Abstract
Purpose
The objective of the current study was to examine the potential effects of surgery start times (morning vs. afternoon) on the long-term prognosis of patients after hepatic resection (HR) for hepatocellular carcinoma (HCC).
Methods
All eligible patients were divided into 2 groups according to the start time of surgery: group M (morning surgery, 8 AM–1 PM) and group A (afternoon surgery, 1 PM–6 PM). Clinicopathologic and surgical parameters, as well as oncologic outcomes were compared between the 2 groups.
Results
In total, 231 patients were included in the study. There was no difference in age, body mass index, comorbidities, tumor size, tumor location, tumor stages, surgical procedures, or surgical margin between morning and afternoon surgery (all P > 0.05). In contrast, patients in group M experienced longer operation duration than those in group A (median, 240 minutes vs. 195 minutes, P = 0.004). However, no differences of overall survival were observed between morning and afternoon surgery groups in the whole cohort or stratified by surgical margin (all P > 0.05).
Curative resection remains the optimal treatment for hepatocellular carcinoma (HCC), although ablation and liver transplant are indicated for early staged disease [12]. However, the prognosis of HCC after curative hepatic resection (HR) is dismal. Typically, the long-term outcome of cancer after curative surgery is determined mostly by tumor characteristics, e.g., size, number, location, vascular invasion, etc. as well as surgical procedures, e.g., margin, ischemia/reperfusion injury, resection type, blood loss, and transfusion, etc. [34]. Few studies have discussed possible impacts of judgment bias and inaccurate performance of surgeons secondary to progressive fatigue on patient outcomes [5].
Long work hours are considered a tradition among surgeons [67]. Undoubtedly, human performance is adversely affected by sleep deficit, circadian rhythm disruption, and long work hours, leading to decrements in cognitive and psychomotor performance and increased risk of accidents [8]. Prolonged duty hours and sleep deprivation have been associated with increased medical errors among interns [910111213]. For example, even during work days, adenoma detection rate was significantly higher in morning colonoscopies than in afternoon colonoscopies [141516]. Patients anesthetized at different time of the day may have different clinical outcomes [17].
However, some other studies found that sleep deprivation before surgery, or surgery start times during working hours did not measurably affect the short-term outcomes of the patients [18192021].
As a complex and high-risk procedure, HR is susceptible to the surgeon's mood, cognitive performance, and psychomotor function. Progressive fatigue caused by sustained work may impair the attention, judgment, and performance accuracy of surgeons, which would lead to adverse clinical outcomes [22]. No study has investigated the potential influence of surgery start times on long-term outcome of patients undergoing HR for HCC. The objective of the current study aimed to examine the effects of surgery start time on oncologic outcomes of HCC after curative HR.
Patients undergoing HR with curative-intent for HCC between January 2012 and September 2015 in our university hospital were included. Patients undergoing palliative surgery (R2), radiofrequency, laparoscopic, or emergency surgery were excluded from the current study. Patients who died within 90 days after surgery were also excluded. The study was approved by the ethics committee of the First Affiliated Hospital, Xi'an Jiaotong University (No. XJTU1AF2017LSL-007) on the premise of obtaining the voluntary informed consent of enrolled patients, the rules of which comply with the Treaty of Helsinki. A waiver of informed consent was obtained, since the data were analyzed from the electronic medical records and reported without personal identifiers.
The clinicopathological data of patients were identified from a prospectively maintained database, including age, gender, body mass index, HBV or HCV status, comorbidities, and preoperative biochemical tests. Tumor size, number and location, and surgical margin were collected from the pathological reports. Surgical procedures, duration, and intraoperative blood loss and transfusion were recorded based on operation and anesthesia reports. Tumor stage was categorized according to the 8th edition of the American Joint Committee on Cancer [23] and Barcelona Clinic Liver Cancer (BCLC) [24] stages.
Diagnosis of HCC was established by characteristic features on CT, MRI or hepatic arteriography, and/or a serum α-FP level greater than 400 ng/mL. HR was offered by assessment of resectability based on tumor size, number, and liver functional reserve. Liver function status was assessed by liver biochemistry status, indocyanine green retention test for 15 minutes, and Child-Pugh classification.
All the resection procedures were performed by senior surgeons with at least 10-year experience in liver surgery. All HR on work days started between 8 AM to 6 PM. The beginning of the surgery was defined as start of skin incision. As such, patients were classified as morning surgery (started between 8 AM and 1 PM, group M) and afternoon (started after 1 PM, group A) surgery groups. One PM was generally the time when most surgeons transitioned from the previous to the current major cases, and thus allowed for comparisons of fatigue, focus, mental concentration between morning and afternoon surgeries. All the surgeries were allocated to a scheduled time the day before operation by the surgery department.
The type and extent of HR were defined according to the Brisbane 2000 Terminology of Liver Anatomy & Resections [25]. Major HR was defined as resection of 3 or more liver segments, while minor resection was defined as removal of 2 or fewer segments. Hepatic inflow occlusion was performed when deemed indicated by the operating surgeon in order to reduce intraoperative blood loss. Intermittent hepatic inflow occlusion using cycles of 15-minute ischemia followed by 10 minutes of reperfusion was the preferred regimen. All the procedures were mainly accomplished by senior surgeons with surgical experience of more than 10 years.
All the patients were routinely followed in the Outpatient Department or by telephone interview. Patients were regularly followed after surgery with α-FP, and abdominal CT or MRI scanning. Overall survival (OS) was calculated from the date of surgery.
Continuous variables are expressed as median and interquartile range (IQR) and compared with Student t-test or the Mann-Whitney U-test. Categorical variables are expressed as numbers and percentages, and compared with the chi-square test or Fisher exact test. OS was estimated by the Kaplan-Meier method and the log rank test was used to compare differences between different groups. A P-value of <0.05 was considered statistically significant. Statistical analysis was carried out using IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA).
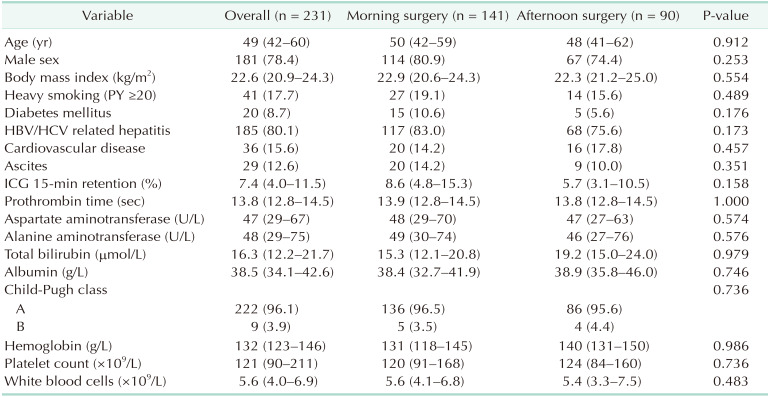
In total, 231 patients were included in the study. Among them, 141 patients underwent morning surgery (8 AM–1 PM, group M), while 90 patients underwent afternoon surgery (1 PM–6 PM, group A). The clinical data of the patients were summarized in Table 1. The median age was 49 years (IQR, 42–60 years). The majority of patients were male (n = 181, 78.4%), and HBV or HCV positive (n = 185, 80.1%). Liver function of Child-Pugh class A was found in 96.1% of patients.
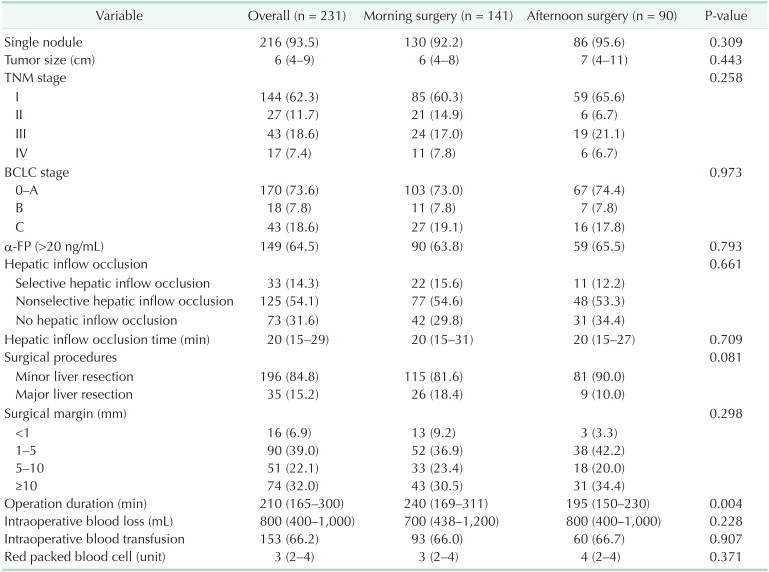
The tumor and surgery associated information was summarized in Table 2. Most patients had a single tumor (n = 216, 93.5%). The median tumor size was 6 cm (IQR, 4–9 cm). Hepatic inflow (selective or nonselective) was a routine procedure performed in about 2/3 of patients during surgery (n = 158, 68.4%). The duration of hepatic inflow occlusion was about 20 minutes (IQR, 15–29 minutes). The median operation time was 210 minutes (IQR, 165–300 minutes). Based on the final pathology report, 74 patients (32.0%) had a wide surgical margin (≥10 mm), 141 patients (61.1%) had a narrow surgical margin (1–10 mm), while 16 patients (6.9%) had microscopically positive margin (<1 mm).
Patients subjected to afternoon surgery were not different from patients undergoing morning surgery in demographic characteristics, comorbidities, preoperative liver function, tumor size, and number, as well as the TNM and BCLC stages (Tables 1, 2). Interestingly, patients who underwent morning surgery were more likely to experience major resection (morning 18.4% vs. afternoon 10.0%, P = 0.081) and thus longer surgery time (median, morning 240 minutes vs. afternoon 195 minutes, P = 0.004). However, the final surgical margin status, intraoperative blood loss, and blood transfusion were not different between morning and afternoon surgery groups (all P > 0.05).
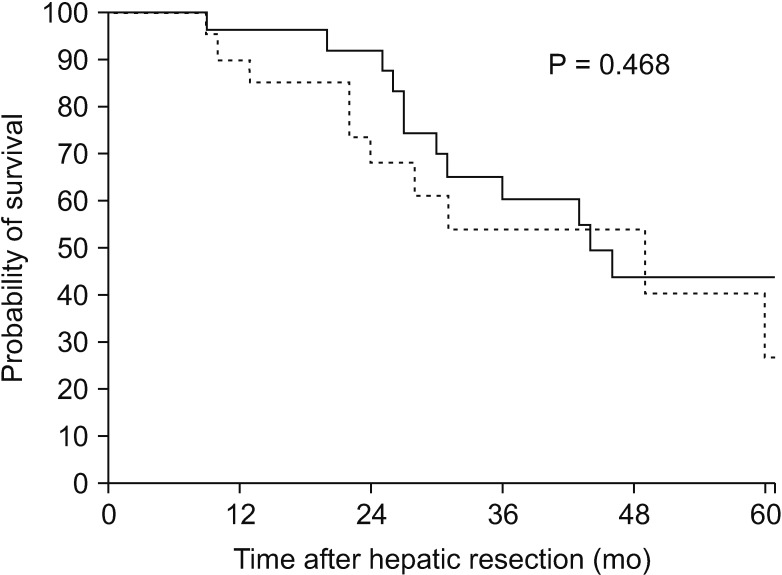
The median, 1-, 3-, and 5-year OS were 45 months, 91%, 78%, and 26% for patients undergoing morning surgery, and 48 months, 93%, 88% and 37% for patients undergoing afternoon surgery (P = 0.351) (Fig. 1), respectively. A further subanalysis was performed depending on the surgical margin and surgery start times. Consistently, patients undergoing morning surgery had equivalent OS versus those undergoing afternoon surgery either in narrow surgical margin group (1–10 mm, median OS, morning surgery 43 months vs. afternoon surgery 44 months, P = 0.319) (Fig. 2) or wide surgical margin group (≥10 mm, median OS, morning surgery 44 months vs. afternoon surgery 52 months, P = 0.468) (Fig. 3).
Overload of work and subsequent progressive fatigue of physicians may lead to increased medical errors or accidents among interns or junior physicians [8910111213]. The reason for decreased efficiency of medical performance may include: (1) Afternoon fatigue. Evidence suggests that fatigue impairs human performance and many physicians work from early in the morning to late in the day. (2) Afternoon circadian lows. The natural circadian rhythm which regulates sleep-wake cycle, cognitive performance, and other physiological functions go down in the afternoon, which may make it harder for medical professionals to maintain performance levels [8]. (3) Work shift in the afternoon. Anesthetists and nurses often change shifts in the afternoon, which might cause information loss or neglect. However, other studies have shown that sleep deprivation, or progressive fatigue during the work day did not increase the postoperative morbidity of the patients [18192021]. It is likely that in medical professional disciplines, physicians can adjust their work schedule, collaborate within teams, and regulate clinical procedures, with an endeavor to minimize adverse events caused by nontechnical factors [18].
Although surgery start time may not measurably affect the postoperative morbidity of patients due to self-regulation and wellness control by surgeons, it remains unclear whether the progressive fatigue of surgeons during a normal working day can significantly weaken their judgment and performance in surgery. The present study is important, as it is the first to investigate the long-term prognosis of HCC following morning versus afternoon HR. The patient characteristics, tumor feature, and surgical procedures were not significantly different between morning and afternoon surgery groups. Of note, the long-term prognosis was equivalent regardless of surgery start times.
In fact, the duration of operations beginning in the morning was longer than those performed in the afternoon in the current study (Table 2). Actually, major resection seemed to be more frequently performed in the morning than afternoon (18.4% vs. 10.0%, Table 2) and, generally, it seems true that complex operations are more likely arranged in the morning. As analyzed, patient demographics, liver function, and tumor characteristics were similar among patients undergoing morning versus afternoon surgery. This implied a relatively random assignment of patients to the day surgery. In fact, assignment of surgery is mostly determined by the operation and anesthesia department in our hospital, and each surgical team has 1 to 2 “normal operation days” due to limitation of operation rooms, which means their surgery can start at 8 AM. in the morning on these days. Therefore, most surgeons would like to arrange more complicated and difficult surgeries on “normal operation days.” It is not surprising that surgeons in the morning are more energetic, and have enough time to finish the operation during the daytime. However, as we noticed, the surgical margin, intraoperative blood loss, and transfusion, which might be more likely affected by progressive fatigue and subsequent inaccurate surgical performance of surgeons, were not different among patients undergoing morning versus afternoon surgery. As such, the OS was equivalent after morning versus afternoon surgery. These findings indicated that surgery start time had no significant influence on physician judgment, productivity, or performance, and therefore had no adverse oncological impacts on patients even when the operation was performed in the afternoon.
HR is a complex and high-risk surgery, and was mostly performed by experienced surgeons after at least 10-year professional training [26]. Experienced surgeons were unlikely to be affected by progressive fatigue when performing operations during a normal work day, as they are more self-regulated and adapted to this situation. Similarly, Slaughter et al. [27] reported that there was no association between surgery start time and long-term prognosis of patients undergoing minimally invasive surgery for gynecologic cancer. The findings of our study supports continued use of the current surgical practice in liver surgery. However, with significant increases in caseloads, the physical health of the physicians should be of concern as well in order to improve the efficacy and efficiency of operations on patients.
There were several limitations of the current study. First, as a retrospective and single-center study, some inherent biases could not be identified or excluded. Second, the time cutoff differentiating morning versus afternoon surgery was somewhat depending on the regular working time of these surgeons (8 AM–6 PM). It is possible other categories of morning versus afternoon surgery may have identified different results. Additionally, disease-free survival was not available in the current study due to inaccurate reports of recurrence or shift to local hospitals. Therefore, OS was utilized as the primary end point.
In conclusion, patients undergoing curative-intent HR appear to have been rather randomly assigned to morning and afternoon surgery. Surgery start times (morning versus afternoon) had no measurable influence on the long-term prognosis of patients. Physicians performing afternoon surgery had no obvious deviation of their judgment or skill even with progressive fatigue, as surgical margin, intraoperative blood loss, and transfusion were not different between afternoon and morning surgery. However, these null findings do not exclude the possible impacts of excessive fatigue of physicians, such as after 24 hours on-call or after a night emergency operation, on the prognosis of patients undergoing regular daytime surgery.
ACKNOWLEDGEMENTS
This abstract has been presented at the 13th World Congress of the International Hepato-Pancreato-Biliary Association (PRESENTATION CODE: EP01B-011).
Notes
References
1. Bigourdan Jean-Marc, Jaeck Daniel, Meyer Nicolas, Meyer Carole, Oussoultzoglou Elie, Bachellier Philippe, et al. Small hepatocellular carcinoma in child A cirrhotic patients: hepatic resection versus transplantation. Liver Transpl. 2003; 9:513–520. PMID: 12740796.
2. Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996; 334:693–699. PMID: 8594428.
3. Zhou Li, Rui Jing-An, Wang Shao-Bin, Chen Shu-Guang, Qu Qiang. Early recu rrence in large hepatocellular carcinoma after curative hepatic resection: prog nostic significance and risk factors. Hepatogastroenterology. 2014; 61:2035–2041. PMID: 25713907.
4. Benzoni Enrico, Lorenzin Dario, Favero Alessandro, Adani Gianluigi, Baccarani Umberto, Molaro Roberta, et al. Liver resection for hepatocellular carcinoma: a multivariate analysis of factors associated with improved prognosis. The role of clinical, pathological and surgical related factors. Tumori. 2007; 93:264–268. PMID: 17679461.
5. Sturm Lana, Dawson Drew, Vaughan Richard, Hewett Peter, Hill Andrew G, Graham John C, et al. Effects of fatigue on surgeon performance and surgical outcomes: a systematic review. ANZ J Surg. 2011; 81:502–509. PMID: 22295360.
6. Strunk CL, Bailey BJ, Scott BA, Cummings CW, Lucente FE, Beatty CW, et al. Resident work hours and working environment in otolaryngology. Analysis of daily activity and resident perception. JAMA. 1991; 266:1371–1374. PMID: 1880867.
7. Whang EE, Perez A, Ito H, Mello MM, Ashley SW, Zinner MJ. Work hours reform: perceptions and desires of contemporary surgical residents. J Am Coll Surg. 2003; 197:624–630. PMID: 14522334.
8. Goel N, Basner M, Rao H, Dinges DF. Circadian rhythms, sleep deprivation, and human performance. Prog Mol Biol Transl Sci. 2013; 119:155–190. PMID: 23899598.
9. Landrigan CP, Rothschild JM, Cronin JW, Rainu Kaushal, Elisabeth Burdick, Joel T Katz, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004; 351:1838–1848. PMID: 15509817.
10. Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004; 351:1829–1837. PMID: 15509816.
11. Fisman DN, Harris AD, Rubin M, Sorock GS, Mittleman MA. Fatigue increases the risk of injury from sharp devices in medical trainees: results from a casecrossover study. Infect Control Hosp Epidemiol. 2007; 28:10–17. PMID: 17230382.
12. Barger LK, Ayas NT, Cade BE, Cronin JW, Rosner B, Speizer FE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006; 3:e487. PMID: 17194188.
13. Ayas NT, Barger LK, Cade BE, Hashimoto DM, Rosner B, Cronin JW, et al. Extended work duration and the risk of selfreported percutaneous injuries in interns. JAMA. 2006; 296:1055–1062. PMID: 16954484.
14. Sanaka MR, Shah N, Mullen KD, Ferguson DR, Thomas C, McCullough AJ. Afternoon colonoscopies have higher failure rates than morning colonoscopies. Am J Gastroenterol. 2006; 101:2726–2730. PMID: 17227519.
15. Gurudu SR, Ratuapli SK, Leighton JA, Heigh RI, Crowell MD. Adenoma detection rate is not influenced by the timing of colonoscopy when performed in half-day blocks. Am J Gastroenterol. 2011; 106:1466–1471. PMID: 21502998.
16. Teng TY, Khor SN, Kailasam M, Cheah WK, Lau CC. Morning colonoscopies are associated with improved adenoma detection rates. Surg Endosc. 2016; 30:1796–1803. PMID: 26198158.
17. Wright MC, Phillips-Bute B, Mark JB, Stafford-Smith M, Grichnik KP, Andregg BC, et al. Time of day effects on the incidence of anesthetic adverse events. Qual Saf Health Care. 2006; 15:258–263. PMID: 16885250.
18. Lu Q, Shen Y, Zhang J, Ren YF, Dong J, Du ZQ, et al. Operation start times and postoperative morbidity from liver resection: a propensity score matching analysis. World J Surg. 2017; 41:1100–1109. PMID: 27878349.
19. Ellman PI, Kron IL, Alvis JS, Tache-Leon C, Maxey TS, Reece TB, et al. Acute sleep deprivation in the thoracic surgical resident does not affect operative outcomes. Ann Thorac Surg. 2005; 80:60–64. PMID: 15975341.
20. Ellman PI, Law MG, Tache-Leon C, Reece TB, Maxey TS, Peeler BB, et al. Sleep eprivation does not affect operative results in cardiac surgery. Ann Thorac Surg. 2004; 78:906–911. PMID: 15337018.
21. Govindarajan A, Urbach DR, Kumar M, Li Q, Murray BJ, Juurlink D, et al. Outcomes of daytime procedures performed by attending surgeons after night work. N Engl J Med. 2015; 373:845–853. PMID: 26308685.
22. You DD, Kim DG, Seo CH, Choi HJ, Yoo YK, Park YG. Prognostic factors after curative resection hepatocellular carcinoma and the surgeon's role. Ann Surg Treat Res. 2017; 93:252–259. PMID: 29184878.
23. Amin MB, Edge SB. AJCC cancer staging manual. New York: Springer;2017.
24. Llovet JM, Brú C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999; 19:329–338. PMID: 10518312.
25. Pang YY. The Brisbane 2000 terminology of liver anatomy and resections. HPB 2000; 2:333–39. HPB (Oxford). 2002; 4:99. author reply 99–100. PMID: 18332933.
26. Kim JM, Yi NJ, Kwon CHD, Lee KW, Suh KS, Joh JW. Early disseminated recurrence after liver resection in solitary hepatocellular carcinoma. Ann Surg Treat Res. 2018; 94:129–134. PMID: 29520346.
27. Slaughter KN, Frumovitz M, Schmeler KM, Nick AM, Fleming ND, dos Reis R, et al. Minimally invasive surgery for endometrial cancer: does operative start time impact surgical and oncologic outcomes. Gynecol Oncol. 2014; 134:248–252. PMID: 24945591.
Fig. 1
Overall survival curves of patients undergoing morning surgery (solid line) and patients undergoing afternoon surgery (dotted line).
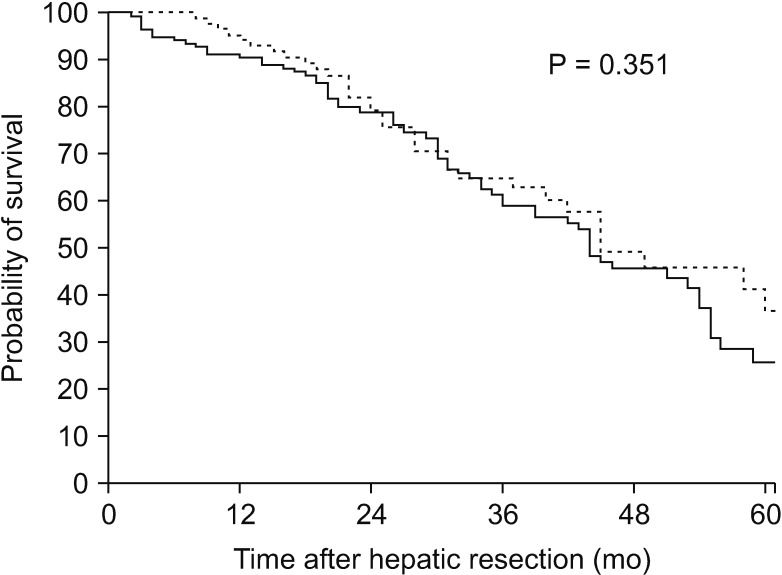
Fig. 2
Overall survival curves of patients undergoing morning surgery (solid line) and patients undergoing afternoon surgery (dotted line) with narrow surgical margin (1–10 mm).
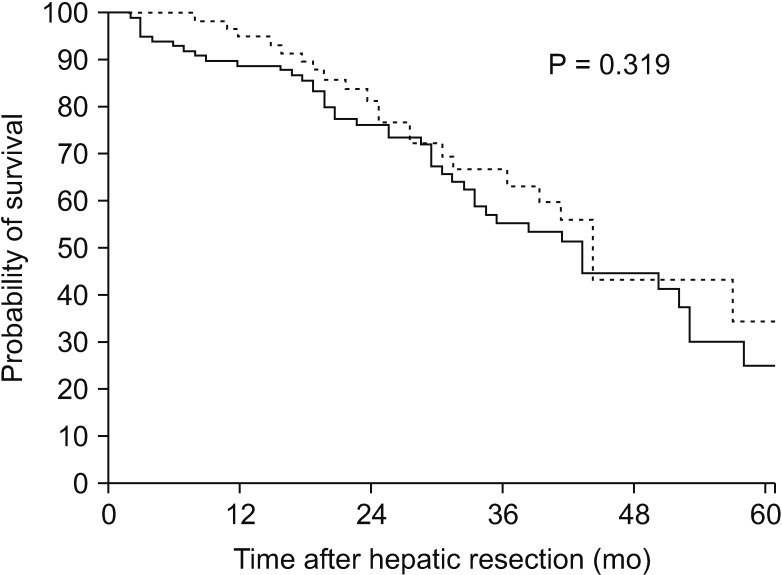
Fig. 3
Overall survival curves of patients undergoing morning surgery (solid line) and patients undergoing afternoon surgery (dotted line) with wide surgical margin (≥10 mm).




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download