Abstract
Purpose
Treatment of rectocele associated with prolapsed hemorrhoids is a debated topic. Transanal stapling achieved good midterm results in patients with symptoms of obstructed defecation, nevertheless a number of severe complications have been reported. The aim of this study was to evaluate the safety and efficacy of a new endorectal manual technique in patients with obstructed defecation due to the combination of muco-hemorrhoidal prolapse and rectocele.
Methods
Patients enrolled after preoperative obstructed defecation syndrome (ODS) score, defecography and anoscopy were submitted to the novel Mucopexy-Recto Anal Lifting (MuRAL) combined with a modified Block procedure, and followed up by independent observers with digital exploration 3 weeks postoperatively, and digital exploration plus anoscopy at 3, 6, and 12 months. Operative time, hospital stay, numerating rating scale (NRS), ODS, satisfaction scores, and recurrence rate were recorded.
Results
Mean operative time was 35.7 minutes. Fifty-six patients completed 1-year follow-up: 7.1% had acute urinary retention, NRS score was < 3 from the third postoperative day, mean time of daily activity resumption was 12 days, none had persistent fecal urgency, 82% declared excellent/good satisfaction score, significant improvement of 6- and 12-month ODS score, no recurrence of rectocele, and 7.1% recurrence of prolapsed hemorrhoids were observed.
Rectocele is a very common finding, particularly in multiparous and/or hysterectomized females; it can be asymptomatic, or cause dyspareunia or obstructed defecation syndrome (ODS), when associated with mucosal rectal prolapse and/or prolapsed hemorrhoids. Although about 30% of patients with ODS may benefit from surgery, the ideal surgical approach to deal with the problem is far from defined with different approaches, techniques, and outcomes [1]. Transanal approaches are appreciated for their minimal aesthetic impact, while the traditional manual techniques are not easy to perform with risk of bleeding, rectovaginal fistula, and recurrence [2]. Though the more recent stapled transanal resection technique using 1 [3], or 2 circular staplers [4], achieved better results than the traditional techniques in the midterm period, a number of severe complications were reported [56]. The Mucopexy-Recto Anal Lifting (MuRAL) method, a recently standardized technique of hemorrhoidopexy, turned out to be a safe and effective minimally invasive approach in managing symptomatic hemorrhoids, with low recurrence rate and without exposing patients to the risk of developing severe complications [7]. The aim of this study was to report the technical notes and outcomes of combining MuRAL with a modified Block technique in patients affected by ODS, due to the association of rectocele and prolapsed hemorrhoids.
From November 2013 to December 2018 a series of consecutive patients with ODS, underwent MuRAL combined with a modified Block procedure. Preoperatively, a validated ODS score [8] had been administered and all patients had anoscopy and defecography, to exclude enterocele and to confirm the rectocele size, initially evaluated at digital exploration.
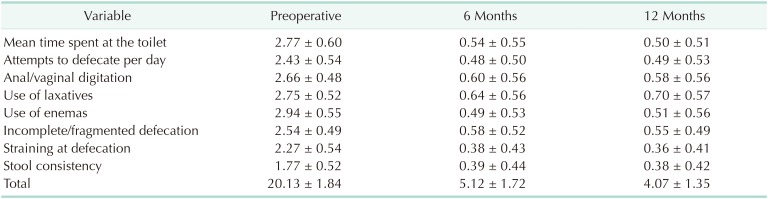
The adapted ODS score is based on the evaluation of the following items: mean time spent at the toilet, number of attempts to defecate per day, presence of anal/vaginal digitation, use of laxatives and enemas, presence of incomplete/fragmented defecation and/or straining at defecation, and stool consistency. The minimum score is 0, the maximum is 31.
Upon receiving informed consent from all patients, the procedures were performed by the same 2-surgeon team, following the technique reported below. The intervention was performed under general, or spinal anesthesia. All patients received 500 mg of Metronidazole intravenously, 1 hour before the intervention. The study has been approved by the Milan Area 1 Ethics Committee (decision number 017/55113).
With the patient in lithotomy position, an HPS anoscope (HemorPex System Angiologica srl, S. Martino Siccomario, Italy), with the operating window positioned at 12 o'clock, is anchored to perineal skin with silk 0/0 stitches.
As the first step of the procedure, the endoanal repair of the rectocele is accomplished with a modified Block technique. The original technique consists of a transanal obliterative running absorbable suture, including the submucosal and muscular layers, usually “carried out in conjunction with the excision of the right anterior internal/external hemorrhoid.” The suture is conducted “one centimeter past the upper edge of the rectocele and returned as a reinforcing lock stitch to the beginning of the suture line and tied there.” In our modification after positioning the anoscope with the operating window at 12 o'clock, in correspondence with the rectocele defect, a double mucosal stitch is passed at the lower edge of the operating window, continuing with a single ascending running mucosalsubmucosal suture with slowly absorbable Polyglycolic Acid 0/0 thread (5/8 needle 26 mm), progressing up to 1 cm past the upper edge of the rectocele. Repair of the rectocele is completed with a suture contraction, achieved by tying together the proximal and distal ends of the thread. No associated hemorrhoidal excision is done (Fig. 1). Instead, 6 columns of hemorrhoidal arterial ligation and mucopexy are performed with the same type of thread, by accessing selectively and repairing the prolapse in the following order: 11, 1, 9, 3, 7, 5 o'clock position (Fig. 2). A standardized rotation sequence of the device's operating window has been applied in the aim of preventing the dragging of the mucosa inside the device when changing the quadrant of hemorrhoidopexy. The 6 ascending sutures involving mucosa and submucosa are performed with passages at every 2–4 mm, starting from the artery ligation knot and progressing upwards; the mucopexy is completed with a suture contraction and a folding of the suture achieved with a deep passage below the location where the arterial ligation has been performed (Fig. 3). Finally, hemostasis is checked. No hemostatic sponge is left in place.
The lifting effect can only be obtained if the stitches involve mucosa and submucosa, whereby the resolution of the prolapse is left to the subsequent fibrosis. The 0/0 slowly absorbable Polyglycolic Acid braided thread is used with the aim of promoting an inflammatory reaction leading ultimately to the formation of significant fibrosis along the mucopexy columns, as aimed for with the endorectal repair of rectocele (Fig. 4).
During hospitalization all patients are administered 1,000 mg of Acetaminophen intravenously every 8 hours. Ketorolac (30 mg intravenously) is administered as a rescue drug, when numerating rating scale (NRS) pain score is greater than 4. After discharge, the patients are advised to take 1,000 mg of Acetaminophen orally, or 80 mg of Ketoprofene, when needed.
Follow-up tests were carried out by independent observers (2 surgeons who had not been involved in performing the procedure). Clinical examination included a digital exploration 3 weeks after the operation. However, unless there was evidence of early recurrence, proctoscopy was not performed in the early period to avoid possible mechanical disruption of the mucopexy columns. Systematic controls with digital exploration plus anoscopy were performed at 3, 6, and 12 months.
The following clinical parameters were considered: duration of intervention, length of in-hospital stay and complications, NRS score [9] of postoperative pain, time of return to normal activity, postoperative ODS score, and anorectal and/or gynecological symptoms. NRS is a validated pain score, based on a numerical scale, ranging from 0 (no pain) to 10 (worst pain imaginable).
Patient Satisfaction Score was assessed at 1 year controlled by an independent trained nurse, using a 4-point scale (1, excellent; 2, good; 3, fairly good; 4, poor), expressing the overall personal perception of the patient. Finally, the recurrence rate, defined as recurrence of rectocele > 2 cm and/or muco-rectal prolapse was checked. Continuous data for statistical analysis were shown as arithmetic mean (±standard deviation [SD]) and qualitative data as absolute and percent frequencies. The IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA) was used. The t-test and the Wilcoxon test for scores were used, as appropriate. Differences were considered significant with values of P < 0.05.
From November 2013 to December 2018, 56 female patients with a mean age 54.5 years (range, 33–79 years) were operated on. Five patients had been previously submitted to anorectal surgery: 2 stapled hemorrhoidopexy, 1 MuRAL, 1 Milligan-Morgan. Fifty-three patients (92.6%) had parity, of whom 31 (55.3%) were multiparous; 8 patients (14.3%) had been previously hysterectomized. Mean (±SD) preoperative ODS score was 20.13 (±1.84), 16 patients (28.6%) had weekly rectal bleeding, 11 (19.6%) dyspareunia.
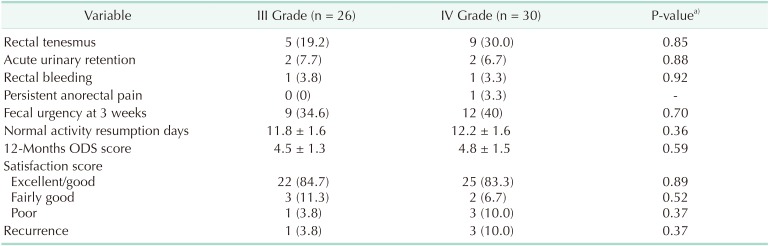
At anoscopy all patients showed prolapsed circular hemorrhoids (26 patients had grade III, and 30 had grade IV hemorrhoids) and rectocele > 3 cm. None of the multiparous and/or hysterectomized patients showed a dynamic enterocele during defecation at defecography. Twenty-two patients (39.3%) underwent spinal anesthesia, the others had general anesthesia.
The overall mean duration of the intervention was 35.7 minutes (range, 14–70 minutes); 37 patients (66.1%) had 1-day surgery, 13 patients (23.2%) had same-day surgery, and 6 (10.7%) needed 2 or more days hospitalization.
Mean (±SD) NRS score, recorded over 3 days following surgery, was 4.5 (±1.5) and 3.6 (±1.3) and 2.7 (±1.3) in the first, second, and third day, respectively.
Regarding postoperative complications: 12 patients (21.4%) suffered from rectal tenesmus, which disappeared within 3 days after intervention; 4 patients (7.1%) all submitted to spinal anesthesia, had acute urinary retention, 2 had bleeding and 1 persistent anorectal pain. Mean time to normal activity resumption was 12 days (range, 7–14 days). At the 3-week check, 21 patients (37.5%) reported fecal urgency. At 3 months the incidence of fecal urgency was reduced to 10.7%; no patient reported this complaint at the 12-month examination. ODS scores at 6 and 12 months are reported in Table 1, with a significant improvement versus preoperative data (P < 0.01). Preoperative anorectal bleeding and dyspareunia disappeared in all patients.
The patient satisfaction scores at 6-month follow-up were 26.8% excellent, 57.2% good, 8.9% fairly good, and 7.1% poor. None had recurrence of rectocele and 4 patients (7.1%) developed a recurrence of hemorrhoids; 2 cases were observed within 6 months and 2 cases 12 months after intervention. The recurrences were successfully managed with 1 redo-MuRAL and 1 Milligan-Morgan.
Table 2 reports in detail the complications and functional results in patients with preoperative grade III and IV hemorrhoids. No statistically significant difference was observed, with only a trend to less transient fecal urgency, earlier normal activity resumption, and lower recurrence rate in patients with less advanced hemorrhoidal disease.
The surgical treatment of ODS is one of the most debated topics in coloproctology. Various techniques to correct rectocele with vaginal, perineal, transanal and combined approaches have been proposed in the past, with controversial results. In 1999, Van Laarhoven et al. [10] demonstrated that the perfect repair of rectocele is often not sufficient to correct an ODS, with 30%–72% of persistence of symptoms: this finding it is not surprising, considering that rectocele is usually associated with other abnormalities, particularly internal rectal mucosal prolapse, prolapsed hemorrhoids, and/or enterocele, that are the main cause of impaired defecation.
In the past 2 decades, the traditional transanal manual surgical techniques, namely the Block and the Sullivan-Sarles procedures, have been challenged by transanal stapled techniques based on the use of single, or double circular stapler, with the aim of improving efficacy and overcoming the limits of the past, particularly technical difficulties, frequent intra- and postoperative bleeding, and risk of rectovaginal fistula (Sullivan-Sarles procedure) [11], and high incidence of recurrence, due to the dehiscence of the suture (Block procedure).
Transanal stapled surgery rapidly spread all over the world with good results, particularly in the early- and midterm period after operation; nevertheless a number of severe complications were reported by various authors, and several meta-analyses demonstrated that stapled surgery has a significantly higher recurrence rate of hemorrhoids than traditional hemorrhoidectomy.
Our results demonstrated a complete resolution of rectocele with a low rate of recurrence of prolapsed hemorrhoids at 1-year follow-up, and a significant reduction of ODS score.
In our hands, the combination of MuRAL and modified Block procedures seemed to offer good efficacy in treating patients with symptomatic rectocele, with no rectocele recurrence. In our opinion, the inflammatory reaction generated by the 7 sutures with subsequent fibrosis plays an essential role with both the recto-anal lifting and the rectocele repair: this hypothesis is supported by the observation of a “fibrosis basket” at anoscopy performed 1 year postoperatively in our patients, confirmed by colonoscopy 3 years postoperatively (Fig. 4).
Incidence of fecal urgency was appreciably lower in comparison with rates reported after stapled hemorrhoidopexy and STARR (stapled transanal rectal resection), and this symptom disappeared within a few months. None of the serious complications reported after stapled surgery were observed in our series of patients.
Arterial ligation by itself seems to have limited efficacy in the treatment of prolapsed hemorrhoids, nevertheless a number of experiences with the association of Doppler-guided arterial ligation (DG-HAL) with mucopexy (recto-anal repair, RAR) proved to significantly reduce the main symptoms caused by the prolapse, or the anal mucosa sliding in a non-negligible number of patients with grade IV hemorrhoidal disease [1213].
Sharing the same principles, MuRAL aims at delivering arterial ligation and mucopexy by adopting a standardized rotation sequence, with similar results as those achieved by DG-HAL and RAR, taking into account that the use of a Doppler guide does not affect prolapse reduction [7].
This is a preliminary study with some limits: the number of patients is low, the follow-up is too short to determine the effective risk of recurrences, and there is not a control group.
Nevertheless, the aim of the study was to demonstrate the feasibility and safety of the new operation, and the immediate and short-term results were very encouraging, particularly considering the absence of severe complications.
Randomized prospective studies are needed in order to assess which is the best treatment solution for managing ODS and enhancing the clinical efficacy. Finally, the hypothesis that the mucopexies could facilitate an intense fibrotic reaction, which should stabilize the vertical lifting effect and prevent recurrences as we observed at anoscopy 1 year after the operation, needs confirmation by experimental studies.
In our preliminary experience the combination of MuRAL and modified Block procedures, turned out to be a safe and effective minimally invasive approach in managing ODS caused by symptomatic rectocele, associated with muco-rectal prolapse and prolapsed hemorrhoids, with no severe complications. In our series, the ODS score improved significantly and more than 80% of the patients reported a good or excellent satisfaction score. Further comparative randomized studies with a larger series of patients and longer follow-up period are needed.
References
1. Boccasanta P, Venturi M, Calabro G, Trompetto M, Ganio E, Tessera G, et al. Which surgical approach for rectocele? A multicentric report from Italian coloproctologists. Tech Coloproctol. 2001; 5:149–156. PMID: 11875682.
2. Block IR. Transrectal repair of rectocele using obliterative suture. Dis Colon Rectum. 1986; 29:707–711. PMID: 3533470.
3. Tjandra JJ, Chan MK. Systematic review on the procedure for prolapse and hemorrhoids (stapled hemorrhoidopexy). Dis Colon Rectum. 2007; 50:878–892. PMID: 17380367.
4. Guttadauro A, Chiarelli M, Maternini M, Baini M, Pecora N, Gabrielli F. Value and limits of stapled transanal rectal repair for obstructed defecation syndrome: 10 years-experience with 450 cases. Asian J Surg. 2018; 41:573–577. PMID: 28693959.
5. Pescatori M, Gagliardi G. Postoperative complications after procedure for prolapsed hemorrhoids (PPH) and stapled transanal rectal resection (STARR) procedures. Tech Coloproctol. 2008; 12:7–19. PMID: 18512007.
6. Jayne DG, Schwandner O, Stuto A. Stapled transanal rectal resection for obstructed defecation syndrome: one-year results of the European STARR Registry. Dis Colon Rectum. 2009; 52:1205–1212. discussion 1212-4. PMID: 19571694.
7. Pagano C, Vergani C, Invernizzi C, Bussone M, Benegiamo G, Venturi M. Mucopexyrecto anal lifting: a standardized minimally invasive method of managing symptomatic hemorrhoids, with an innovative suturing technique and the HemorPex System®. Minerva Chir. 2018; 73:469–474. PMID: 29652112.
8. Altomare DF, Spazzafumo L, Rinaldi M, Dodi G, Ghiselli R, Piloni V. Set-up and statistical validation of a new scoring system for obstructed defaecation syndrome. Colorectal Dis. 2008; 10:84–88. PMID: 17441968.
9. Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978; 37:378–381. PMID: 686873.
10. Van Laarhoven CJ, Kamm MA, Bartram CI, Halligan S, Hawley PR, Phillips RK. Relationship between anatomic and symptomatic long-term results after rectocele repair for impaired defecation. Dis Colon Rectum. 1999; 42:204–210. discussion 210-1. PMID: 10211497.
11. Sarles JC, Arnaud A, Selezneff I, Olivier S. Endo-rectal repair of rectocele. Int J Colorectal Dis. 1989; 4:167–171. PMID: 2768999.
12. Cho SW, Lee RA, Chung SS, Kim KH. Early experience of doppler-guided hemorrhoidal artery ligation and rectoanal repair (DG-HAL & RAR) for the treatment of symptomatic hemorrhoids. J Korean Surg Soc. 2010; 78:23–28.
13. Ratto C, Campenni P, Papeo F, Donisi L, Litta F, Parello A. Transanal hemorrhoidal dearterialization (THD) for hemorrhoidal disease: a single-center study on 1000 consecutive cases and a review of the literature. Tech Coloproctol. 2017; 21:953–962. PMID: 29170839.
Fig. 1
(a) Modified Block procedure performed at 12 o'clock position, (b) rectal prolapse, (c) enterocele, (d) cystocele.
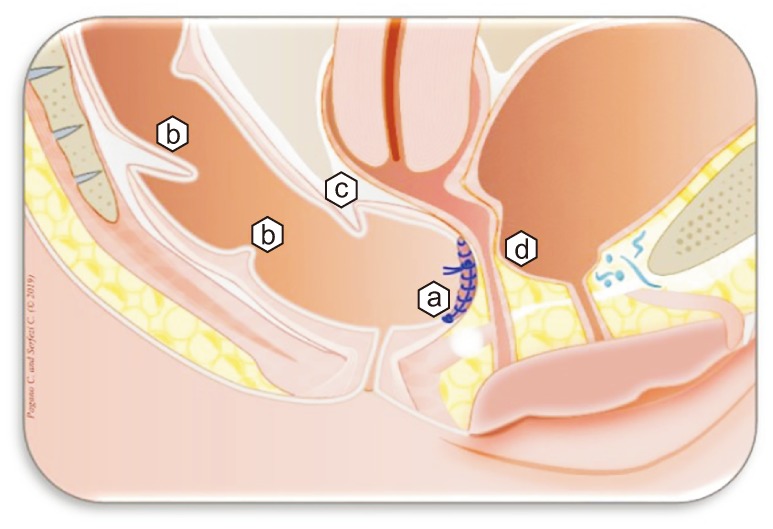
Fig. 2
Procedure sequence: rectocele repair at 12 o'clock; 6 arterial ligations and mucopexies: first at 11, second at 1, third at 9, fourth at 3, fifth at 7, and sixth at 5 o'clock. RA, right anterior; LA, left anterior; RL, right lateral; LL, left lateral; RP, right posterior; LP, left posterior.

Fig. 3
Suturing technique of each mucopexy: arterial ligation, mucopexy, suture contraction, suture folding, and securing knot.
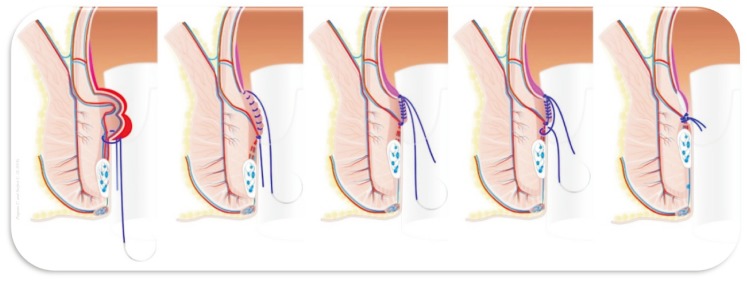
Table 1
Pre- and postoperative (6 and 12 months) obstructed defecation syndrome score (from 0 to 31) [5] in 56 patients submitted to MuRAL + Block procedure




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download