INTRODUCTION
Acute appendicitis is the most common condition requiring emergency abdominal surgery worldwide, with a lifetime risk of 8.6% in males and 6.9% in males [
1]. Appendectomy is the standard treatment modality for appendicitis. For over a century, open appendectomy was the only standard approach for treating appendicitis. Laparoscopic appendectomy has become a standard procedure since it was first reported in 1983 [
2]. The development of laparoscopic techniques over time has led to the use of single-incision laparoscopic appendectomy (SILA) in addition to classical 3-incision laparoscopic appendectomy (TILA) [
3]. The merits of SILA include excellent cosmetic results because scarring is scarcely visible as the incision is made only along the navel and the surgical procedure is performed through this single incision.
However, SILA requires a large skin incision measuring approximately 3 cm in length and extending to the fascia, since this single incision must permit simultaneous entry of the camera and several instruments during surgery. The size of the incision wound associated with SILA is evidently very large, given that the largest incision for TILA measures 12 mm. Several prospective randomized controlled trials have compared SILA and TILA. Numerous studies reported that the intensity of postoperative pain was considerably greater with SILA than that with TILA [
456]. The interim analysis in another study showed that the pain was significantly more severe after SILA, leading to discontinuation of the study [
5]. One study reported that although there was no difference during resting state, the pain intensity was higher when exercising or coughing after SILA [
7]. In contrast, some studies found no difference in the pain associated with SILA and TILA. Additionally, a recently published meta-analysis found no difference in the pain associated with the 2 surgeries [
8]. We reported that SILA is significantly less painful than TILA based on a retrospective study conducted at our institution [
9]. Therefore, the difference in the pain associated with SILA and TILA remains controversial. This may be because the incision for SILA is large in size, while the incision for TILA is large in number.
We devised a method to reduce the size of the main incision wound on the navel to minimize postoperative pain and maximize cosmetic results. We named the procedure “needle grasper-assisted single-incision laparoscopic appendectomy” (NASILA). A retrospective study found that NASILA induced lesser pain, required a shorter operative time, and provided similar cosmetic results when compared to SILA. Therefore, it was concluded that the pain would be minimized, and the procedure would be performed more easily using the NASILA approach [
10].
However, the previous study was limited by its retrospective design, and the surgical method was determined according to the operator's discretion. Therefore, the present study was conducted to compare the operative and postoperative outcomes of NASILA and SILA using a prospective randomized clinical trial.
Go to :

METHODS
Study design
This prospective randomized controlled study was conducted to evaluate the operative and postoperative outcomes of NASILA for acute appendicitis. The study was approved by the Institutional Review Board of Chung-Ang University Hospital (No. 1781-001-291) and was registered with Clinical Research Information Service (
cris.cdc.go.kr; ID, KCT0002746). Each patient was informed about the investigational nature of the trial and received detailed information about the study protocol. Written informed consent was obtained from each participant before enrollment in the trial.
Eligibility and exclusion criteria
Patients who were diagnosed with acute appendicitis based on clinical examination, CT, or ultrasonography, and aged above 19 years were included in this study. Patients with appendicitis with overt perforation or periappendiceal abscess were excluded. Cases that were rendered difficult owing to a previous abdominal surgery and pregnant patients were also excluded.
Randomization
Randomization was performed using the random number table method following stratification of the usage of patient-controlled anesthesia (PCA). The patients and pain raters were blinded to the appendectomy procedure. The SILA and NASILA groups underwent stratification-randomization in a 1:1 ratio.
Withdrawal criteria
The case was included in the conversion rate and the patient was not included in subsequent evaluation if the surgical method was altered (extra trocar insertion, conversion to laparotomy, or additional surgery other than appendectomy [cecectomy, etc.]). The patient was not included in the evaluation of cosmetic satisfaction with the scar if a drainage tube was placed, because it was deemed necessary based on the surgical findings. Patients with wound infection complications were excluded from the evaluation of cosmetic satisfaction with scars. If a participant expressed his/her intention to opt out of the study, he/she was withdrawn from the study and all data were excluded.
Interventions
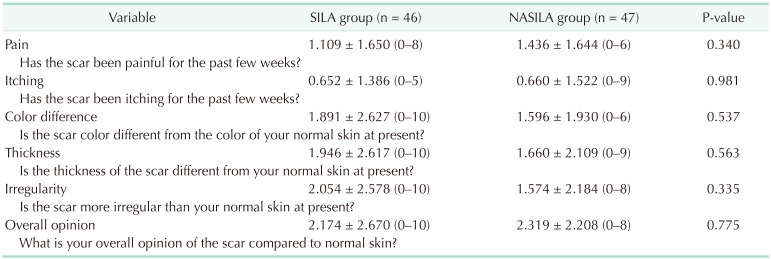
A transumbilical incision measuring approximately 2.5 cm was made for SILA, and the fascia was incised about 3 cm in length. A glove port (NELIS Corp., Bucheon, Korea) was placed through the incision. A 5-mm laparoscopic camera and 2 laparoscopic instruments were introduced through the glove port. The appendectomy procedure was performed (
Fig. 1). Cecectomy was performed with a linear stapler in case of severe inflammation at the base of the appendix. A closed suction drain was inserted in the event of obvious contamination [
10].
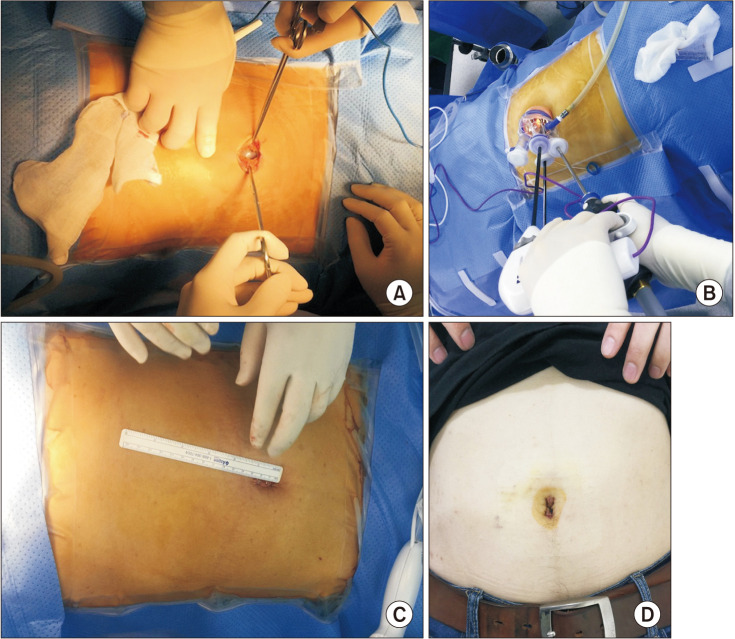 | Fig. 1Single-incision laparoscopic appendectomy. (A) An about 2.5-cm transumbilical incision is made. (B) Glove port (NELIS Corp., Bucheon, Korea) was introduced through the umbilical incision. Laparoscopy (5 mm) and instruments were introduced through the glove port. (C) About 2.5 cm-sized wound at the end of the operation. (D) A scar on postoperative 1 week.
|
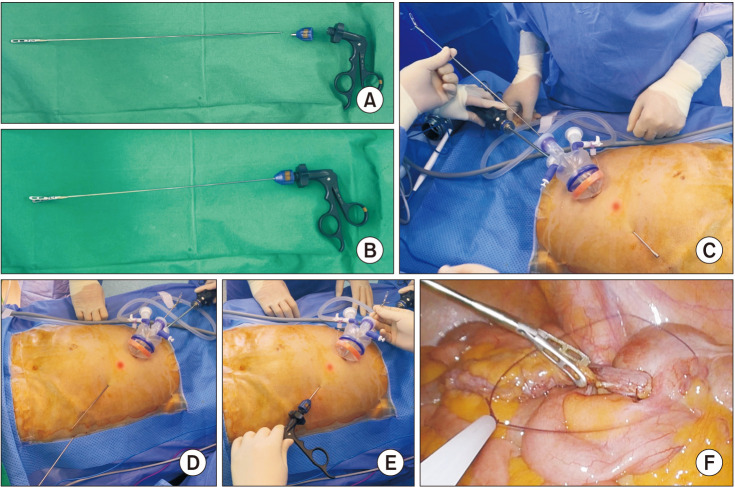
A small umbilical incision through which only a 12-mm trocar could be loaded was made for the NASILA procedure. A 12-mm trocar was introduced using the open technique and pneumoperitoneum was induced using CO
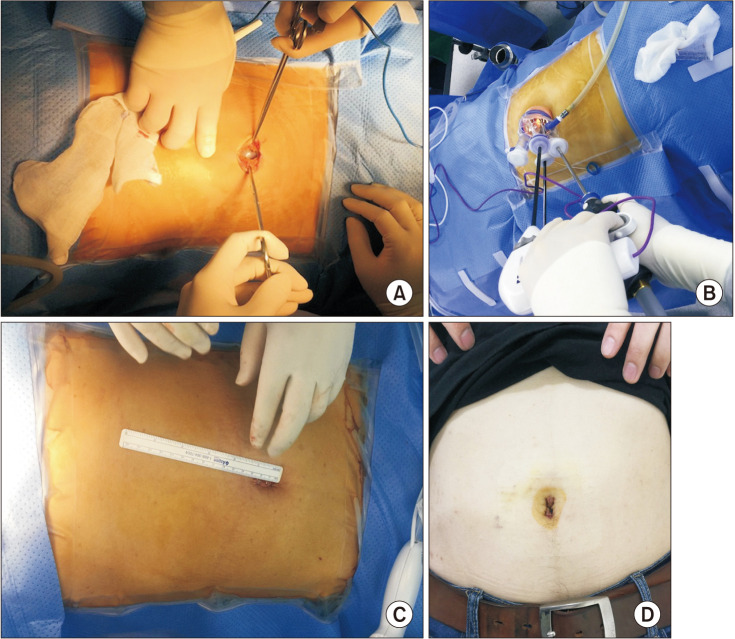
2 gas. A pediatric glove port was inserted immediately after removing the 12-mm trocar. Subsequently, an approximately 2.5-mm long incision was made along the suprapubic area and a needle grasper (Endo Relief, Hirata Precisions Corp., Kamagaya, Japan) was inserted through the tiny wound under laparoscopic visualization (
Fig. 2). The appendectomy procedure, cecectomy, and drain placement protocols were the same as those employed for SILA (
Fig. 3) [
10].
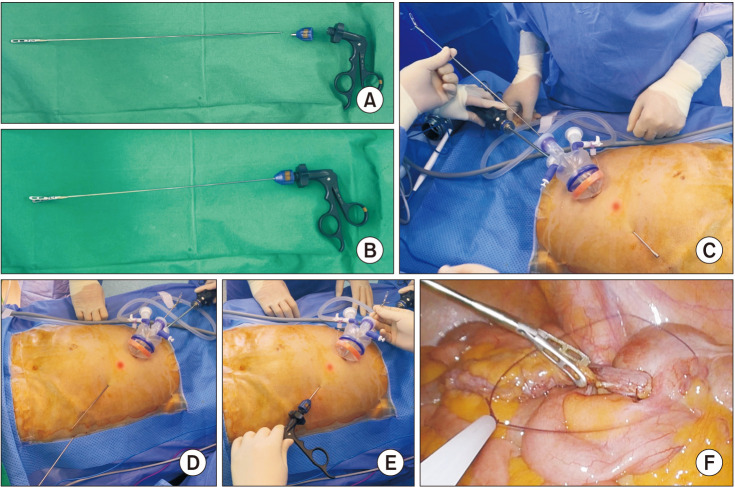 | Fig. 2Characteristics of needle grasper (Endo Relief, Hirata Precisions Corp., Kamagaya, Japan). (A) The needle grasper consists of 3 parts. One is the shaft and the jaws, it has a handle, and there is a part that connects the 2 parts. The shaft is 2.4-mm thick and the jaws are the same as the jaws of the 5-mm instrument. (B) It is used by assembling 3 parts. It is joined after passing through the abdominal wall for mounting through a small wound in the abdominal wall. (C) A guide tube enters through the abdominal wall and exits through the trocar. Align the guide tube with the needle grasper so that the handle side of the needle grasper's shaft comes out through the abdominal wall. (D) The guide tube is separated from the needle grasper. (E) The handle is connected, and the needle grasper is ready to use. (F) The needle grasper can handle tissue like any other 5-mm instrument.
|
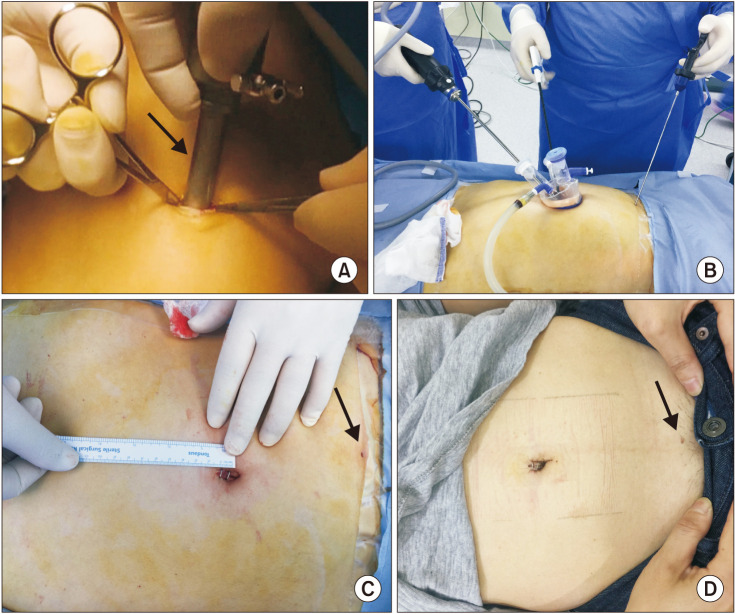 | Fig. 3Needle grasper-assisted single-incision laparoscopic appendectomy. (A) Small umbilical incision in which only a 12-mm trocar can be loaded is made. The arrow is a 12-mm reusable trocar. (B) Pediatric glove port (NELIS Corp., Bucheon, Korea) is applied, and a needle grasper is introduced on the suprapubic area through a 2.5-mm wound. (C) About 1.3-cm main wound and about 3-mm needle grasper site wound at the end of the operation. The arrow is the wound for the needle grasper. (D) Scar on postoperative 1 week. The arrow indicates scar of the wound for the needle grasper.
|
Postoperative pain control was based on the same criteria in both groups and was achieved using PCA or tramadol 50 mg injection 3 times a day according to the patient's prerandomization choice. We recorded the number of times the patient pressed the PCA button. Additional analgesics were used when the numerical pain intensity score (NPIS) exceeded 3. We also recorded the frequency of injection and dose of the additional analgesic.
Endpoints
The degree of pain immediately after surgery, i.e., when the patient arrived at the ward from the operating room, constituted the primary endpoint. NPIS was determined immediately after the patient was shifted to the bed. Both patients and nurses were blinded to randomization results. The NPIS requires the patient to rate their pain on a defined scale. For example, 0–10 where 0 is no pain and 10 is the worst pain imaginable.
The secondary endpoints included operative time (main operative time and total operative time), NPIS-max (highest degree of pain experienced by the patient on a given day among those checked regularly every 8 hours and those checked additionally when patient complained of pain), complete blood count, CRP level at postoperative day 1, and cosmetic satisfaction with the surgical wounds 1 month after surgery (telephone questionnaire). The dose and frequency of injection of the additional analgesic, numerical rating score for postoperative nausea, frequency of antiemetics, and length of hospitalization (in days) were also evaluated.
For the evaluation of scars, phone interviews were conducted using a modified form of the patient scale in the Patient and Observer Scar Assessment Scale. We asked 6 questions: 2 on scar symptoms (pain and itching), 3 on differences from normal skin (the color, thickness, and irregularity of the scar), and the overall opinion compared to normal skin. The scar symptoms were scaled from 0 (“no, not at all”) to 10 (“yes, very much”). The difference from normal skin was scaled from 0 (“no, as normal skin”) to 10 (“yes, very different”). The overall opinion was also scaled from 0 (“as normal skin”) to 10 (“very different”).
Sample size and statistical analysis
This study was designed to test the hypothesis that NASILA is superior to SILA in relieving postoperative pain. The NPIS (mean ± standard deviation [SD]) associated with SILA has been reported by various clinical studies, as 3.9 ± 1.3, 2.77 ± 1.14, and 2.76 ± 1.64, respectively [
6911]. Since the current study utilized the pain score obtained immediately after transferring the patient to the ward following surgery as the primary endpoint, it is plausible that it may be slightly higher than that recorded by previous studies. Therefore, the mean and the SD of pain score for SILA was estimated to be 4.0 ± 1.7. The post-NASILA pain score was anticipated to be 1 point lower than the post-SILA score. We calculated that a sample of 104 patients would be required, with 52 each in each group to achieve a significance level (α) of 0.05 and statistical power of 85% based on the t-test. The dropout rate was not expected to be very high, given the short follow-up duration. Fifty-five patients were required in each group, assuming a dropout rate of 5% in both groups.
We analyzed the distribution of each variable in the 2 groups using the t-test for continuous variables and the chi-square test for categorical variables. All statistical analyses were performed using IBM SPSS Statistics ver. 23.0 (IBM Corp., Armonk, NY, USA). P-values of <0.05 indicated statistically significant differences.
Go to :

RESULTS
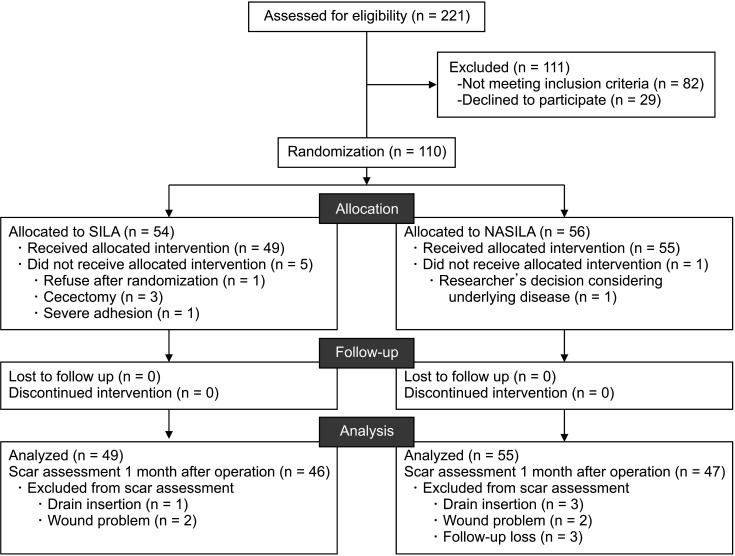
This study enrolled 110 patients between December 2017 and August 2018. A total of 54 patients were allocated to the SILA group and 56 to the NASILA group. Open conversion or additional incisions were not required in either group. Six patients withdrew from the study. Three of these patients withdrew because they required additional surgery (cecectomy) besides appendectomy. One patient withdrew owing to severe adhesion, while another withdrew owing to underlying heart disease based on the researcher's decision. One patient refused to participate in the study after randomization. Finally, 49 patients who underwent SILA and 55 patients who underwent NASILA were evaluated (
Fig. 4).
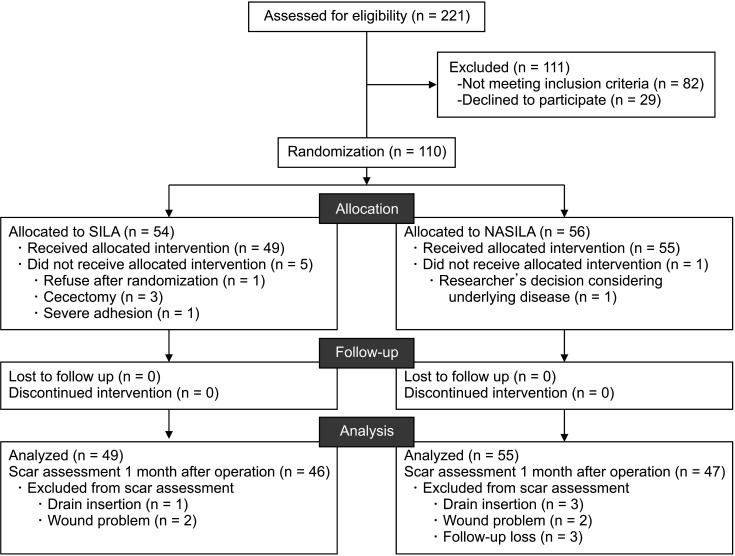 | Fig. 4CONSORT (Consolidated Standards of Reporting Trials) flow. SILA, single-incision laparoscopic appendectomy; NASILA, needle grasper-assisted single-incision laparoscopic appendectomy.
|
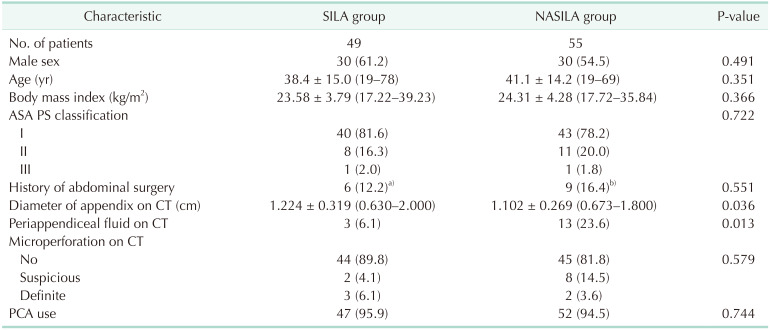
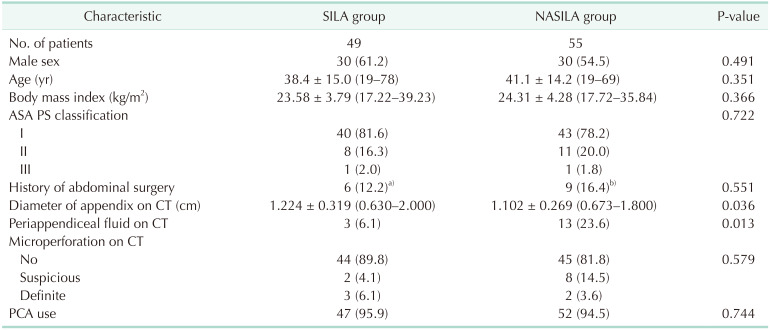
The participants were evenly allocated with respect to sex, age, body mass index, American Society of Anesthesiologists physical status classification, history of abdominal surgery, and PCA use. The diameter of the appendix was larger in the SILA group than that in the NASILA group. Periappendiceal fluid was observed more frequently on CT in the NASILA group than that in the SILA group. The finding of microperforation on CT was not significantly different between the 2 groups (
Table 1).
Table 1
Participants' baseline characteristics

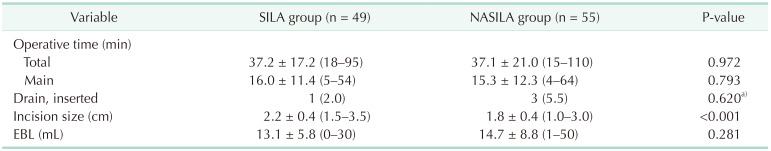
The operative outcomes are summarized in
Table 2. The size of the main incision wound was significantly smaller in the NASILA group than that in the SILA group (mean ± SD, 1.8 ± 0.4 cm
vs. 2.2 ± 0.4 cm; P < 0.001). The operative time (total or main), drain insertion rate, and amount of estimated blood loss did not differ significantly between the 2 groups.
Table 2
Operative outcomes
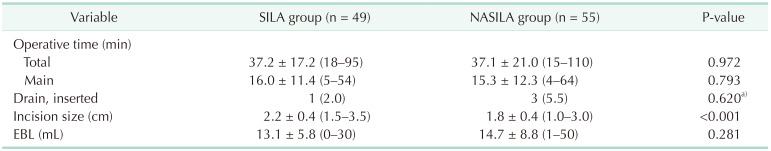

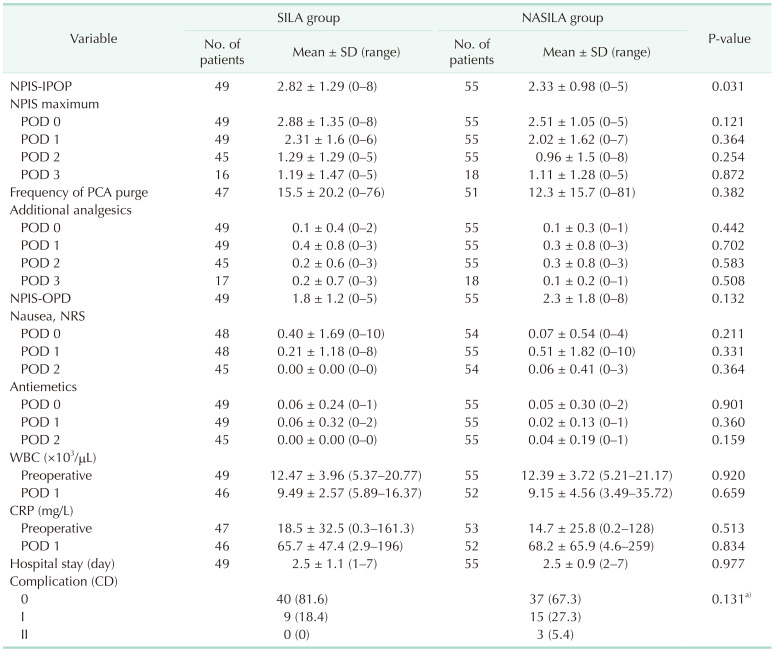
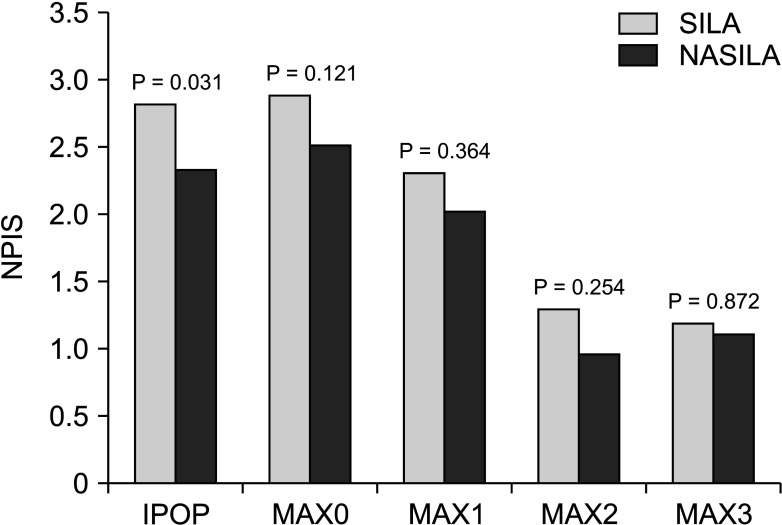
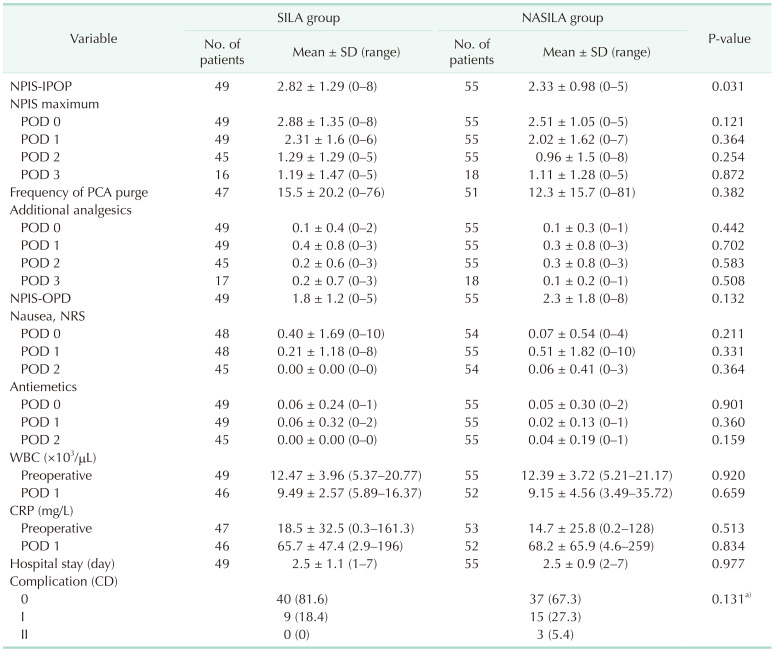
Table 3 presents postoperative outcomes of the study cohort. The immediate postoperative NPIS, i.e., the primary endpoint, was significantly lower in NASILA group than in SILA group (mean ± SD, 2.33 ± 0.98
vs. 2.82 ± 1.29; P = 0.031). However, the maximal NPIS on each postoperative day did not differ significantly between the 2 groups. The NPIS scores were plotted on a graph, which showed that the post-NASILA NPIS score was slightly lower, except for the 3rd day; however, there was no significant difference between the NASILA and SILA groups except during the immediate postoperative period (
Fig. 5). There was no significant difference in the frequency of PCA purge by pushing the button, and the administration of additional analgesics between the NASILA and SILA groups. There was no significant difference in the NPIS at the outpatient visit after discharge. There was no difference in the degree of nausea and dose of antiemetics between the 2 groups. Inflammatory markers, including WBC and CRP levels, did not differ significantly between the 2 groups. The duration of hospitalization also did not differ between the NASILA and SILA groups. The postsurgical complications, which were evaluated using the Clavien-Dindo classification, were not significantly different between the 2 groups. The most frequent complication was postoperative fever, which was controlled using antipyretics. Three grade II complications were observed in the NASILA group, including skin eruption, arrhythmia, and urinary retention.
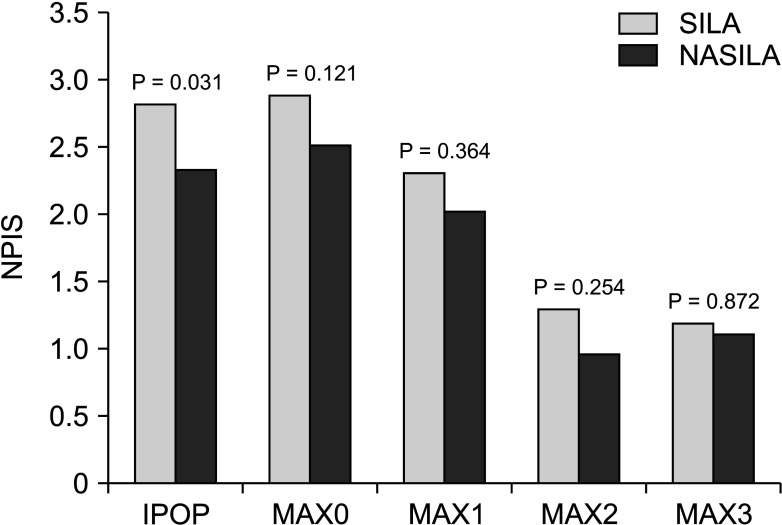 | Fig. 5Degree of postoperative pain. IPOP, immediate postoperative (pain score right after transfer to the ward from the operating room); MAX#, maximum pain score at postoperative day #; SILA, single-incision laparoscopic appendectomy; NASILA, needle-assisted single-incision laparoscopic appendectomy.
|
Table 3
Postoperative outcomes

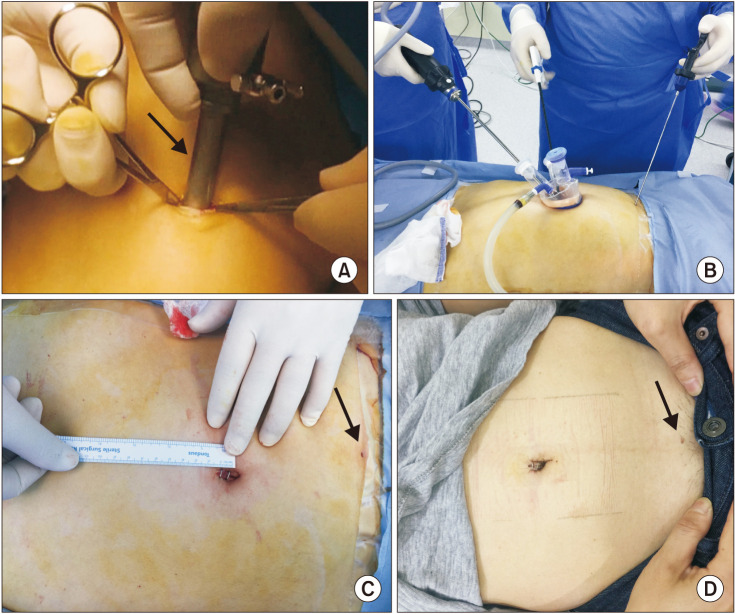
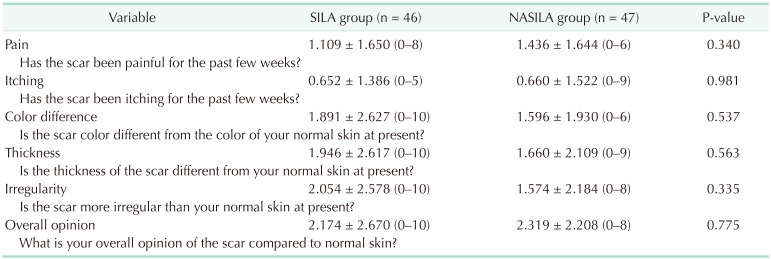
Questionnaire for scar
Ninety-three patients (46 in the SILA group and 47 in the NASILA group) responded to the telephonic interviews for scar evaluation 1 month after surgery. There were no significant differences in pain sensation and itching, or any difference from normal skin with respect to color, thickness, and irregularity. Moreover, the overall opinion of the scar did not differ significantly between the 2 groups (
Table 4).
Table 4
Complaints regarding the scar 1 month after surgery

Go to :

DISCUSSION
The pain score measured immediately after transfer to the ward after surgery, which was used as the primary endpoint, was significantly lower in the NASILA group (mean ± SD, 2.33 ± 0.98
vs. 2.82 ± 1.29; P = 0.031). Moreover, the size of the main wound was significantly smaller in the NASILA group (mean ± SD, 1.8 ± 0.4 cm
vs. 2.2 ± 0.4 cm; P < 0.001). Laparoscopic appendectomy has replaced open appendectomy owing to its considerable advantages [
12]. For more than a decade, SILA has emerged as the preferred technique, since it yields better cosmetic outcomes [
3]. However, since SILA involves the creation of only one wound, albeit a large one, it is reportedly associated with greater pain compared to conventional TILA [
13]. Moreover, performing the procedure through one incision may lead to procedural difficulties during SILA due to the interference between instruments. These problems limited the widespread use of SILA. Therefore, we devised the NASILA technique, which minimizes the size of the main wound and adds a needle grasper to make the procedure easier. A retrospective study revealed the feasibility of NASILA with respect to the lower intensity of postoperative pain and shorter surgical time compared to SILA [
10]. The present study intended to prospectively evaluate the outcomes of NASILA. Our study resulted that NASILA reduced the size of the main wound and the pain score after surgery.
A difference of about 1 point in the NPIS was expected while calculating the sample size. However, the difference was 0.49 points after the final analysis in this study, i.e., it did not reach 1 point. We attributed the lower-than-expected pain scores to the following. This study was planned because we assumed that the pain would be highly intense immediately after the procedure; however, this was not the case (the pain was not as great as expected) because patients were transferred to the ward from the recovery room under sufficient pain control. Additionally, since the hospital's pain management policy stipulates that analgesia is mandatory if the NPIS score is 4 or higher, most patients were transferred under adequate pain control with NPIS scores of less than 4 points. PCA was performed in most patients, which means that sufficient analgesia was administered to most patients. Even in this situation, a small but significant difference definitely represents a meaningful result. Subsequently, there was no significant difference in the maximum NPIS scores for each day, which may be attributed to sufficient pain control. Future studies that include patients who are not administered PCA are necessary, because the side effects of PCA, including nausea, are not entirely rare. Thus, if pain can be minimized by limiting the wound size, postoperative management without PCA may be possible. Therefore, we opine that NASILA is the best surgical method for minimizing pain by limiting the incision wound.
Another advantage of NASILA is that there is less interference between the surgical tools, which makes surgery more convenient than SILA. SILA is associated with considerable interference between several instruments, including cameras, which are inserted through a single hole. However, only one camera and device are inserted through the main wound in NASILA. Subsequently, a small wound is made separately, through which the needle grasper is inserted, which does not require suturing and becomes obscure after some time. Therefore, there is little interference between the instruments, and the angle available for the movement of the devices is wide, which makes the procedure more comfortable for the operator. Moreover, the needle grasper used in our method is distinct from the device used in other studies [
1415]. Because the grasping jaw is similar to that of a 5-mm instrument, no problems are encountered while grasping and maintaining the tissue in traction (
Fig. 2). Our previous retrospective study demonstrated this convenience in the form of a shortened operative time [
10]. However, no reduction in the operative time was observed in this study. Unlike the previous study, this study excluded patients with severe inflammation, which makes it appear as if was no substantial difference that could demonstrate the technical convenience quantitatively. Moreover, except for one surgeon, the remaining surgeons mainly had performed SILA before this study, necessitating adaptation to the NASILA procedure.
A previous retrospective study also demonstrated that NASILA is not inferior to SILA from the cosmetic perspective [
10]. As the main wound is subsequently obscured in the navel after both procedures, NASILA cannot be cosmetically superior to SILA. Therefore, NASILA, which entails the creation of an additional wound beside the navel incision, is acceptable, if not inferior. However, since the additional wound on the abdominal wall in NASILA is very small and becomes almost invisible later, it did not have a substantial impact on the cosmetic aspect. Thus, this prospective study showed that NASILA was not cosmetically inferior to SILA (
Table 4).
This study was conducted with the participation of surgeons who mainly performed SILA surgery and a surgeon who developed NASILA and mainly performed NASILA. Therefore, it has the advantage of being less likely to induce a biased result in a certain group. Another strength of this study is that the participants and the pain scale measurer were blinded. Practically, dressing materials were applied to the umbilicus incision site and suprapubic area regardless of the presence of incision in all patients, so that it was not known which group they were allocated in.
The fact that a pain score, which can be said to be very subjective, was used as an endpoint can be seen as a weakness of this study. However, if the wound size, which is an objective indicator, is analyzed as an endpoint, it is not worth conducting the study because there will of course be a difference. In addition, although NPIS is subjective, it is considered to be sufficient as an endpoint because it is used as one of the main indicators to monitor patients clinically. In addition, as mentioned above, the blinding method was used to exclude subjective interference as much as possible.
It is a weakness of this study that the difference between the 2 groups was not as large as was estimated at the time of study planning because the overall pain was not as great as expected at the research planning stage. Also, there may be questions about whether a difference of about 0.5 points in NPIS would have any clinical significance. However, if you have a pain management policy that uses a score of 4 points as an additional analgesic administration criterion, then if you lower the average score by 0.5 points in patients who express around the 3 points of NPIS, it is highly likely that you can reduce the use of analgesics, and pain management may be easy even without the use of PCA. In the future, it will be necessary to study the effects of NASILA without using PCA to reduce the side effects of using PCA.
The fact that only patients with mild inflammation were included can be both a strength and a weakness of this study. In the patient with perforated appendicitis, it would have been difficult to evaluate the pain of the surgical wound itself due to the subjective effect on the pain felt after surgery because the intensity of pain felt before surgery was severe. Consistency in pain score evaluation could be expected by limiting to subjects with mild inflammation. However, it is a pity that the technical advantages of NASILA compared to SILA are not well emphasized due to the low difficulty of the operation itself. In the future, it is necessary to study the technical merits of NASILA in cases with high surgical difficulty with severe inflammation.
In conclusion, NASILA could attenuate postoperative pain by minimizing the size of the surgical wound. Furthermore, the cosmetic outcome with NASILA is comparable to that with SILA. Therefore, it can be considered as an option to aid early recovery and to improve the quality of life after surgery. If physicians are reluctant to use SILA owing to complaints of postoperative pain, NASILA may be considered.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download