Abstract
Purpose
In June 2016, the Model for End-Stage Liver Disease (MELD) score was employed in South Korea instead of the Child-Turcotte-Pugh (CTP) score. This study compared the outcomes of deceased donor liver transplantation (DDLT) before and after the MELD system application.
Methods
This retrospective study reviewed 48 patients who underwent DDLT for end-stage liver disease at a single tertiary referral center between January 2014 and December 2018. The patients were categorized into the pre-MELD (22 patients) and post-MELD (26 patients) groups. The demographics, postoperative outcomes, and overall survival time were evaluated between the 2 groups.
Results
The 2 groups had no differences in age, sex, ABO type, etiology for liver transplantation, CTP-score, operation time, cold ischemic time, and amount of red blood cell transfusion, although their MELD score differed significantly (post-MELD group, 36.2 ± 4.9; pre-MELD group, 27.7 ± 11.8; P < 0.001). The post-MELD group has longer intensive care unit stay (11.2 ± 9.5 days vs. 5.7 ± 4.5 days, P = 0.018) and hospital stay than the pre-MELD group (36.8 ± 26 days vs. 22.8 ± 9.3 days, P = 0.016). The 1-year survival rate was lower in the post-MELD group (61.5% vs. 86.4%, P = 0.029).
Conclusion
After MELD allocation, patients with high MELD scores had increased DDLT and consequently required a longer recovery time, which could negatively affect survival. According to the experience of a small-volume center, these problems were related to both severe organ shortages in South Korea and MELD allocation.
The standard for organ allocation for deceased donor liver transplantation (DDLT) remains controversial. Until June 2016, the Child-Turcotte-Pugh (CTP) score was used in South Korea as an index to evaluate the emergency degree of waiting for DDLT [12]. However, various shortcomings of this method have been discovered, and since June 2016, the allocation of DDLT was performed through the Model for End-Stage Liver Disease (MELD) score using the objective medical information of the patient [34]. The MELD system was designed to predict the survival potential of patients with liver cirrhosis after 3 months, and in the United States, organs have been allocated based on the MELD score since 2002 [3].
In the case of DDLT, when the MELD system was used in selecting transplant subjects, the mortality rate of waiting people decreased compared to when the CTP system was used. However, the 1-year survival rate of patients who received DDLT decreased, and the incidence of renal failure requiring kidney transplantation increased. In addition, the cost of disease treatment has increased by 55% since the introduction of the MELD system [5].
In the high-volume liver transplant center, many comparative analyses before and after the introduction of the MELD score have been published; however, the lower-volume center has not yet performed a comparative analysis, making the effectiveness of the MELD system inconclusive [6]. Therefore, by analyzing the outcome of patients who underwent DDLT before and after the introduction of the MELD score, we could consider its effectiveness and the correct direction for future MELD score implementation in South Korea.
This study aimed to analyze whether there were significant clinical results before and after the adoption of MELD in patients who underwent DDLT in our hospital and to evaluate the usefulness of MELD for DDLT in small liver transplant centers.
This retrospective study reviewed 48 patients who underwent DDLT for end-stage liver disease at Gachon University Gil Medical Center, a tertiary referral center, between January 2014 and December 2018. The patients were then categorized into 2 groups according to whether to introduce the MELD system; 22 were in the pre-MELD group and 26 were in the post-MELD group. The study was approved by the Institutional Review Board of Gachon University Gil Medical Center (No. GDIRB2020-306). This study was performed in accordance with the Declaration of Helsinki and written informed consent was waived due to its retrospective nature.
The main outcomes of this study were the 1-, 3-, and 5-year overall survival rates, 3-, 6-, 9-, and 12-month mortality rates, and postoperative intensive care unit stay. The secondary outcomes were the length of postoperative hospital stay, operation time, morbidity of Clavien-Dindo grade IIIa or worse, and readmission within 30 days.
The data on the following parameters were collected from each patient: demographic characteristics, including age, sex, ABO type, preoperative body mass index, primary liver disease, CTP score, MELD score (3.78 ln [bilirubin] + 11.20 ln [international normalized ratio] + 9.57 ln [creatinine] + 6.43) [7], and proportion of combined hepatocellular carcinoma (HCC). Perioperative and postoperative outcomes, including operation time, red blood cell transfusion, intraoperative and postoperative complications, postoperative intensive care unit stay, and hospital stay duration, were prospectively collected and evaluated. Additionally, the 1-, 3-, and 5-year overall survival rates, 3-, 6-, 9-, and 12-month mortality rates, and readmission within 30 days were evaluated between the 2 groups. To assess the postoperative morbidity rate, all events that occurred during the same hospital stay and within 30 days of operation were analyzed. Postoperative morbidities were recorded according to the Clavien-Dindo classification system [8]. Survival time was defined as the time from the date of operation to the date of death or the last follow-up.
Patient demographics and perioperative and postoperative outcomes were compared between the pre-MELD and MELD groups using the analysis of variance or t-tests for continuous variables and the chi-square tests for categorical variables. Kaplan-Meier analyses were conducted to compare survival rates between the 2 groups, and log-rank tests were used to compare differences in survival. The median survival time was estimated from the Kaplan-Meier curves. Cox proportional hazards models were used to evaluate risk factors affecting the survival rate. All analyses were performed using IBM SPSS Statistics ver. 22.0 (IBM Corp., Armonk, NY, USA). Statistical significance was set at P < 0.05 (2-tailed).
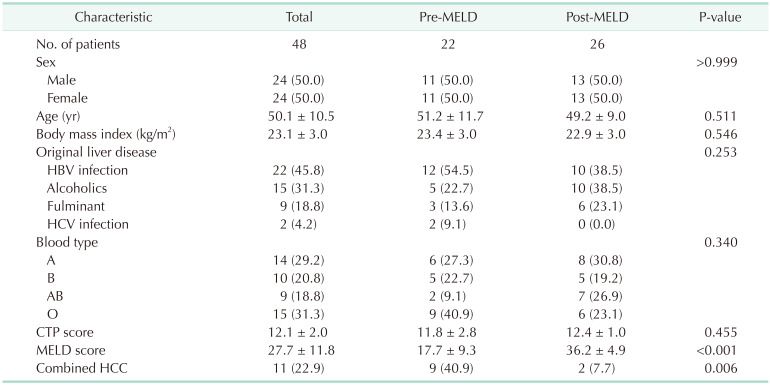
The baseline characteristics of the 2 groups are summarized in Table 1. The mean age was 50.1 years, and 24 patients were male. The causes of end-stage liver disease were HBV infection (n = 22, 45.8%), alcohol-induced hepatitis (n = 15, 31.3%), fulminant hepatitis (n = 9, 18.8%), and HCV infection (n = 2, 4.2%). No significant differences were observed in terms of age, sex ratio, body mass index, blood type, original liver disease, and CTP score between the pre- and post-MELD groups. However, there was a relatively large number of patients with HBV in the pre-MELD group and a relatively large number of patients with alcohol-induced hepatitis or fulminant hepatitis in the post-MELD group. Significant differences were observed in the MELD score (pre-MELD, 17.7 ± 9.3 vs. post-MELD, 36.2± 4.9; P < 0.001), and combined HCC ratio (pre-MELD, n = 9 [40.9%] vs. post-MELD, n = 2 [7.7%]; P = 0.006) between the 2 groups.
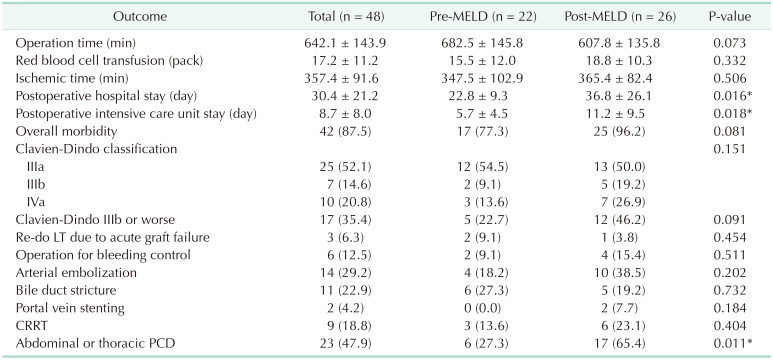
The perioperative and postoperative outcomes are listed in Table 2. No significant difference was observed in terms of operation time, transfusion of red blood cells, or ischemic time between the 2 groups. Significant differences were observed in terms of length of postoperative hospital stay (pre-MELD, 22.8 ± 9.3 days vs. post-MELD, 36.8 ± 26.1 days; P = 0.016) and length of postoperative intensive care unit stay (pre-MELD, 5.7 ± 4.5 days vs. post-MELD, 11.2 ± 9.5 days; P = 0.018) between the 2 groups.
No significant difference was observed in overall postoperative morbidity (pre-MELD, n = 17 [77.3%] vs. post-MELD, n = 25 [96.2%]; P = 0.081) and morbidity of Clavien-Dindo classification IIIb or worse (pre-MELD, n = 5 [22.7%] vs. post-MELD, n = 12 [46.2%]; P = 0.091) between the 2 groups. Three patients underwent liver retransplantation due to acute graft failure, and 6 patients underwent reoperation for post-liver transplantation bleeding control. No significant differences were observed in continuous renal replacement therapy or postoperative radiologic intervention procedures including arterial embolization, portal vein stenting, endoscopic retrograde cholangiopancreatography, percutaneous transhepatic biliary drainage, and abdominal or thoracic percutaneous drainage between the 2 groups.
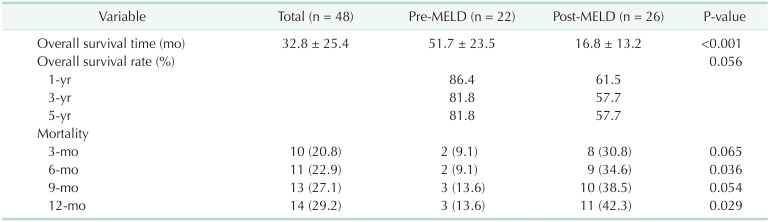
The overall survival rate and 3-, 6-, 9-, and 12-month mortality rates are showed in Table 3 and Figs. 1, 2. The overall survival time was 32.8 months in all patients. The survival time in the pre-MELD group was longer than that in the post-MELD group because of differences in the timing of DDLT (pre-MELD, 51.7 ± 23.5 months vs. post-MELD, 16.8 ± 13.2 months; P < 0.001). The 1-, 3-, and 5-year overall survival rates in the pre-MELD and post-MELD groups were 86.4%, 81.8%, and 81.8% and 61.5%, 57.7%, and 57.7%, respectively (P = 0.056). The 3-, 6-, 9-, and 12-month mortality rates in pre-MELD and post-MELD groups were 9.1%, 9.1%, 13.6%, and 13.6% and 30.8%, 34.6%, 38.5%, and 42.3%, respectively (P = 0.036 in 6-month mortality rate and P = 0.029 in 12-month mortality rate).
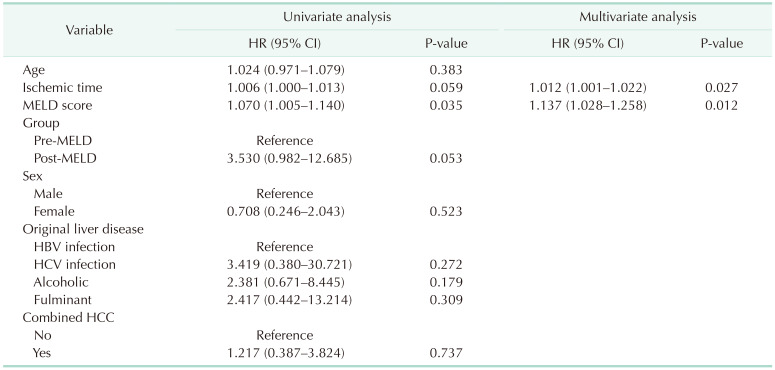
The Cox proportional hazards regression analyses are performed to identify which factor affected the 6-month mortality rate (Table 4). In univariate analysis, MELD allocation (hazard ratio [HR], 3.530; 95% confidence interval [CI], 0.982–12.685; P = 0.053), graft ischemic time (HR, 1.006; 95% CI, 1.000–1.013, P = 0.059), and MELD score (HR, 1.070; 95% CI, 1.070–1.140, P = 0.035) showed possible associations with 6-month mortality rate. In multivariate analysis, graft ischemic time (HR, 1.012; 95% CI, 1.001–1.022, P = 0.027) and MELD score (HR, 1.137; 95% CI, 1.028–1.258, P = 0.012) showed significant associations with 6-month mortality rate.
The MELD system is a useful indicator for predicting the prognosis of liver cirrhosis patients and has been studied extensively before its introduction [136]. Many efforts have been made to improve organ distribution in South Korea through the MELD system [4]. According to previous studies, the waiting mortality rate decreased after the introduction of the MELD system; however, the prognosis after liver transplantation was negative in terms of overall morbidity rate and overall survival rate [56]. A comparison of liver transplantation patients before and after the introduction of the MELD system in our center also showed similar results with those of other studies.
Patients who received DDLT after the MELD system implementation had higher MELD scores than those who received DDLT in the previous CTP system, and the length of hospital stay in the intensive care unit and the recovery period became longer. Dutkowski et al. [5] reported that the incidence of renal failure requiring kidney transplantation has increased, and the cost of disease treatment has also increased by 55% since the introduction of the MELD system. In addition, a single-center study similar to the current one showed a significantly higher readmission rate after the introduction of the MELD system in patients who underwent DDLT [6]. The overall survival was also longer in pre-MELD patients than in post-MELD patients due to a longer follow-up period. The 1- and 3-year survival rates after DDLT were not statistically significant; however, the overall survival rate of patients in the post-MELD group tended to be lower than those in the pre-MELD group. These suggest that the introduction of the MELD system adversely affected patients’ recovery and postoperative performance because of preferentially selecting patients with higher severity for DDLT.
Notably, after the introduction of the MELD system, the number of HCC patients selected for DDLT significantly decreased from 40.9% to 7.7% [69]. In contrast, the DDLT rate in alcoholic cirrhosis patients increased remarkably after the application of the MELD system [10]. In the case of HCC patients, additional points are given to the MELD score calculation; however, they will be eliminated from the waiting list due to HCC progression while waiting for DDLT. In addition, in HCC patients with preserved liver function, it is almost impossible to be selected for DDLT because their MELD score is relatively low [469]. This is a situation in which liver transplantation cannot be performed if HCC patients with preserved liver function cannot secure living donors. Therefore, HCC patients in the MELD system have a lower probability of being selected for DDLT compared to the CTP system. To solve this problem, introducing a quota for each disease may be considered when selecting a liver transplant recipient. This will contribute to compensating for the relative concentration of transplant recipients with alcoholic liver cirrhosis.
In the current as well as in previous studies [5611], the prognosis of patients who received DDLT after the introduction of the MELD system was worse prior to the introduction, and the overall survival rate also decreased. Thus, the MELD system is criticized for increasing medical costs and incidence of complications in patients [5]. However, as a more objective prognostic factor than the CTP system, the MELD system provides an opportunity for a liver transplant to critically ill patients first, thereby reducing the number of patients who die while waiting for a transplant [11], and many studies have shown the result of lowering the overall socioeconomic cost [612].
The deterioration of surgical performance and patient’s prognosis due to the introduction of the MELD system suggests that patients with higher severity were preferentially selected for DDLT. This is because the MELD system faithfully reflects the principle of priority for critical patients. However, it was also confirmed that there were clearly fewer opportunities for patients with HCC. In South Korea, an additional point system suitable for our environment is provided based on various statistical grounds for patients with HCC [46]. It is almost impossible for HCC patients who satisfy the Milan criteria to receive additional points and be selected for DDLT [10]. Therefore, additional system modifications are needed, such as introducing a quota for HCC patients other than bonus points for HCC patients. Moreover, according to a recent study, donation improvement programs can help increase organ donation [13].
In the current study, 3-, 6-, 9-, and 12-month mortality rates were compared between the pre-MELD and post-MELD groups. Significant differences were observed in 6-, and 12-month mortality rates between the 2 groups; post-MELD group had higher 6-, and 12-mortality rates than those of pre-MELD group. In both groups, most deaths occurred within 1 year after DDLT. The reasons for the difference in mortality rate between the 2 groups were related to the higher proportion of alcoholic liver cirrhosis patients in the post-MELD group and the MELD score difference between the 2 groups. A recent study reported that 6-month mortality in pre-MELD group (n = 77) and post-MELD group (n = 52) were 11.7% and 25.0%, respectively (P = 0.022) [14]. In multivariate analysis [14], MELD/CTP allocation was the only factor that showed significant association with higher 6-month mortality than the CTP allocation system (HR, 2.865; 95% CI, 1.057–7.764; P = 0.039). However, MELD score and organ ischemic time were classified as risk factors for 6-month mortality rate in the current study.
The most important problem after the introduction of the MELD system in South Korea is that the opportunity does not return to patients with HCC and to moderate-to-emergency patients who do not have a living donor. Due to the absolute shortage of brain-dead organ donors, the opportunity arises only in critically ill patients with a MELD score of 40 or more. Currently, the number of brain-dead organ donors per million in South Korea is 8.68, which is very low compared to 48.9 in Spain and 36.88 in the United States [1516]. This serious shortage of brain-dead donors appeared to be a phenomenon in which patients with high severity were mainly selected for DDLT after the introduction of the MELD system [17]. Therefore, unless the shortage of brain-dead organ donors is improved, it is predicted that the problem of distribution between transplants and HCC patients cannot be solved in the current MELD system.
Although the current study was a single-institution study with a small number of patient to make clear conclusions, it showed DDLT results before and after the MELD system from a low-mid volume center that were rarely reported. In addition, after the implementation of the MELD system, the characteristics and changes in the distribution of end-stage liver disease in the low-mid volume center were described. Through studies from various centers including low-mid volume centers comparing clinical results before and after the implementation of the MELD system, studies with high level of evidence such as meta-analysis can be conducted in the future.
In summary, the MELD system reflects the severity of patients requiring DDLT better than the CTP system. However, when there is a shortage of liver donors, the opportunity for DDLT is concentrated in patients with severe liver cirrhosis with high MELD scores, including alcoholic liver cirrhosis. This relatively reduced the chance of DDLT in patients with HCC. In addition, after the introduction of the MELD system, the incidence of complications and overall survival rates after DDLT tended to decrease. Thus, it is necessary to determine solutions to the reduced chances of DDLT in HCC patients due to a shortage of brain-dead organ donors.
Notes
References
1. Hong G, Lee KW, Suh S, Yoo T, Kim H, Park MS, et al. The model for end-stage liver disease score-based system predicts short term mortality better than the current Child-Turcotte-Pugh score-based allocation system during waiting for deceased liver transplantation. J Korean Med Sci. 2013; 28:1207–1212. PMID: 23960449.

2. Min SI, Ahn C, Han DJ, Kim SI, Chung SY, Lee SK, et al. To achieve national self-sufficiency: recent progresses in deceased donation in Korea. Transplantation. 2015; 99:765–770. PMID: 25226175.
3. Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000; 31:864–871. PMID: 10733541.

4. Kim MS. Modification of emergency status in deceased donor liver allocation: evidence for Korean Model of End-stage Liver Disease (MELD) system. J Korean Soc Transplant. 2016; 30:51–58.

5. Dutkowski P, Oberkofler CE, Béchir M, Müllhaupt B, Geier A, Raptis DA, et al. The model for end-stage liver disease allocation system for liver transplantation saves lives, but increases morbidity and cost: a prospective outcome analysis. Liver Transpl. 2011; 17:674–684. PMID: 21618688.

6. Lee JA, Choi GS, Kim JM, Kwon CHD, Joh JW. Comparison study of outcomes of deceased donor liver transplantation before and after Korean model for End-Stage Liver Disease (MELD) system: single center experience. J Korean Soc Transplant. 2018; 32:7–11.

7. Dunn W, Jamil LH, Brown LS, Wiesner RH, Kim WR, Menon KV, et al. MELD accurately predicts mortality in patients with alcoholic hepatitis. Hepatology. 2005; 41:353–358. PMID: 15660383.

8. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.
9. Freeman RB Jr, Gish RG, Harper A, Davis GL, Vierling J, Lieblein L, et al. Model for end-stage liver disease (MELD) exception guidelines: results and recommendations from the MELD Exception Study Group and Conference (MESSAGE) for the approval of patients who need liver transplantation with diseases not considered by the standard MELD formula. Liver Transpl. 2006; 12(12 Suppl 3):S128–S136. PMID: 17123284.

10. Kwon TJ, Kang W, Gwak GY, Paik YH, Choi MS, Lee JH, et al. Outcome of patients with severe alcoholic hepatitis after Model for End-Stage Liver Disease-based allocation system implementation in Korea. Korean J Transplant. 2021; 35:24–32.

11. Lee J, Kim DG, Lee JY, Lee JG, Joo DJ, Kim SI, et al. Impact of Model for End-stage Liver Disease Score-based allocation system in Korea: a nationwide study. Transplantation. 2019; 103:2515–2522. PMID: 30985735.

12. Cywinski JB, Mascha EJ, You J, Sessler DI, Kapural L, Argalious M, et al. Pre-transplant MELD and sodium MELD scores are poor predictors of graft failure and mortality after liver transplantation. Hepatol Int. 2011; 5:841–849. PMID: 21484127.

13. Heo SJ, Ju YH, Noh EJ, Kim KM, Son YK, Jung SW, et al. A study on the performance of the Donat ion Improvement Program in Korea. Korean J Transplant. 2021; 35:77–85.
14. Park HS, Lee JM, Hong K, Han ES, Hong SK, Choi Y, et al. Impact of Model for End-Stage Liver Disease allocation system on outcomes of deceased donor liver transplantation: a single-center experience. Ann Hepatobiliary Pancreat Surg. 2021; 25:336–341. PMID: 34402433.

15. Cho WH. Causes of donation failure and improvement measures analyzed based on data from domestic deceased donors in 2019. Korean J Transplant. 2020; 34:219–230.

16. Kwak BJ, Kim DG, Han JH, Choi HJ, Bae SH, You YK, et al. Clinical outcome of 1,000 consecutive cases of liver transplantation: a single center experience. Ann Surg Treat Res. 2018; 95:267–277. PMID: 30402445.

17. Park GC, Hwang S, Jung DH, Song GW, Ahn CS, Kim KH, et al. Is renal replacement therapy necessary in deceased donor liver transplantation candidates with hepatorenal syndrome?: a 2-year experience at a high-volume center. Ann Surg Treat Res. 2020; 98:102–109. PMID: 32051819.

Fig. 1
Kaplan-Meier curve for overall survival between the 2 groups. MELD, Model for End-Stage Liver Disease.
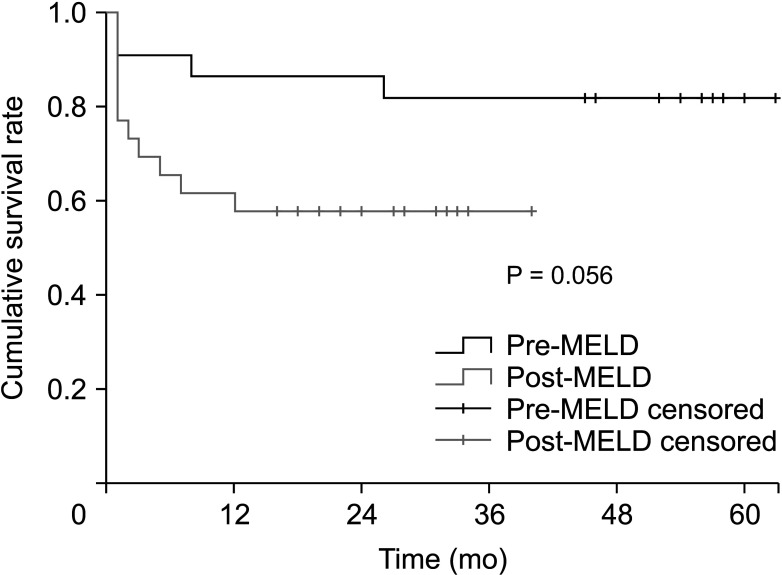
Fig. 2
Kaplan-Meier curve for 12-month survival between the 2 groups. MELD, Model for End-Stage Liver Disease.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download