes of gut microbiota in post-surgery colorectal cancer patients. Front Microbiol. 2018; 9:2777. PMID:
30515141.
25. Jin Y, Liu Y, Zhao L, Zhao F, Feng J, Li S, et al. Gut microbiota in patients after surgical treatment for colorectal cancer. Environ Microbiol. 2019; 21:772–783. PMID:
30548192.
26. Kong C, Gao R, Yan X, Huang L, He J, Li H, et al. Alterations in intestinal microbiota of colorectal cancer patients receiving radical surgery combined with adjuvant CapeOx therapy. Sci China Life Sci. 2019; 62:1178–1193. PMID:
30796721.
27. Dethlefsen L, Relman DA. Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci U S A. 2011; 108 Suppl 1(Suppl 1):4554–4561. PMID:
20847294.
28. Zwielehner J, Lassl C, Hippe B, Pointner A, Switzeny OJ, Remely M, et al. Changes in human fecal microbiota due to chemotherapy analyzed by TaqMan-PCR, 454 sequencing and PCR-DGGE fingerprinting. PLoS One. 2011; 6:e28654. PMID:
22194876.
29. Zeller G, Tap J, Voigt AY, Sunagawa S, Kultima JR, Costea PI, et al. Potential of fecal microbiota for early-stage detection of colorectal cancer. Mol Syst Biol. 2014; 10:766. PMID:
25432777.
30. Lin XH, Jiang JK, Luo JC, Lin CC, Ting PH, Yang UC, et al. The long term microbiota and metabolic status in patients with colorectal cancer after curative colon surgery. PLoS One. 2019; 14:e0218436. PMID:
31199857.
 . In order to measure beta diversity, the difference in organism composition was measured according to Bray-Curtis distance as follows:
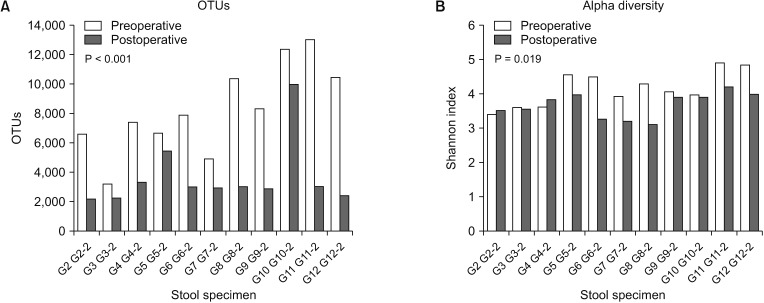
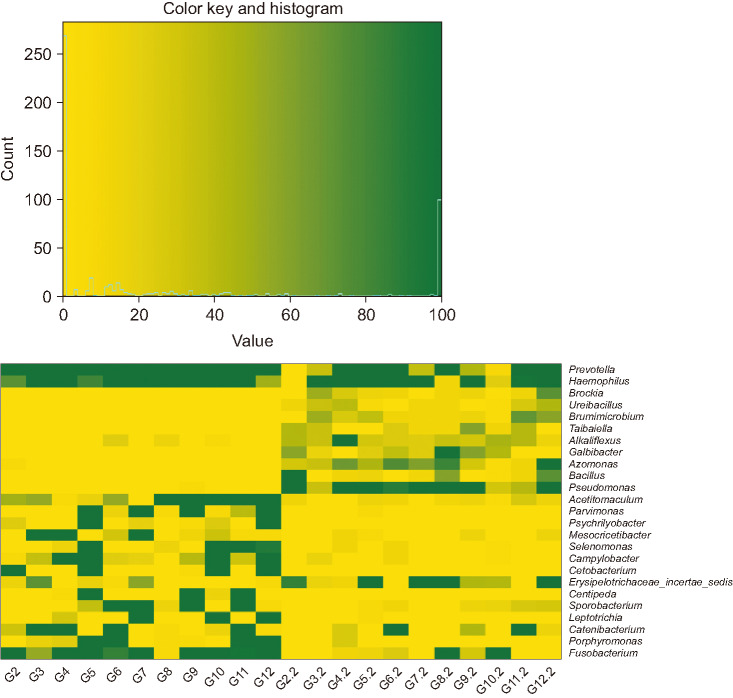
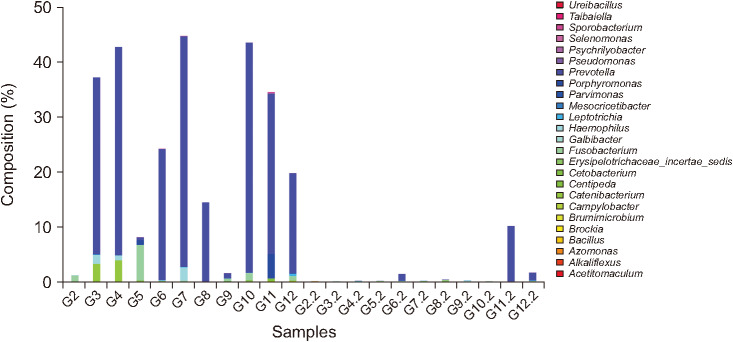
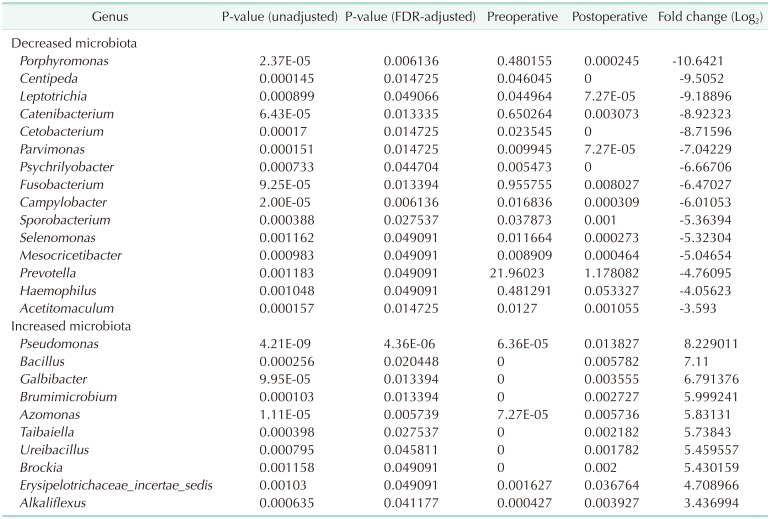
. In order to measure beta diversity, the difference in organism composition was measured according to Bray-Curtis distance as follows:  . Principal component analysis (PCA) was then performed using the measured beta diversities. Continuous variables (OTUs and alpha diversity) were analyzed using the Student t-test or Wilcoxon rank-sum test following normality tests. The edge R software version 3.6.8 (Bioconductor, Garvan Institute of Medical Research, Darlinghurst, NSW, Australia) was used to compare the microbial composition between preoperative and postoperative stool samples. An adjusted P-value < 0.05 was considered statistically significant and all statistical analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
. Principal component analysis (PCA) was then performed using the measured beta diversities. Continuous variables (OTUs and alpha diversity) were analyzed using the Student t-test or Wilcoxon rank-sum test following normality tests. The edge R software version 3.6.8 (Bioconductor, Garvan Institute of Medical Research, Darlinghurst, NSW, Australia) was used to compare the microbial composition between preoperative and postoperative stool samples. An adjusted P-value < 0.05 was considered statistically significant and all statistical analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).



 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download