Abstract
Purpose
The use of prophylactic central neck dissection (PCND) and the extent of thyroid surgery in clinically node-negative (cN0) papillary thyroid carcinoma (PTC) are controversial. This study aimed to investigate whether the extent of thyroid surgery influences the prognosis of patients with PTC with central lymph node metastasis (N1a), which was cN0 but pathologically confirmed after PCND.
Methods
This was a single-center retrospective study using medical records. Patients who underwent thyroid surgery with PCND for the treatment of PTC between 2004 and 2019 were included. Predictive factors and local recurrence rates were analyzed.
Results
Of 2,274 patients with cN0 PTC, 436 were confirmed to have pathologic N1a disease after PCND. Among them, 340 patients (78.0%) underwent total thyroidectomy (TT) and 96 patients (22.0%) underwent less than TT. Of the 374 patients who were followed up for >6 months, 5 (1.3%) experienced recurrence. The 15-year recurrence-free survival (RFS) rate was 98.2%. No clinicopathologic factor was predictive of tumor recurrence. RFS tended to be lower in patients who underwent less than TT than in those who underwent TT; however, the difference was not statistically significant.
Conclusion
Our study showed low recurrence rates in patients with cN0 PTC pathologically confirmed as N1a after PCND. The RFS did not differ according to the extent of thyroid surgery. Considering the low recurrence rate and the surgical morbidity associated with thyroid surgery, less than TT with PCND may be considered for patients with cN0 unilateral PTC even with a pathologic staging of N1a after PCND.
Papillary thyroid carcinoma (PTC) is the most common type of differentiated thyroid carcinoma (DTC) and has shown better prognosis than the other types. With the accumulation of the results of thyroid cancer treatment and evidence from numerous studies, the guidelines for the treatment of DTCs have evolved. The American Thyroid Association (ATA) published guidelines for the management of thyroid nodules and DTCs in 2006 [1] and revised the guidelines in 2009 [2]. These guidelines recommended near-total thyroidectomy (near-TT) or TT for all tumors >1 cm, whereas thyroid lobectomy alone may be sufficient for <1 cm, low-risk, unifocal, intrathyroidal papillary carcinomas in the absence of prior head and neck irradiation or radiologically or clinically involved neck lymph node (LN) metastases (cN0). In 2015, the ATA modified their guidelines for the treatment of thyroid cancer to recommend a more conservative approach and a reduced extent of surgery compared with the previous guidelines [3]. In the current ATA guidelines, near-TT or TT is recommended for patients with thyroid cancer >4 cm, those with gross extrathyroidal extension (ETE), or those with clinically apparent metastatic disease to the nodes (cN1) or distant sites (cM1). For patients with DTC ≤1 cm or between 1 and 4 cm, thyroid lobectomy can be chosen if there is no evidence of ETE and cN1. In the National Comprehensive Cancer Network (NCCN) guidelines, completion thyroidectomy is recommended in the presence of PTC >4 cm, positive resection margins, gross ETE, macroscopic multifocal disease >1 cm, macroscopic LN metastasis defined as more than 3–5 involved nodes or >5 mm in largest dimension, and vascular invasion [4].
Regional LN metastases have been associated with poor survival outcomes and the risk of recurrent disease [56], and therapeutic central neck dissection (CND) is the standard treatment for patients with cN1 thyroid cancer [3]. Radioactive iodine (RAI) therapy is selectively recommended by the ATA in intermediate-risk DTC after TT, including cN1 cases or those with more than 5 pathologic N1 (pN1) with all involved LNs <3 cm in the largest dimension [3], as well as in patients with several clinicopathologic factors including neck LN metastases according to the NCCN guidelines [4]. However, the long-term results of prophylactic CND (PCND) in patients with cN0 PTC are unclear, especially in those with pathologically proven neck node metastasis (pN1) after PCND. In addition, the necessity of completion thyroidectomy in patients with pN1 staging after PCND to allow for efficient RAI therapy is controversial.
Recent studies have investigated the utility of PCND in patients with cN0 PTC [78] and reported inconsistent results. A meta-analysis showed that PCND reduced the locoregional recurrence rate in patients with PTC but increased the postoperative RAI ablation rate and the occurrence of hypocalcemia [9]. In contrast, another meta-analysis showed no significant differences in recurrence and long-term complications regardless of PCND [10]. Ryu et al. [11] investigated the risk factors for recurrence in cN0 PTC patients who underwent TT plus bilateral CND and were verified to have pN1a disease. They found that gross ETE and nodal factors such as LN ratio >0.5 and 3 or more positive LNs were predictive of recurrence. Previous studies have attempted to determine the rationality of PCND in patients with cN0 PTC; however, studies on whether unilateral thyroid lobectomy or TT should be performed according to the results of PCND are limited. Moreover, long-term follow-up results with or without completion thyroidectomy in patients with pN1 staging after PCND are lacking.
Our study aimed to investigate whether the extent of thyroid surgery influences the prognosis of patients with PTC with central LN metastasis (N1a), which is cN0 but pathologically confirmed after PCND.
From April 2004 to June 2019, the medical records of 2,274 patients who underwent thyroid surgery with PCND for the treatment of cN0 PTC at Daegu Catholic University Hospital were reviewed. Of these, patients who were confirmed to have pN1a disease after PCND were identified for inclusion in this study. Patients who had evidence of central neck LN metastases on preoperative neck ultrasound (US) or neck CT, those who underwent completion thyroidectomy because of the recurrence of PTC within 6 months after the first surgery, and those who underwent sampling of lateral neck LNs and were found to have lateral neck LN metastases were excluded. Clinicopathologic characteristics including age, sex, tumor size, multiplicity, bilaterality, minimal ETE, number of metastatic LNs, removed LNs, postoperative RAI ablation, and tumor recurrence were evaluated. The LN ratio was defined as the number of metastatic LNs divided by the number of removed LNs.
Ethical approval for the study was obtained from the Institutional Review Board (IRB) of Daegu Catholic University Hospital (CR-20-040). The written informed consent from the patients was waived from the IRB according to the deliberation criteria.
The included patients underwent thyroidectomy (TT or less than TT [unilateral lobectomy or isthmusectomy]). The extent of thyroid surgery was preoperatively determined on the basis of preoperative staging, tumor size, bilaterality, multifocality, and patient's preference. During surgery, conversion from less than TT to TT was performed at the surgeon's decision according to the status of LN metastasis and intraoperative findings.
PCND refers to the removal of neck LNs at level VI including the Delphian (prelaryngeal), pretracheal, paraesophageal, and paratracheal nodes. Bilateral PCND was performed in patients who underwent TT, and ipsilateral PCND was performed in patients who underwent less than TT. All patients who underwent TT also underwent postoperative thyroid remnant ablation with 30–150 mCi of RAI, except for those who refused RAI therapy. Patients who underwent less than TT were not eligible for postoperative RAI ablation.
Postoperative follow-up was performed at intervals of 3–6 months for the first postoperative year and 6 months–1 year thereafter. During the follow-up, all patients underwent routine physical examination, neck US, chest radiography, and measurement of serum thyroglobulin (Tg) and anti-Tg antibody at each visit. We defined tumor recurrence as structural neck recurrence that was confirmed with cytology or biopsy, or distant metastatic disease found in imaging studies with elevated serum Tg level. Biochemical incomplete response was defined as follows: nonstimulated Tg of >1 ng/mL or thyroidstimulating hormone-stimulated Tg of >10 ng/mL in patients treated with TT and RAI ablation [3].
Statistical analysis was performed using IBM SPSS Statistics ver. 19.0 (IBM Corp., Armonk, NY, USA). For statistical analysis, the chi-square test or Fisher exact test was used to compare categorical variables. To analyze continuous data, Student t-test or the nonparametric Mann-Whitney U-test was used. Cox proportional hazard model and multivariate logistic regression were used to analyze the association between the clinicopathologic factors and recurrence-free survival (RFS). Kaplan-Meier curve analysis with the log-rank test was used to compare RFS according to the extent of thyroid surgery and other predictive factors. A P-value of <0.05 was considered to indicate statistical significance.
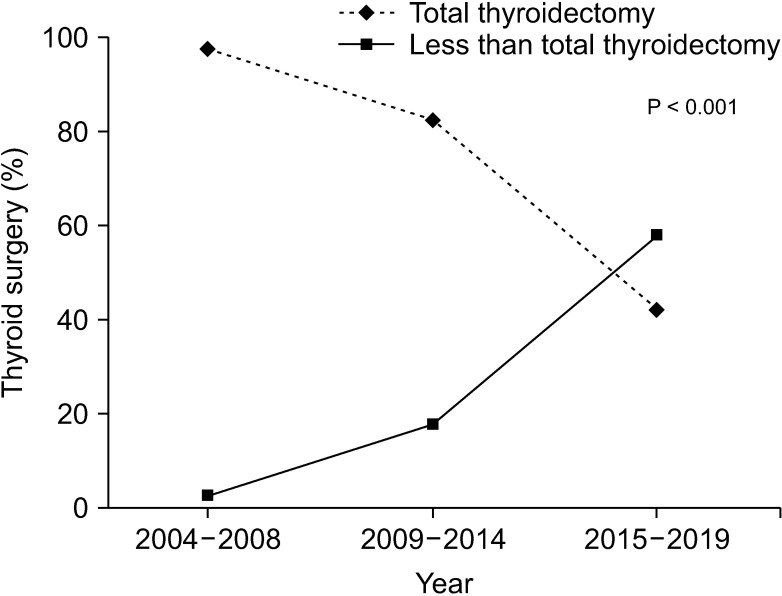
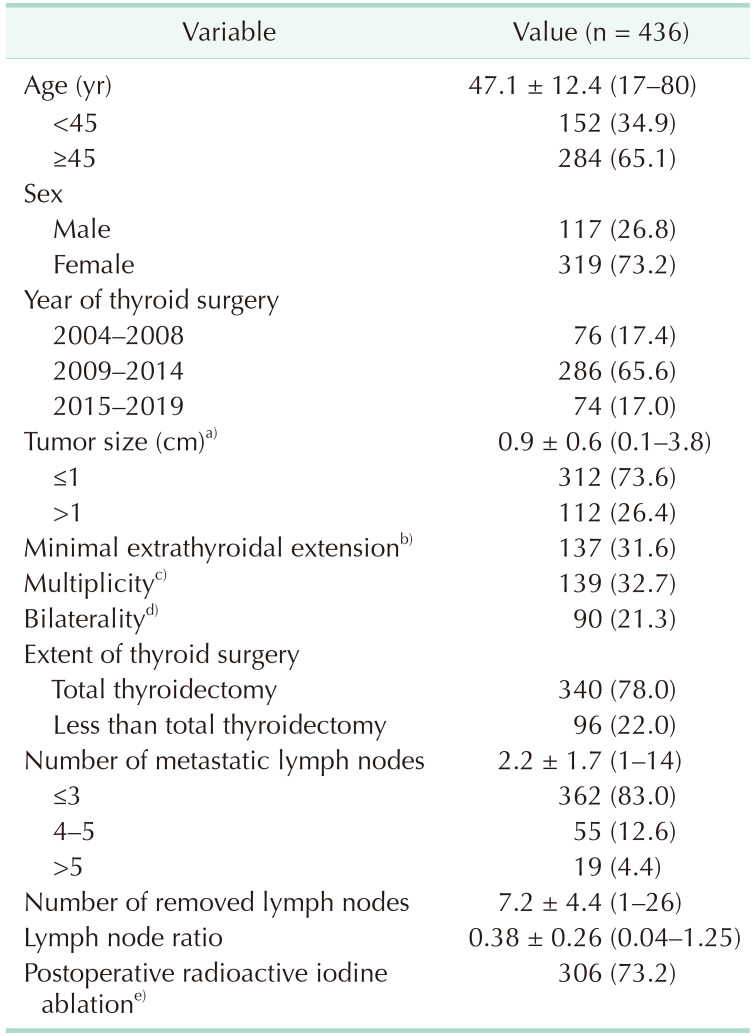
Of the total of 2,274 patients with cN0 PTC, 436 patients were confirmed to have pN1a disease after PCND. The patient characteristics are presented in Table 1. The average patient age was 47.1 ± 12.4 years (range, 17–80 years). Of the patients, 340 (78.0%) underwent TT and 96 (22.0%) underwent less than TT. The mean tumor size was 0.98 ± 0.6 cm, and 312 patients (73.6%) had papillary thyroid microcarcinoma. Among the 436 patients, the mean number or metastatic LNs was 2.2 ± 1.7 and 362 patients (83.0%) had fewer than 3 cervical LN metastases in the central neck compartment. When comparing the extent of thyroid surgery according to the year of surgery, the proportion of less than TT increased over time (Fig. 1). The median followup time (range) was 71 (6–186) months. Not surprisingly, the median follow-up period was longer in patients who underwent TT than in those who underwent less than TT regardless of RAI ablation (77 [range, 6–186] months and 37 [range, 6–135] months, respectively; P < 0.001).
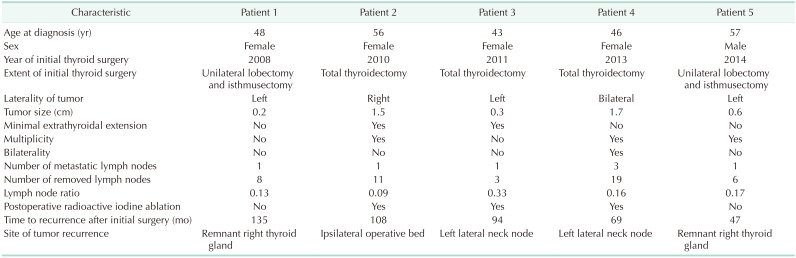
Of the 374 patients who were followed for >6 months, recurrence occurred in 5 patients (1.3%). The sites of recurrence were the remnant thyroid gland in 2 patients, lateral neck LNs in 2 patients, and ipsilateral operative bed in one patient (Table 2). None of the followed up patients had a biochemical incomplete response. Even in patients with structural recurrence, the nonstimulated Tg values were <1 ng/mL. None of the patients had distant metastasis. The 15-year RFS rate was 98.2%.
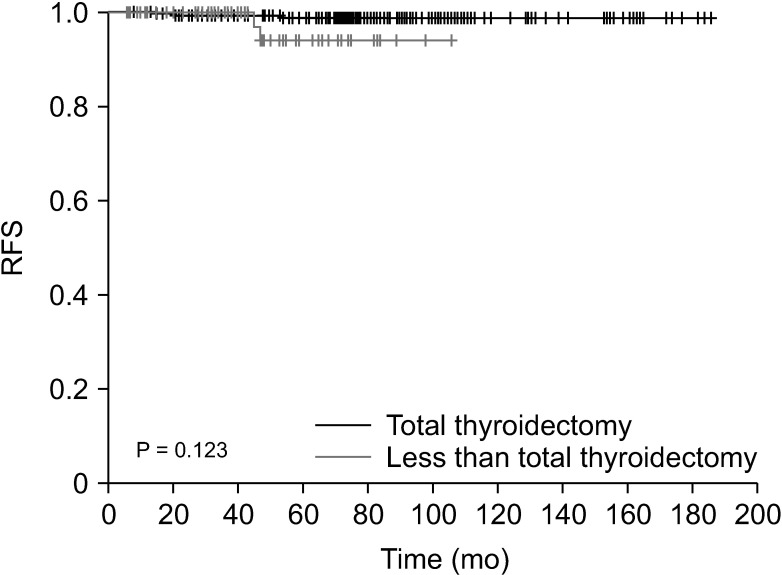
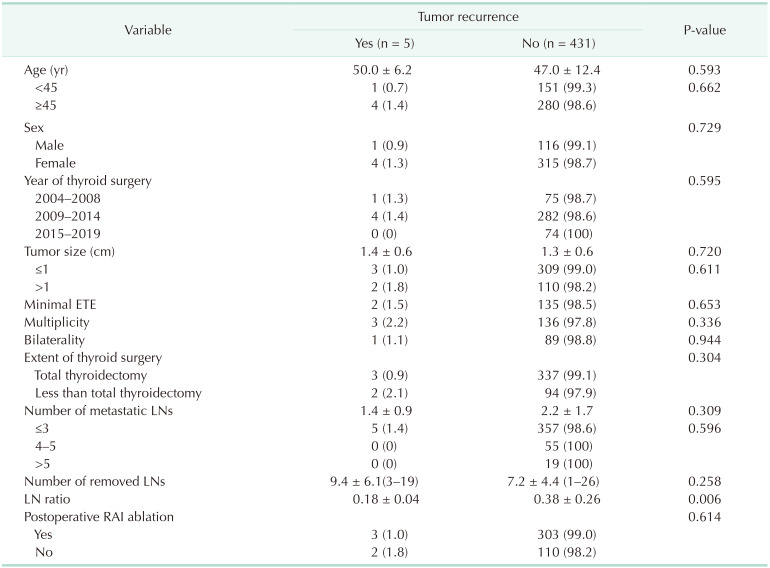
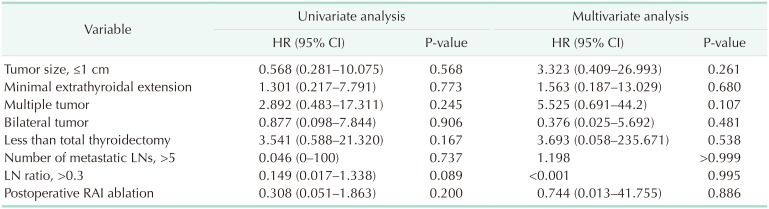
The LN ratio was significantly associated with tumor recurrence (P = 0.006), and the LN ratio in patients with recurrence was lower than that in patients without recurrence (0.18 ± 0.04 and 0.38 ± 0.26, respectively). No other factors were associated with tumor recurrence in patients with cN0 PTC pathologically confirmed as N1a after PCND (Table 3). No significant difference in tumor recurrence rates was observed between the less than TT group and the TT group. The RFS tended to be lower in patients who underwent less than TT than in those who underwent TT; however, the difference was not statistically significant (Fig. 2).
Univariate analysis using the Cox proportional hazard model showed no clinicopathologic factors predictive of tumor recurrence (Table 4). The hazard ratio (HR) of multiple tumors and less than TT seemed to be increased (HR [95% confidence interval]: 2.892 [0.483–17.311] and 3.541 [0.588–21.320], respectively); however, no statistical significance was found (P = 0.245 and P = 0.167, respectively). Further, no significant factor predicting tumor recurrence was identified in multivariate logistic regression analysis.
In this study, we investigated the tumor recurrence and RFS rates according to the extent of thyroid surgery in patients with cN0 PTC who underwent TT or less than TT plus PCND and were confirmed to have pN1a disease. No significant differences in tumor recurrence and RFS rates were found between the less than TT and TT groups even with a pathologic staging of N1a after PCND. Most previous studies investigating the effects of PCND included only patients with cN0 PTC undergoing TT. Therefore, no previous study has compared the outcomes between TT and thyroid lobectomy in patients with cN0 PTC and pN1a after PCND. Several studies evaluated disease-free survival (DFS) depending on the surgical extent of thyroidectomy regardless of clinical neck node metastasis. In a recent study comparing DFS in patients with PTC after 1:1 propensity score matching by age, sex, tumor size, ETE, multifocality, and neck LN metastasis, no significant difference in DFS was observed between a TT group and a thyroid lobectomy group [12]. In addition, lobectomy was not associated with an increased risk of structural persistent/recurrent disease [12]. Consistent with a previous study [12], our results support the feasibility of unilateral thyroid lobectomy without completion thyroidectomy for the treatment of cN0 unilateral PTC even if neck LN metastasis is confirmed after PCND.
The presence of neck LN metastases in patients with PTC has been reported to be associated with compromised survival and a higher recurrence rate that ranges from 3% to 32% compared with the absence of neck LN metastasis [3561314]. Postoperative RAI ablation has been used to eliminate postsurgical remnant thyroid tissue to decrease the risk of recurrence and to facilitate the early detection of recurrence and initial staging by identifying previously undiagnosed disease [215]. In this regard, the 2009 ATA guidelines recommended RAI ablation for selected patients with 1–4 cm thyroid cancers confined to the thyroid, those with documented LN metastases, or those with other high-risk factors for recurrence or death from thyroid cancer [2]. Thereby, completion thyroidectomy was necessary for those patients to allow RAI therapy. However, there has been little evidence on the impact of RAI in low-risk DTC cases and the indications of RAI ablation are becoming more selective [1617]. In the 2015 ATA guidelines, the initial risk stratification system for DTC was modified and an LN status of no clinical LN metastasis or 5 or fewer pN1 micrometastases (defined as <0.2 cm in the largest dimension) was classified as a low-risk factor [3]. The tumor recurrence rate of cN0 PTC patients was relatively low, ranging from 0% to 9% [1819], whereas those of cN0 PTC and pN1 (identified only by PCND) patients ranged from 4% to 11.5% [111819]. Likewise, the tumor recurrence rate in our study was as low as 1.3%. Considering the low recurrence rate, postoperative RAI may not be routinely recommended for cN0 PTC patients, even with pathologically confirmed LN metastasis after PCND. Further, it is not necessary to perform TT to allow postoperative RAI in cN0 low-risk PTC.
Although the surgical treatment of low- to intermediate-risk DTCs is evolving into a more conservative approach, the extent of thyroid surgery for PTC is still a matter of debate. It is controversial whether to perform TT or thyroid lobectomy for the treatment of cN0 PTC ≤4 cm, and whether or not to perform completion thyroidectomy when subclinical LN metastasis is confirmed after the initial surgery in patients with cN0 PTC. Several studies analyzing large-scale databases failed to demonstrate a significant difference in survival between patients who underwent TT and those who underwent thyroidectomy [20212223]. Recently, Song et al. [12] showed similar DFS between TT and thyroid lobectomy in patients with 1–4 cm PTC after controlling for major prognostic factors. In contrast, a recent retrospective study using the National Cancer Database showed improved survival in patients who underwent TT compared with those who underwent thyroid lobectomy for 2.0–3.9 cm PTC, but not for 1.0–1.9 cm tumors [24]. In addition to DFS, postoperative complications are one of the factors to consider when determining the extent of thyroidectomy because of the increased risk of complications in TT compared with thyroid lobectomy [25]. Our study also found no significant difference in tumor recurrence and RFS rates according to the surgical extent. Our results support the feasibility of thyroid lobectomy as the initial surgical procedure in patients with cN0 unilateral PTC.
Although routine PCND has been controversial, the extent of thyroidectomy when LN metastasis is identified in PCND is also debated. Central neck LN metastases have been reported to exist in the range of 16.7% to 82.3% at the time of diagnosis in patients with PTC undergoing PCND [2627]. Therapeutic LN dissection for the treatment of cN1 PTC is well accepted [351428]. However, preoperative detection of metastatic LNs in the central neck compartment is somewhat difficult and there are limitations in the diagnosis of central neck LN metastasis using preoperative neck US or CT [27]. In this regard, PCND can help assess the neck LN status and make decisions about RAI therapy [11]. While routine PCND remains debated, whether or not to perform completion thyroidectomy when LN metastases are identified after PCND is another concern for thyroid surgeons. In a recent study, it was suggested that frozen section examination in PCND for cT1N0 unifocal PTC can be useful to intraoperatively assess the LN status; if occult LN metastasis occurs, TT and CND become mandatory [29]. In another study, the authors proposed indications for thyroid lobectomy for DTCs based on a review of the impact of various clinicopathologic features on structural recurrence or survival [30]. They suggested that a more conservative management approach may be a reasonable alternative to immediate completion of thyroidectomy in cN0 DTCs even with metastatic LNs according to LN-related variables [30]. In our study, all included patients had LN metastasis, but the tumor recurrence rate was low and there were no significant differences in the tumor recurrence and RFS rates between TT and less than TT. To our knowledge, this is the first study to compare the outcomes of TT and thyroid lobectomy in patients with cN0 PTC and pN1a after PCND. Considering the low recurrence rate and the surgical morbidity associated with thyroid surgery, our results showed the feasibility of thyroid lobectomy without immediate completion thyroidectomy in cN0 PTC patients undergoing PCND and with verified neck LN metastasis after PCND.
This study had several limitations. First, this was a retrospective study and the postoperative complications could not be adequately assessed. In addition, there were limitations to the available dataset from our retrospective cohort. Second, because the number of recurrent cases was small, the reliability of the statistical analysis may be diminished by the division of patients into the recurrent and nonrecurrent groups. Third, the follow-up period was relatively short to confirm recurrence in some patients. In particular, the median follow-up period was shorter in patients who underwent less than TT than in those who underwent TT. The relatively short follow-up period of <5 years may have affected the RFS of patients who underwent less than TT. Further prospective, multi-institutional clinical trials are needed to define the rationality of thyroid lobectomy in cN0 unilateral PTC and to identify predictors that will help determine the extent of thyroid surgery.
In conclusion, our study showed low recurrence rates in patients with cN0 PTC pathologically confirmed as N1a after PCND. No difference in RFS according to the extent of thyroid surgery was found. Less than TT with PCND may be considered as the initial treatment for patients with cN0 unilateral PTC even with a pathologic staging of N1a after PCND. Furthermore, with respect to substantial LN involvement in PTC and surgical removal of all structural disease, PCND in cN0 PTC can be a useful and reasonable procedure.
References
1. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2006; 16:109–142. PMID: 16420177.
2. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty , GM , Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214. PMID: 19860577.
3. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; 26:1–133. PMID: 26462967.
4. Haddad RI, Bischoff L, Busaidy NL, Dickson P, Duh QY, Ehya H, et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) for thyroid carcinoma, version 2.2019. Fort Washington, PA: National Comprehensive Cancer Network, Inc.;2019.
5. Amit M, Tam S, Boonsripitayanon M, Cabanillas ME, Busaidy NL, Grubbs EG, et al. Association of lymph node density with survival of patients with papillary thyroid cancer. JAMA Otolaryngol Head Neck Surg. 2018; 144:108–114. PMID: 29192312.
6. Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, et al. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 2012; 22:1144–1152. PMID: 23083442.
7. Dobrinja C, Troian M, Cipolat Mis T, Rebez G, Bernardi S, Fabris B, et al. Rationality in prophylactic central neck dissection in clinically node-negative (cN0) papillary thyroid carcinoma: is there anything more to say? A decade experience in a single-center. Int J Surg. 2017; 41 Suppl 1:S40–S47. PMID: 28506412.
8. Ywata de Carvalho A, Chulam TC, Kowalski LP. Long-term results of observation vs prophylactic selective level VI neck dissection for papillary thyroid carcinoma at a cancer center. JAMA Otolaryngol Head Neck Surg. 2015; 141:599–606. PMID: 25997016.
9. Zhao W, You L, Hou X, Chen S, Ren X, Chen G, et al. The effect of prophylactic central neck dissection on locoregional recurrence in papillary thyroid cancer after total thyroidectomy: a systematic review and meta-analysis: pCND for the locoregional recurrence of papillary thyroid cancer. Ann Surg Oncol. 2017; 24:2189–2198. PMID: 27913945.
10. Wang TS, Cheung K, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of the effect of prophylactic central compartment neck dissection on locoregional recurrence rates in patients with papillary thyroid cancer. Ann Surg Oncol. 2013; 20:3477–3483. PMID: 23846784.
11. Ryu YJ, Cho JS, Park MH, Yoon JH. Identifying risk factors of recurrence for clinically node negative papillary thyroid carcinoma with pathologic N1a. BMC Surg. 2019; 19:78. PMID: 31277631.
12. Song E, Han M, Oh HS, Kim WW, Jeon MJ, Lee YM, et al. Lobectomy is feasible for 1-4 cm papillary thyroid carcinomas: a 10-year propensity score matched-pair analysis on recurrence. Thyroid. 2019; 29:64–70. PMID: 30375260.
13. Adam MA, Pura J, Goffredo P, Dinan MA, Reed SD, Scheri RP, et al. Presence and number of lymph node metastases are associated with compromised survival for patients younger than age 45 years with papillary thyroid cancer. J Clin Oncol. 2015; 33:2370–2375. PMID: 26077238.
14. Podnos YD, Smith D, Wagman LD, Ellenhorn JD. The implication of lymph node metastasis on survival in patients with well-differentiated thyroid cancer. Am Surg. 2005; 71:731–734. PMID: 16468507.
15. Choudhury PS, Gupta M. Differentiated thyroid cancer theranostics: radioiodine and beyond. Br J Radiol. 2018; 91:20180136. PMID: 30260232.
16. Schvartz C, Bonnetain F, Dabakuyo S, Gauthier M, Cueff A, Fieffé S, et al. Impact on overall survival of radioactive iodine in low-risk differentiated thyroid cancer patients. J Clin Endocrinol Metab. 2012; 97:1526–1535. PMID: 22344193.
17. Lamartina L, Durante C, Filetti S, Cooper DS. Low-risk differentiated thyroid cancer and radioiodine remnant ablation: a systematic review of the literature. J Clin Endocrinol Metab. 2015; 100:1748–1761. PMID: 25679996.
18. Wada N, Duh QY, Sugino K, Iwasaki H, Kameyama K, Mimura T, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg. 2003; 237:399–407. PMID: 12616125.
19. Cranshaw IM, Carnaille B. Micrometastases in thyroid cancer. An important finding? Surg Oncol. 2008; 17:253–258. PMID: 18504121.
20. Haigh PI, Urbach DR, Rotstein LE. Extent of thyroidectomy is not a major determinant of survival in low- or high-risk papillary thyroid cancer. Ann Surg Oncol. 2005; 12:81–89. PMID: 15827782.
21. Mendelsohn AH, Elashoff DA, Abemayor E, St John MA. Surgery for papillary thyroid carcinoma: is lobectomy enough? Arch Otolaryngol Head Neck Surg. 2010; 136:1055–1061. PMID: 21079156.
22. Barney BM, Hitchcock YJ, Sharma P, Shrieve DC, Tward JD. Overall and cause-specific survival for patients undergoing lobectomy, near-total, or total thyroidectomy for differentiated thyroid cancer. Head Neck. 2011; 33:645–649. PMID: 20687168.
23. Adam MA, Pura J, Gu L, Dinan MA, Tyler DS, Reed SD, et al. Extent of surgery for papillary thyroid cancer is not associated with survival: an analysis of 61,775 patients. Ann Surg. 2014; 260:601–605. PMID: 25203876.
24. Rajjoub SR, Yan H, Calcatera NA, Kuchta K, Wang CE, Lutfi W, et al. Thyroid lobectomy is not sufficient for T2 papillary thyroid cancers. Surgery. 2018; 163:1134–1143. PMID: 29426618.
25. Hauch A, Al-Qurayshi Z, Randolph G, Kandil E. Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann Surg Oncol. 2014; 21:3844–3852. PMID: 24943236.
26. Liang J, Li Z, Fang F, Yu T, Li S. Is prophylactic central neck dissection necessary for cN0 differentiated thyroid cancer patients at initial treatment? A meta-analysis of the literature. Acta Otorhinolaryngol Ital. 2017; 37:1–8. PMID: 28374865.
27. Ahn JE, Lee JH, Yi JS, Shong YK, Hong SJ, Lee DH, et al. Diagnostic accuracy of CT and ultrasonography for evaluating metastatic cervical lymph nodes in patients with thyroid cancer. World J Surg. 2008; 32:1552–1558. PMID: 18408961.
28. Lang BH, Wong KP, Wan KY, Lo CY. Impact of routine unilateral central neck dissection on preablative and postablative stimulated thyroglobulin levels after total thyroidectomy in papillary thyroid carcinoma. Ann Surg Oncol. 2012; 19:60–67. PMID: 21681379.
29. Raffaelli M, Tempera SE, Sessa L, Lombardi CP, De Crea C, Bellantone R. Total thyroidectomy versus thyroid lobectomy in the treatment of papillary carcinoma. Gland Surg. 2020; 9(Suppl 1):S18–S27. PMID: 32055495.
30. Park JH, Yoon JH. Lobectomy in patients with differentiated thyroid cancer: indications and follow-up. Endocr Relat Cancer. 2019; 26:R381–R393. PMID: 31018176.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download