Abstract
Purpose
After kidney transplantation (KT), a large amount of drainage can delay postoperative recovery. Viscum album extract is an agent used in pleurodesis, and the purpose of this study was to evaluate the efficacy of this agent in reducing the amount of drainage after KT.
Methods
Medical records of patients with a large amount of drainage (≥ 100 mL/day) on postoperative day (POD) 7 after KT who had undergone V. album extract instillation through drainage tube (n = 115) or conservative management (n = 177) were retrospectively reviewed. The primary endpoint was a decrease in the amount of drainage on POD 14 from POD 7.
Results
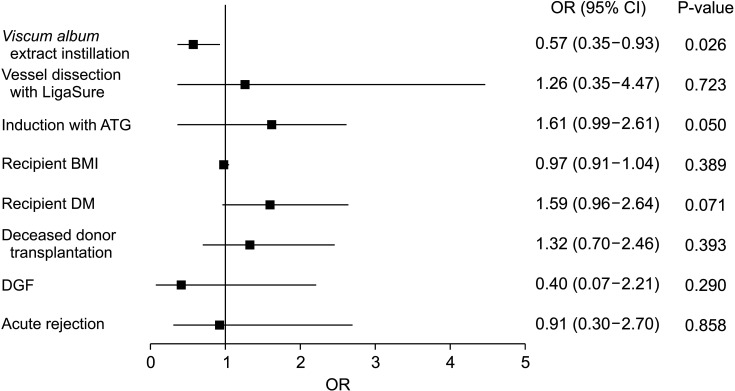
A decrease in the amount of drainage on POD 14 from POD 7 was larger in the V. album extract instillation group than in the conservative management group (–228.3 ± 181.6 mL vs. –144.6 ± 202.0 mL, P < 0.001). Duration of hospitalization after operation was shorter in the V. album extract instillation group than in the conservative management group (15.9 ± 3.2 days vs. 18.1 ± 5.3 days, P < 0.001). In multivariate analysis, there was a statistically significant association of V. album extract instillation with lower risk of persistent large amount of drainage (≥ 100 mL/day on POD 14), with an odds ratio of 0.57 (95% confidence interval, 0.35–0.93; P = 0.026).
Go to : 
In many transplantation centers, drainage tubes are placed after kidney transplantation (KT) to prevent collection of lymphatic fluid within the surgical cavity [1]. Drainage tubes can also serve to monitor bleeding and urine leakage after transplantation. Drainage tubes are usually removed when the amount of drainage decreases to less than a certain amount to prevent the formation of lymphocele, because lymphocele can cause symptoms such as pain or complications even impairing graft function by compressing surrounding structures [2].
However, in some patients, drainage tubes cannot be removed for a considerable period because the drainage volume does not decrease. In such cases, postoperative recovery of patients may be delayed due to discomfort such as pain caused by drainage tubes. And drainage tubes that continue to remain unremoved can lead to wound infection, which can be fatal in immunosuppressed KT patients [3]. In addition, since many patients want to be discharged from the hospital after removing the drainage tube, an unremoved drainage tube can prolong the hospital stay, which can lead to an increase in medical costs.
In lymphocele treatment, sclerotherapies through instillation of povidone iodine, ethanol, fibrin sealant, and so on to a site where lymphatic fluid leakage occurs have been studied as one of the treatment methods with favorable outcome [456]. And it has been reported that extract from Viscum album, a European mistletoe, can also be used for lymphocele treatment by inducing perigraft adhesion [78]. V. album extract (sold under the brand name Helixor M; Helixor Heilmittel GmbH, Rosenfeld, Germany), one of the agents used in a pleurodesis procedure when treating malignant pleural effusion, is known to cause chemical pleurodesis by inducing nonspecific inflammation and fibrosis [9]. However, there have been no studies to date on the effects of V. album extract instillation in patients with a large amount of drainage after KT. Thus, the objective of this study was to evaluate the efficacy of this agent in reducing the amount of drainage in KT patients. Other clinical benefits of V. album extract in KT patients were also investigated.
Go to : 
Medical records of patients who had undergone KT between January 2016 and December 2020 at Seoul St. Mary’s Hospital were retrospectively reviewed. During the transplantation, careful ligation with ties or sealing with LigaSure (Medtronic, Minneapolis, MN, USA) was performed for the lymphatics at the time of vessel dissection, and a 4.8-mm–diameter Jackson-Pratt (JP) drainage tube was inserted before closing the fascia so that it was placed around the transplanted kidney for all patients. Patients with a large amount of drainage (≥100 mL per day) on postoperative day (POD) 7 were analyzed in this study. The drainage amount itself was set as the inclusion criteria regardless of creatinine rise, leg swelling, or any sign of infection, because it was considered that complications due to lymphocele itself could not occur while the drainage tube was already placed. Whether to instill V. album extract or to perform only conservative management was decided by the operator surgeon based on intraoperative findings, and V. album extract was instilled mainly for patients who were observed to have abundant lymphatics at the time of operation. For those who determined to be instilled with V. album extract, 100 mg of Helixor M was instilled into the retroperitoneal space through the JP drainage tube and the tube was clamped for 8 hours. Then, the position of patient was changed every 2 hours to achieve adequate distribution of V. album extract within the retroperitoneal space. Additional adjustment of the instillation dose of V. album extract according to the primary drainage amount was not performed during the study period. In both the patient group instilled with V. album extract and the group given only conservative management without instillation, the drainage tube was removed when the drainage amount was less than 100 mL per day.
The primary endpoint was a decrease in the amount of drainage on POD 14 from POD 7. This primary outcome was set for the purpose of assessing the drainage volume reduction effect of V. album extract instillation compared to conservative management during the same period, considering that there is a difference in the baseline drainage volume of POD 7 in the patients. The secondary endpoint was postoperative recovery reflected by the duration of hospitalization after operation.
Student t-test or Mann-Whitney U-test was used for comparing continuous variables, and the chi-square test or Fisher exact test was used for comparing proportions of categorical variables. Logistic regression analysis was performed to identify factors affecting dependent variables. P-values of <0.05 were considered statistically significant. Statistical analysis was performed using IBM SPSS Statistics ver. 24.0 (IBM, Armonk, NY, USA).
This study was performed in accordance with the Declaration of Helsinki and was approved and monitored by the Institutional Review Board (IRB) of our institution. The need for informed consent was waived by IRB because patients’ data were deidentified (No. KC21RASI0350).
Go to : 
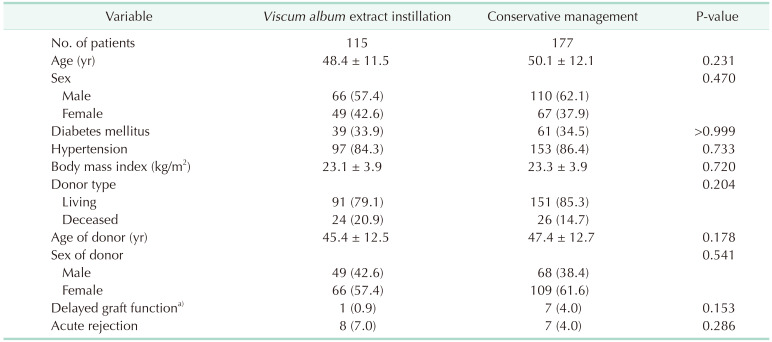
Between January 2016 and December 2020, 838 patients underwent either living donor or deceased donor KT. Of them, 292 patients with a large amount of drainage on POD 7 (≥100 mL per day) were identified, including 115 patients who received V. album extract instillation and 177 patients who received conservative management. Clinical characteristics of these patients and their corresponding donors are shown in Table 1. Demographic characteristics of recipients and donors, underlying diseases of recipients, and occurrence of delayed graft function and acute rejection in the 2 groups were similar.
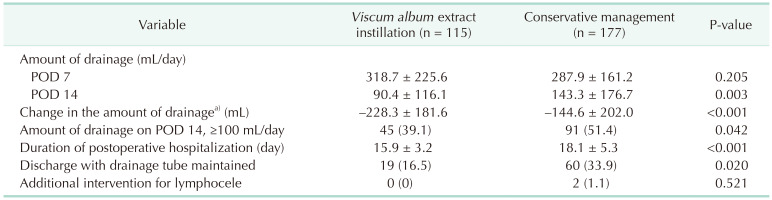
Table 2 shows postoperative data related to the amount of drainage and postoperative recovery. There was no significant difference in the amount of drainage on the day V. album extract was instilled (POD 7) between the 2 groups. However, compared to conservative management, V. album extract instillation resulted in a significantly less amount of drainage on POD 14 (90.4 ± 116.1 mL vs. 143.3 ± 176.7 mL, P = 0.003) and more decrease in the amount of drainage during 1 week after POD 7 (–228.3 ± 181.6 mL vs. –144.6 ± 202.0 mL, P < 0.001). Furthermore, the V. album extract instillation group showed a significantly shorter hospital stay (15.9 ± 3.2 days vs. 18.1 ± 5.3 days, P < 0.001), and a lower rate of discharge with drainage tube maintained (16.5% vs. 33.9%, P = 0.020). Two patients in the conservative management group required intervention for the development of lymphocele and laparoscopic internal drainage operations were done in these patients. There was no patient who underwent additional intervention for lymphocele in the V. album extract instillation group.
Results of multivariate logistic regression analysis to examine adjusted association of V. album extract instillation, vessel dissection method, induction with antithymocyte globulin (ATG), in addition to previously reported risk factors for the development of lymphocele after KT, with persistent large amount of drainage (≥100 mL per day on POD 14) are shown in Fig. 1. Previously reported risk factors used in the analysis included recipient body mass index [1011], recipient diabetes mellitus [12], deceased donor transplantation [13], delayed graft function [14], and acute rejection [1415]. There was a statistically significant association of V. album extract instillation with lower risk of persistent large amount of drainage, resulting in an odds ratio of 0.57 (95% confidence interval, 0.35–0.93; P = 0.026). There was no significant association of other clinical factors with persistent large amount of drainage.
Among the patients who were followed up for more than 1 year after operation, biopsy-confirmed chronic rejection occurred in 3 patients in the conservative management group. There was no patient with biopsy-confirmed chronic rejection in the V. album extract instillation group, and no other identifiable immunologic complications occurred.
Go to : 
In this study, retroperitoneal V. album extract instillation in patients with a large amount of drainage after KT resulted in more decrease in the amount of drainage during 1 week after POD 7, compared to conservative management. And there was a significant association of V. album extract instillation with lower risk of persistent large amount of drainage. In addition, V. album extract instillation induced a shorter hospital stay, meaning that the effective reduction in the amount of drainage had a positive effect on patients’ recovery after transplantation.
There have been many studies on therapeutic options for already formed lymphoceles, including aspiration, sclerotherapy, and surgery [16]. However, there are few studies on methods to reduce the amount of drainage before the formation of lymphoceles. Among methods used for lymphocele treatment, aspiration through additional needling or surgery is an invasive method, so a suitable method to be applied before lymphocele formation might be a method of instilling a sclerotherapy agent through an already inserted drainage tube. In our study, there was no patient with an identifiable lymphocele formation after V. album extract instillation, suggesting that sclerotherapy with V. album extract could be clinically useful in the pre-lymphocele stage.
V. album extract has been used for a relatively long time for treating pleural effusion, but the exact mechanism of action of sclerosis induced by V. album extract is not well understood yet. Lee et al. [9] have reported a pleurodesis with V. album extract as an effective procedure for controlling malignant pleural effusion in lung cancer patients, and assumed that both an inflammatory reaction involving visceral and parietal pleura and a nonspecific immune activation contributed to the outcome. We presume that V. album extract could cause sclerosis in the retroperitoneal space through a mechanism similar to that in the case of pleurodesis, but additional basic research is needed to confirm this.
Current transplantation centers have different policies regarding drainage tube. There are centers, including ours, that routinely put the JP drain during KT based on evidences that intraoperative placing of drains decreases the incidence of complications associated with lymphocele [17], and there are also centers that do not place drain considering it has no benefit. Furthermore, the amount of drainage that is used as a criterion for drainage tube removal is different even between centers where drainage tubes are routinely placed. Based on clinical experience of our institution so far, our center removes the drainage tube when the daily drainage volume is less than 100 mL from POD 7, but there will be centers that remove the drainage tube at a much lower amount of drainage. However, from January 2016 to December 2020, no patients with newly developed symptomatic lymphocele after removal of the drainage tube were identified at our center, and the drainage volume at POD 7 of the 2 patients who needed additional intervention for lymphocele in this study was 185 and 454 mL, respectively. Therefore, the results of this study, which was conducted by setting the daily drainage amount above 100 mL as the inclusion criteria, could have clinical implication that can be applied when drainage tubes are routinely placed during KT.
In this study, the proportion of patients with a large amount of drainage among overall KT recipients in our institution during the study period was 34.8%, which is relatively high considering the known incidence of lymphocele after KT. During our recipient operation, ligation with ties or sealing with LigaSure was performed for the lymphatics at the time of vessel dissection. However, the method of vessel dissection appears insufficient to explain the relatively large amount of drainage in this study, since there was no difference in the amount of drainage on POD 7 between the patients operated with ties and those operated with LigaSure (300.9 ± 189.8 mL vs. 279.4 ± 188.3 mL, P = 0.713). Furthermore, there was no significant association of vessel dissection method with a persistent large amount of drainage in the multivariate logistic regression analysis. A possible explanation for the large amount of drainage is that ATG was used as induction agent for many patients in this study. It has been indicated that T cell depletion might impair the mechanical strength of tissue [18], and a higher incidence of lymphocele in the patients receiving ATG was also reported previously [19]. In addition, there was a tendency in which ATG use was associated with a higher risk of a persistent large amount of drainage in this study, resulting in an odds ratio of 1.61 (95% confidence interval, 0.99–2.61; P = 0.050) in the multivariate logistic regression analysis. In our institution, the number of immunologically high-risk transplantation has increased continuously, and the number of induction therapy with ATG also increased [20]. ATG was used as the induction immunosuppressant in 36.9% of overall KT recipients in our institution during the study period and in 45.5% of patients with a large amount of drainage, while ATG was given to 20.2% of overall KT recipients in Korea in 2016 [21].
This study has several potential limitations. The first limitation is that specific analysis of adverse events related to V. album extract instillation was not performed. Previous studies on lymphocele treatment have reported that the instillation of a sclerotherapy agent is associated with complications such as infections [22], but no other side effects occurred in our study except for mild pain or fever that did not require medication. However, since these minor side effects can negatively affect patients’ recovery process, it might be necessary to analyze them. In addition, in terms of investigating the possibility of potential side effects related to the mechanism of action of V. album extract, it might be helpful to utilize novel biomarkers for fibrosis of kidney allograft such as urinary transglutaminase 2 [23]. Second, in this study, a fixed dose was instilled to all patients when the V. album extract was used, which did not take into account the primary drainage amount or bodyweight of each patient. Therefore, further studies are needed to determine whether the instillation dose should be adjusted differently according to the patient’s characteristics. Finally, we were unable to exclude the possibility of selection bias due to the retrospective design of this study. Although this study has a relatively large sample size compared to previous studies on lymphocele sclerotherapy, prospective studies need to be conducted in order to provide more robust evidence for V. album extract instillation after KT.
In conclusion, retroperitoneal V. album extract instillation was effective in reducing the amount of drainage and shortening the duration of hospitalization, suggesting that V. album extract instillation could be considered for a faster postoperative recovery in patients with a large amount of drainage after KT.
Go to : 
References
1. Mehrabi A, Fonouni H, Wente M, Sadeghi M, Eisenbach C, Encke J, et al. Wound complications following kidney and liver transplantation. Clin Transplant. 2006; 20 Suppl 17:97–110. PMID: 17100709.

2. Sawhney R, D'Agostino HB, Zinck S, Rose SC, Kinney TB, Oglevie SB, et al. Treatment of postoperative lymphoceles with percutaneous drainage and alcohol sclerotherapy. J Vasc Interv Radiol. 1996; 7:241–245. PMID: 9007804.

3. Petrosillo N, Drapeau CM, Nicastri E, Martini L, Ippolito G, Moro ML, et al. Surgical site infections in Italian Hospitals: a prospective multicenter study. BMC Infect Dis. 2008; 8:34. PMID: 18328101.

4. Zomorrodi A, Buhluli A. Instillation of povidone iodine to treat lymphocele and leak of lymph after renal transplantation. Saudi J Kidney Dis Transpl. 2007; 18:621–624. PMID: 17951955.
5. Tasar M, Gulec B, Saglam M, Yavuz I, Bozlar U, Ugurel S. Posttransplant symptomatic lymphocele treatment with percutaneous drainage and ethanol sclerosis: long-term follow-up. Clin Imaging. 2005; 29:109–116. PMID: 15752966.
6. Silas AM, Forauer AR, Perrich KD, Gemery JM. Sclerosis of postoperative lymphoceles: avoidance of prolonged catheter drainage with use of a fibrin sealant. J Vasc Interv Radiol. 2006; 17(11 Pt 1):1791–1795. PMID: 17142709.

7. Evans M, Bryant S, Huntley AL, Feder G. Cancer patients' experiences of using mistletoe (Viscum album): a qualitative systematic review and synthesis. J Altern Complement Med. 2016; 22:134–144. PMID: 26684278.

8. Kim M, Hwang J. Direct intranodal lipiodol injection for management of lymphocele in kidney transplant recipient. Korean J Transplant. 2020; 34(Supple 1):S111.

9. Lee YG, Jung I, Koo DH, Kang DY, Oh TY, Oh S, et al. Efficacy and safety of Viscum album extract (Helixor-M) to treat malignant pleural effusion in patients with lung cancer. Support Care Cancer. 2019; 27:1945–1949. PMID: 30218188.

10. Atray NK, Moore F, Zaman F, Caldito G, Abreo K, Maley W, et al. Post transplant lymphocele: a single centre experience. Clin Transplant. 2004; 18 Suppl 12:46–49. PMID: 15217407.

11. Goel M, Fle chner SM, Zhou L, Mastroianni B, Savas K, Derweesh I, et al. The influence of various maintenance immunosuppressive drugs on lymphocele formation and treatment after kidney transplantation. J Urol. 2004; 171:1788–1792. PMID: 15076277.

12. Ulrich F, Niedzwiecki S, Fikatas P, Nebrig M, Schmidt SC, Kohler S, et al. Symptomatic lymphoceles after kidney transplantation - multivariate analysis of risk factors and outcome after laparoscopic fenestration. Clin Transplant. 2010; 24:273–280. PMID: 19719727.

13. Derouiche A, Mechri M, Ktari MM, Helal I, Ben Abdallah T, Chebil M. [Lymphoceles after renal transplantation: study of risk factors]. Prog Urol. 2010; 20:301–306. French. PMID: 20380993.
14. Khauli RB, Stoff JS, Lovewell T, Ghavamian R, Baker S. Post-transplant lymphoceles: a critical look into the risk factors, pathophysiology and management. J Urol. 1993; 150:22–26. PMID: 8510262.

15. Veeramani M, Mishra S, Kurien A, Ganpule A, Sabnis R, Desai M. Does rejection have a role in lymphocele formation post renal transplantation? A single centre experience. Indian J Urol. 2010; 26:193–195. PMID: 20877595.

16. Lucewicz A, Wong G, Lam VW, Hawthorne WJ, Allen R, Craig JC, et al. Management of primary symptomatic lymphocele after kidney transplantation: a systematic review. Transplantation. 2011; 92:663–673. PMID: 21849931.

17. Derweesh IH, Ismail HR, Goldfarb DA, Araki M, Zhou L, Modlin C, et al. Intraoperative placing of drains decreases the incidence of lymphocele and deep vein thrombosis after renal transplantation. BJU Int. 2008; 101:1415–1419. PMID: 18190623.

18. Peterson JM, Barbul A, Breslin RJ, Wasserkrug HL, Efron G. Significance of T-lymphocytes in wound healing. Surgery. 1987; 102:300–305. PMID: 3497461.
19. Benavides C, Mahmoud KH, Knight R, Barcenas C, Kahan BD, Van Buren CT. Rabbit antithymocyte globulin: a postoperative risk factor for sirolimus-treated renal transplant patients? Transplant Proc. 2005; 37:822–826. PMID: 15848544.

20. Kim MH, Jun KW, Hwang JK, Park SC, Yun SS, Moon IS, et al. Incidence and outcome of isolated distal deep vein thrombosis in kidney transplant recipients. Ann Surg Treat Res. 2020; 98:324–331. PMID: 32528912.

21. Park S, Kim M, Kim JE, Kim K, Park M, Kim YC, et al. Characteristics of kidney transplantation recipients over time in South Korea. Korean J Intern Med. 2020; 35:1457–1467. PMID: 32218102.

22. Risaliti A, Corno V, Donini A, Cautero N, Baccarani U, Pasqualucci A, et al. Laparoscopic treatment of symptomatic lymphoceles after kidney transplantation. Surg Endosc. 2000; 14:293–295. PMID: 10741452.

23. Kim JY, Wee YM, Choi MY, Jung HR, Choi JY, Kwon HW, et al. Urinary transglutaminase 2 as a potent biomarker to predict interstitial fibrosis and tubular atrophy of kidney allograft during early posttransplant period in deceased donor kidney transplantation. Ann Surg Treat Res. 2019; 97:27–35. PMID: 31297350.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download