Abstract
Purpose
Splenic flexure colon cancer (SFCC) is a rare disease that accounts for 2%–8% of colorectal cancers, and the extent of surgery and resection is still debatable. There have also been few studies on the safety and feasibility of laparoscopic surgery for SFCC. The purpose of this study is to evaluate outcomes and prognoses of surgery for SFCC.
Methods
We included patients with stage 1 to 3 who had undergone laparoscopic surgery for distal transverse-to-sigmoid colon cancer at 2 hospitals from March 2004 to December 2016 and collected data by retrospective design. We defined SFCC as being cancer between distal transverse and proximal descending colon. The short- and long-term outcomes of the anterior resection (AR) group (those patients who had undergone laparoscopic AR for mid and distal descending to sigmoid colon cancer) and the left colon resection (LR) group (those who had undergone laparoscopic segmental left colectomy for SFCC) were compared using propensity score matching.
Results
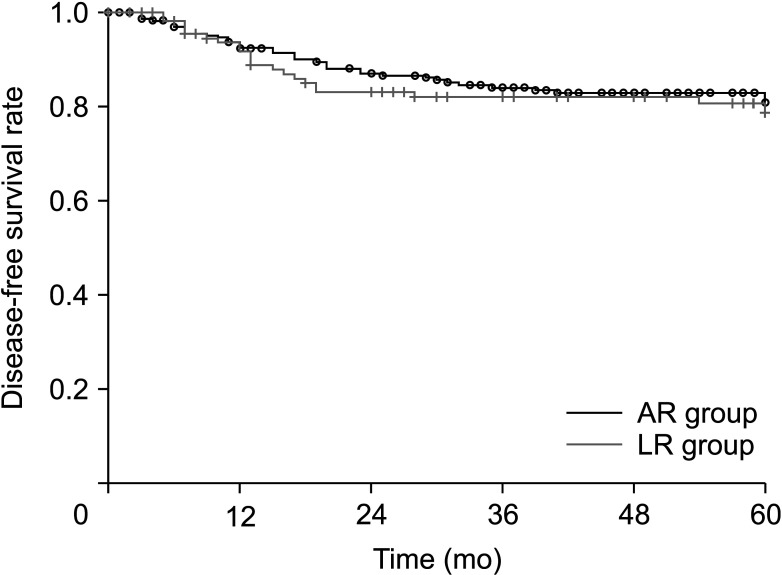
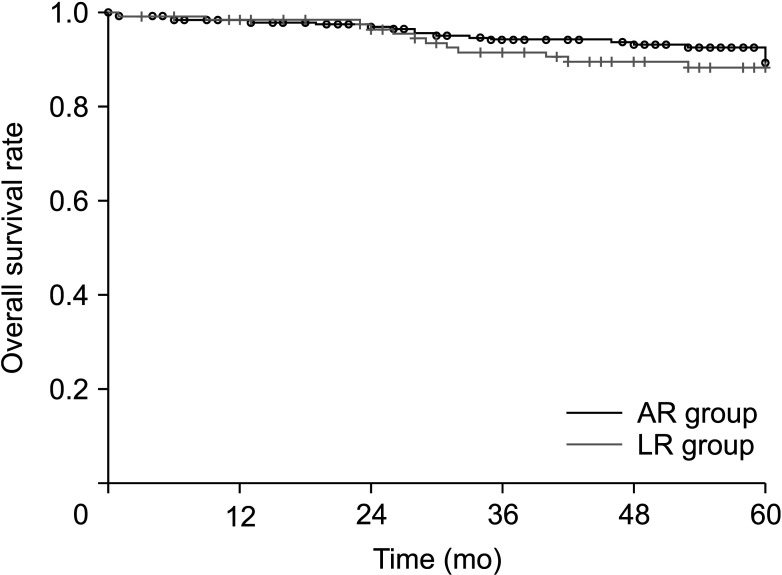
The median follow-up period was 60 months. The numbers of subjects in the AR and the LR groups were 948 and 118. After 2:1 propensity score matching, 236 vs. 118 patients were selected. There was no significant difference in 5-year disease-free survival (80.7% vs. 78.6%, P = 0.607), and both the 5-year overall survival (89.2% vs. 88.2%, P = 0.563) as well as short-term outcomes showed no statistical difference in most of the variables.
The incidence of splenic flexure colon cancer (SFCC) is less than 10% of all colorectal cancers. It has a relatively poor prognosis in advanced stages and with obstructive presentations because of its late detection compared to other colon cancers [1234].
For this reason, research on the prognosis and surgical outcomes for SFCC is rare. And there is only limited evidence for established surgical procedures or the extent of resection for SFCC. One study about approaching SFCC surgically reported that there is no difference in long-term outcomes regardless of the procedure used: (1) extended right colectomy, (2) left colectomy (ligation of the inferior mesenteric artery [IMA] and the left branch of the middle colic artery), or (3) segmental left colectomy (ligation of the left colic artery and left branch of the middle colic artery) [1]. Another paper reported that in cases of descending colon cancer, the group without IMA ligation has no difference in survival rates as compared to the ligation group [5].
The purpose of this study is to demonstrate the oncologic safety of segmental left colectomy for SFCC. The molecular biology of these tumors is almost the same from distal transverse-to-sigmoid colon because they all originate in the hindgut [678]. Therefore, we compared the long-term outcome of laparoscopic segmental left colectomy for SFCC and laparoscopic anterior resection (AR) for mid to distal descending and sigmoid colon cancer.
In addition, surgery for SFCC is technically challenging as compared to surgeries done for colon cancer in other sites. There is not sufficient evidence on whether laparoscopic surgery for SFCC is safe and feasible. Therefore, to demonstrate the technical safety and feasibility of laparoscopic segmental left colectomy for SFCC, we compared it with laparoscopic AR for mid to distal descending and sigmoid colon cancer.
In this study, SFCC is defined as cancer located from the distal third of transverse colon to the proximal third of the descending colon [123]. We retrospectively analyzed a total of 1,066 consecutive patients who had undergone laparoscopic segmental left colectomy for primary SFCC (left colon resection [LR] group, n = 118) and laparoscopic AR for primary mid to distal descending and sigmoid colon cancer (AR group, n = 948) between March 2004 and December 2016 at St. Vincent Hospital and Incheon St. Mary’s Hospital, affiliated with The Catholic University of Korea. Exclusion criteria were as follows: (1) stage IV colon cancer, (2) double primary cancer, (3) nonadenocarcinoma, and (4) emergent surgery such as obstruction or perforation.
Five experienced laparoscopic colorectal surgeons performed all surgeries. In both procedures, 5 trocars were used in a medial-to-lateral approach. Umbilical extension was done to extract the specimens. In all cases of mid to distal descending and sigmoid colon cancer, the surgeons performed laparoscopic AR with high ligation of the IMA. Mobilization of the splenic flexure colon was performed selectively for tension-free anastomosis. In most cases, the anastomosis was done by the end-to-end method using a double stapling technique. For SFCC, laparoscopic segmental left colectomy was performed. The origins of the left colic artery and the left branch of the middle colic artery were ligated (Fig. 1). The anastomosis method was at the surgeons’ discretion.
R software ver. 4.0.0 (R Foundation for Statistical Computing, Vienna, Austria) was utilized as a statistical tool. Independent t-test, chi-square test, and Fisher effect test were adjusted for statistical analysis. The P-values of <0.05 were considered to be significant. The propensity score matching (PSM) method was used to reduce bias in retrospective research in which we were unable to conduct a randomized control study [9]. The propensity score was calculated by implementing bivariate logistic stress. The PSM was performed for both the AR and LR groups using the nearest neighbor method on a 2:1 proportion. Variables considered for matching included age, sex, body mass index, American Society of Anesthesiologists physical status classification, CEA level (more than 5 ng/mL or none), history of previous abdominal surgery, stent insertion, en bloc resection, R0 resection, tumor size, T stage, N stage, TNM stages, lymphatic invasion, vascular invasion, perineural invasion, tumor grade, and adjuvant chemotherapy. After matching, statistical analysis was used to compare the 2 groups using the same method. Primary outcomes were 5-year disease-free survival (DFS) and 5-year overall survival (OS). Survival analysis utilized the Kaplan-Meier graph. Secondary outcomes were short-term outcomes.
The study’s protocol was reviewed and approved by the Institutional Review Board of St. Vincent Hospital and Incheon St. Mary’s Hospital (No. XC20RIDI0032) and the informed consent was waived.
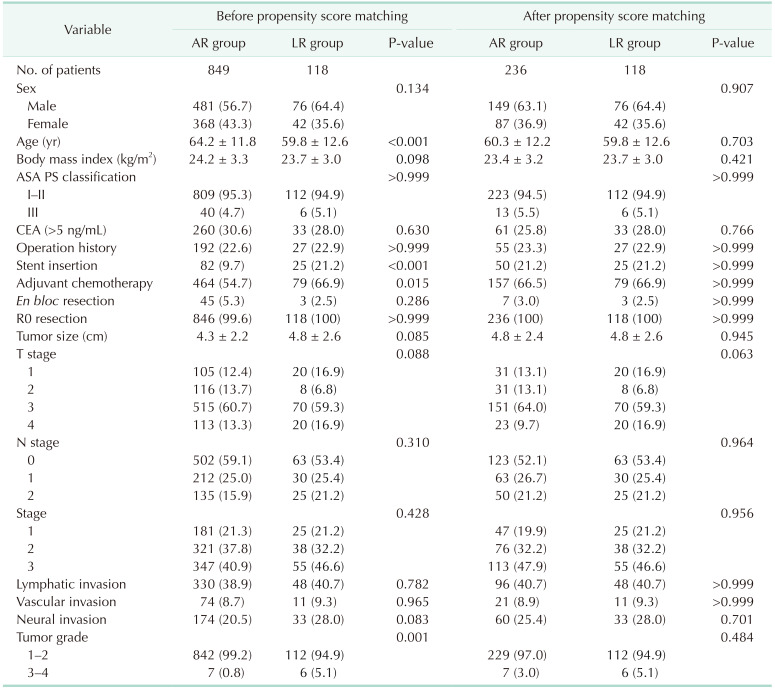
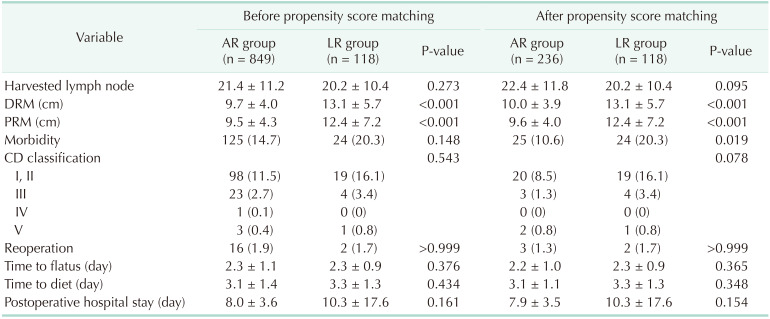
Out of the total 1,066 patients, the AR group accounted for 948 and the LR group accounted for 118. After a 2:1 PSM, the AR group had 236 and the LR group had 118. Table 1 shows the patients’ demographics and cancer characteristics. Before PSM, there were significant differences in age (64.2 years vs. 59.8 years, P < 0.001), rate of stent insertion (9.7% vs. 21.2%, P < 0.001), rate of adjuvant chemotherapy (54.7% vs. 66.9%, P = 0.015), and tumor grade (P = 0.001). However, after PSM, there was no significant difference between the 2 groups. The en bloc resected organs in the AR group consisted of bladder (3 cases), retroperitoneal fat (2 cases), abdominal wall (1 case), and ovary (1 case). In the LR group, they were stomach (1 case), retroperitoneal fat (1 case), and abdominal wall (1 case).
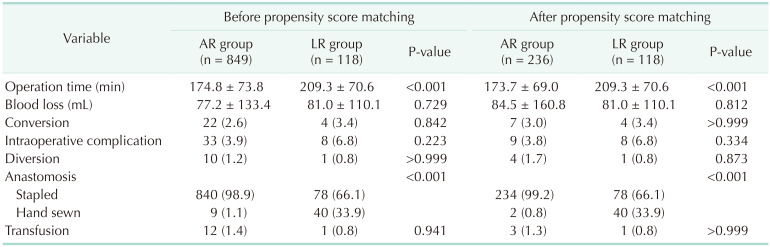
Table 2 shows the operative data. After PSM, the LR group operation time was longer than in the AR group (173.7 minutes vs. 209.3 minutes, P < 0.001). And the LR group had a higher hand-sewn anastomosis ratio than did the AR group (0.8% vs. 33.9%, P < 0.001). The intraoperative complications in the AR group were stapler failure (4 cases) and injury of adjacent organ (5 cases: spleen, pancreas, descending colon, marginal artery, and ureter) and in LR groups, they were bleeding (2 cases) and adjacent organ injury (6 cases: 4 transverse colon, 1 jejunum, and 1 spleen).
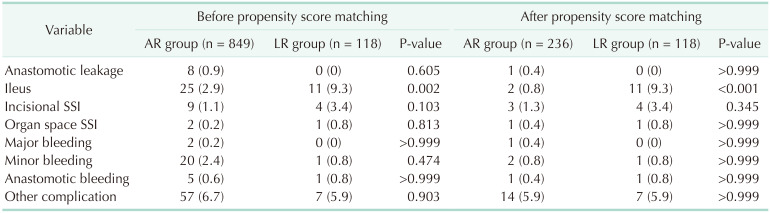
Tables 3 and 4 show the short-term outcomes. After PSM, the proximal and distal resection margins in LR group are longer than in the AR group (P < 0.001). The LR group had greater morbidity than did the AR group (10.6% vs. 20.3%, P = 0.019). This difference is because of minor morbidity (Clavien-Dindo classification I and II) and specifically because of ileus (0.8% vs. 9.3%, P < 0.001). The mortality rate was similar in both groups (1 aspiration pneumonia, 1 myocardial infarct in the AR group, and 1 myocardial infarction in the LR group).
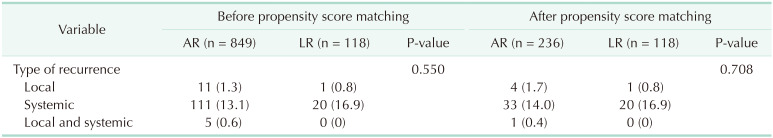
There was no significant difference in long-term outcomes between the 2 groups after PSM (Figs. 2, 3). The median follow-up duration was 60 months. The 5-year DFS in the AR and LR groups was 80.7% and 78.6% (P = 0.607). The 5-year OS rate in the AR and LR groups was 89.2% and 88.2% (P = 0.563). There was no significant difference in the pattern of recurrence (Table 5). In both groups, most recurrences were systemic.
The aim of this study is to demonstrate the oncologic and technical safety of laparoscopic segmental left colectomy for SFCC. There is not much research on this surgical treatment, and performing segmental left colectomy is still debatable. Most papers about SFCC involve a small number of subjects, and almost of them are retrospectively designed studies [10111213]. This is because SFCC is rarely detected as compared to other colon cancers, and this makes it hard to perform randomized controlled trials [1].
The present study is also conducted retrospectively, although we attempted to eliminate bias by adjustments with PSM. We used the PSM method to minimize selection bias and to enhance statistical accuracy by supplementing huge population differences between the control and experimental groups [9].
Recently, many studies on tumor sidedness have been actively conducted, and in all studies, the right and left colon are divided based on the distal third of the transverse colon [678]. The reason for this criterion is that tumor molecular and biological differences according to tumor sidedness are secondary to different embryological origins [14]. This study was conducted on the premise that the embryological origin of SFCC and sigmoid colon cancer is the same as the hindgut, so the molecular and biological characteristics are also the same.
Published studies on SFCC have noted that it has a poor prognosis as compared to other colon cancers. In our study, the LR group showed a higher proportion of stent insertion and poor pathologic histology before PSM, as did other papers about SFCC [31115]. However, pathologic tumor characteristics, such as pathologic stage, microinvasion, and tumor differentiation were similar in both groups after PSM. Furthermore, the LR group showed a similar 5-year long-term survival rate (DFS, OS) as compared to the AR group. The number of harvested lymph nodes in the LR group was 20, with sufficient lymph node dissection, and this was not inferior to the AR group. This is also related to the local recurrence rate, which presented no statistical difference in either group. In addition, the LR group presented longer proximal and distal resection margins than did the AR group after PSM.
To conclude, the results of this study demonstrate that LR is an oncologically safe procedure that enables the operator to perform sufficient lymph node dissection.
In terms of short-term surgical outcomes, these results were comparable between both groups except in the case of ileus. Although LR group procedures took longer than did the AR group procedures, there was no significant difference between other short-term postoperative outcomes such as bleeding, intraoperative complication rate, conversion rate, hospital days, days to diet, and surgical site infection. These results demonstrated that laparoscopic segmental left colectomy is a technically feasible procedure as compared to laparoscopic AR.
The LR group showed higher morbidity than did the AR group. However, most of the morbidity was caused by minor morbidity, specifically ileus. The ileus showed a significant difference; the LR group had a higher rate than did the AR group. This might be because of increased pressure around duodenojejunal flexure, which is the result of anastomosis in the segmental left colectomy procedure. Further research is needed on this. Except for this minor morbidity, surgical mortality rate was similar in both groups.
The present study is a multicenter study that was conducted at 2 institutions, and as a result, a larger population of subjects was recruited. This follow-up study was conducted over a comparatively long period, and we could analyze 5-year survival of the 2 procedures. What makes this study arguably more discriminative than others is that this is the first one to investigate the segmental left colectomy surgical method and to compare it with laparoscopic AR. Most former studies compared surgical approaches for SFCC between segmental left colectomy, extended right or left colectomy, and left hemicolectomy. They concluded that the outcomes of segmental left colectomy were not inferior to extended colectomy [13101316]. This study is more meaningful in the sense that it proved laparoscopic segmental left colectomy is an oncologically safe and technically feasible procedure as compared to laparoscopic AR, which is the most commonly used method.
Our study has limitations in the sense that it was retrospective research. Still, it collected many more subjects than did the other studies on SFCC, and it utilized PSM methods to overcome statistical bias. Considering the various strong points included in the study, we hope that it suggested a new perspective on surgical treatment of SFCC.
Except in cases of ileus, PSM showed that laparoscopic segmental left colectomy for SFCC did not show a statistical difference in short-term and long-term outcomes when compared to laparoscopic AR for sigmoid colon cancer. Laparoscopic segmental left colectomy can be one option among the standard procedures for SFCC.
References
1. de'Angelis N, Martínez-Pérez A, Winter DC, Landi F, Vitali GC, Le Roy B, et al. Extended right colectomy, left colectomy, or segmental left colectomy for splenic f lexure carcinomas: a European multicenter propensity score matching analysis. Surg Endosc. 2021; 35:661–672. PMID: 32072288.
2. Nakagoe T, Sawa T, Tsuji T, Jibiki M, Nanashima A, Yamaguchi H, et al. Carcinoma of the splenic f lexure: multivariate analysis of predictive factors for clinicopathological characteristics and outcome after surgery. J Gastroenterol. 2000; 35:528–535. PMID: 10905361.
3. Rega D, Pace U, Scala D, Chiodini P, Granata V, Fares Bucci A, et al. Treatment of splenic f lexure colon cancer: a comparison of three different surgical procedures: experience of a high volume cancer center. Sci Rep. 2019; 9:10953. PMID: 31358904.

4. Kim CW, Shin US, Yu CS, Kim JC. Clinicopathologic characteristics, surgical treatment and outcomes for splenic flexure colon cancer. Cancer Res Treat. 2010; 42:69–76. PMID: 20622960.

5. Lee SY, Yeom SS, Kim CH, Kim YJ, Kim HR. Distribution of lymph node metastasis and the extent of lymph node dissection in descending colon cancer patients. ANZ J Surg. 2019; 89:E373–E378. PMID: 31452333.

6. Imperial R, Ahmed Z, Toor OM, Erdoğan C, Khaliq A, Case P, et al. Comparative proteogenomic analysis of right-sided colon cancer, left-sided colon cancer and rectal cancer reveals distinct mutational profiles. Mol Cancer. 2018; 17:177. PMID: 30577807.

7. Yahagi M, Okabayashi K, Hasegawa H, Tsuruta M, Kitagawa Y. The worse prognosis of right-sided compared with left-sided colon cancers: a systematic review and meta-analysis. J Gastrointest Surg. 2016; 20:648–655. PMID: 26573851.

8. Loupakis F, Yang D, Yau L, Feng S, Cremolini C, Zhang W, et al. Primary tumor location as a prognostic factor in metastatic colorectal cancer. J Natl Cancer Inst. 2015; 107:dju427. PMID: 25713148.

9. Austin PC. Optimal caliper widths for propensity-score matching when est imat ing di f ferences in means and differences in proportions in observational studies. Pharm Stat. 2011; 10:150–161. PMID: 20925139.
10. de'Angelis N, Hain E, Disabato M, Cordun C, Carra MC, Azoulay D, et al. Laparoscopic extended right colectomy versus laparoscopic left colectomy for carcinoma of the splenic flexure: a matched case-control study. Int J Colorectal Dis. 2016; 31:623–630. PMID: 26689401.
11. Chenevas-Paule Q, Trilling B, Sage PY, Girard E, Faucheron JL. Laparoscopic segmental left colectomy for splenic flexure carcinoma: a single institution experience. Tech Coloproctol. 2020; 24:41–48. PMID: 31834555.

12. Pisani Ceretti A, Maroni N, Sacchi M, Bona S, Angiolini MR, Bianchi P, et al. Laparoscopic colonic resection for splenic flexure cancer: our experience. BMC Gastroenterol. 2015; 15:76. PMID: 26148781.

13. Rouffet F, Hay JM, Vacher B, Fingerhut A, Elhadad A, Flamant Y, et al. Curative resection for left colonic carcinoma: hemicolectomy vs. segmental colectomy: a prospective, controlled, multicenter trial. French Association for Surgical Research. Dis Colon Rectum. 1994; 37:651–659. PMID: 8026230.
14. Dekker E, Tanis PJ, Vleugels JL, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019; 394:1467–1480. PMID: 31631858.

15. Manceau G, Mori A, Bardier A, Augustin J, Breton S, Vaillant JC, et al. Lymph node metastases in splenic flexure colon cancer: is subtotal colectomy warranted? J Surg Oncol. 2018; 118:1027–1033. PMID: 30212600.

16. Bademci R, Bollo J, Martinez Sanchez C, Hernadez P, Targarona EM. Is segmental colon resection an alternative treatment for splenic flexure cancer? J Laparoendosc Adv Surg Tech A. 2019; 29:621–626. PMID: 30950767.

Fig. 1
Laparoscopic segmental left colectomy procedure. (A) Ligation of left colic artery. (B) Ligation of middle colic artery left branch. (C) Laparoscopic segmental left colectomy specimen.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download