Abstract
Purpose
Coronavirus disease 2019 (COVID-19) affects healthcare systems worldwide; however, few studies have assessed the impact of COVID-19 on emergent surgical diseases. This study aimed to investigate the impact of COVID-19 on the care given to patients with acute appendicitis in Korea.
Methods
Between November 2019 and November 2020, 495 patients underwent laparoscopic surgery for acute appendicitis. The patients were divided into prepandemic and pandemic groups. The baseline characteristics and perioperative outcomes were compared.
Results
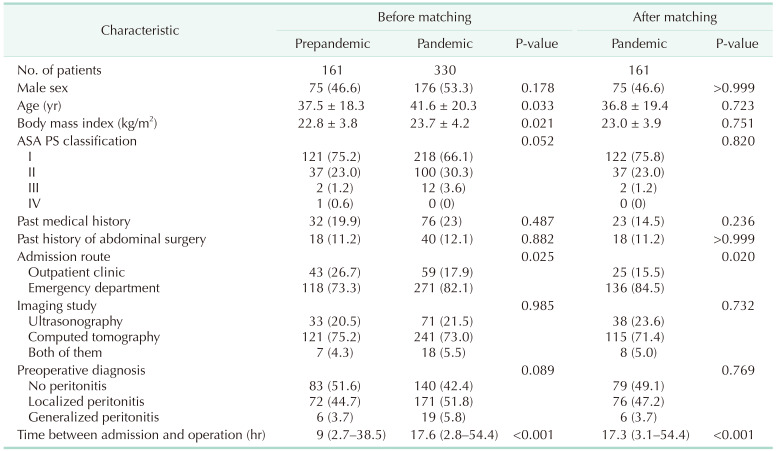
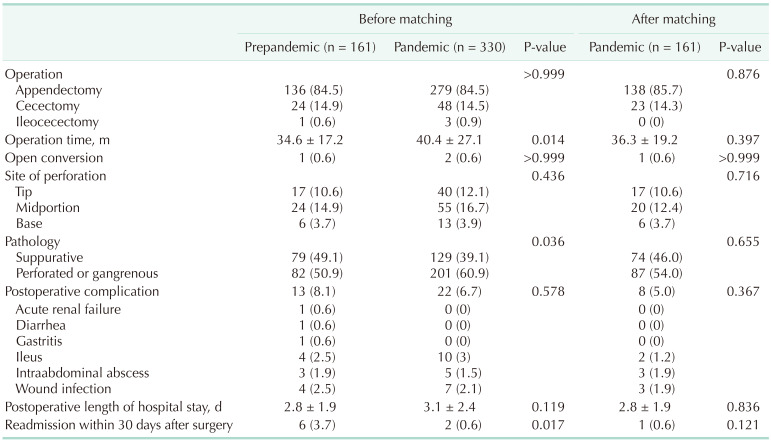
The time between admission and surgery was longer in the pandemic group than in the prepandemic group (17.6 hours vs. 9 hours, P < 0.001). The operation time was longer (5.8 minutes, P = 0.014), inflammation was more severe (10%, P = 0.036), and more patients visited the emergency room (82.1% vs. 73.3%, P = 0.025) in the pandemic group than in the prepandemic group. There were no significant differences in postoperative complications or length of hospital stay between the 2 groups. After propensity score matching, the time to surgery was delayed (17.3 hours vs. 9 hours, P < 0.001) and more patients visited the emergency room (84.5% vs. 73.3%, P = 0.020) in the pandemic group.
Coronavirus disease 2019 (COVID-19) has affected the healthcare systems of most countries worldwide and has changed the nature of medical services. Various perspectives have been suggested for the surgical field since the World Health Organization (WHO) declared a COVID-19 pandemic on March 11, 2020 [1]. It is clear that patients with COVID-19 have poor postoperative outcomes. Indeed, a large international cohort study including 235 hospitals in 24 countries reported that postoperative pulmonary complications and high mortality occurred in over half of the patients with perioperative COVID-19 infection [2]. Another matched study also showed higher rates of surgical mortality and complications in patients with COVID-19 than in those without [3]. Based on these results, the WHO has suggested that non-urgent procedures should be considered for postponement.
Concurrently, some experts have focused on the safety and protection of healthcare workers who work in surgery. Most of these experts suggested that decisions to proceed with scheduled surgeries should not only consider the clinical situation but also the availability of personal protective equipment for healthcare workers [4]. Another researcher warned of the risks of viral contamination in healthcare workers during laparoscopic surgery, which may produce potentially harmful aerosols from pneumoperitoneum [5]. However, inevitable and emergent clinical situations that generally involve laparoscopic surgery, such as acute appendicitis, still exist and remains unknown how surgeons should manage such situations in the era of COVID-19.
Laparoscopic surgery for acute appendicitis is the sixth most common surgical practice among all surgeries and the first general surgical emergency in Korea, with 74,823 cases in 2019 [6]. Although a few reports have suggested conservative management for acute appendicitis according to strict criteria, antibiotic therapy for adult appendicitis is not always successful, and a significant proportion of patients still require surgery at some point [78]. Several reports have assessed changes in the management of acute appendicitis in the era of COVID-19. These reports found that there was a long delay between the onset of symptoms and medical consultation and between admission and surgery, an increased rate of complicated appendicitis and surgical management, poorer clinical features of patients, longer operation times (OTs), and more postoperative pain compared to those before the pandemic [910111213]. However, the previous studies reflected the situation and healthcare systems of countries that are considerably different from those of Korea, and to date, there has been no report from Korea. Therefore, in this study, we aimed to investigate the impact of COVID-19 on acute appendicitis in Korea.
We reviewed the medical records of patients diagnosed with acute appendicitis based on clinical manifestations, laboratory studies, and imaging studies at Kyung Hee University Hospital at Gangdong, Seoul, Korea, between November 2019 and November 2020. The Institutional Review Board of our hospital approved the study (No. 2021–03-012), and all consecutive patients were included. This study was performed in accordance with the Declaration of Helsinki. Written informed consent was waived due to its retrospective nature. Patients who underwent delayed surgery after conservative management or percutaneous drainage of intraabdominal abscesses were excluded because the time delay between admission and surgery, which is an important variable, would be too long to be analyzed. Moreover, the decision for delayed surgery was made according to the surgeons-on-duty and was not based on a solid principle in our institution. However, considering the sick leave that must be taken by patients due to appendicitis, laparoscopic appendectomy is a better option in Korea than antibiotic therapy alone.
The following patient demographic data were assessed: sex, age, body mass index (BMI), American Society of Anesthesiologists (ASA) physical status (PS) classification, past medical history, previous abdominal surgery, admission route (outpatient clinic or emergency room), imaging study for diagnosis, preoperative diagnosis of peritonitis, and time between admission and surgery.
The following perioperative data were also collected: operation type, OT, site of perforation intraoperatively (tip, midportion, and base), inflammation severity according to pathologic reports (suppurative vs. perforated or gangrenous), conversion to open surgery, postoperative complications, postoperative length of stay (LOS), and readmission within 30 days after surgery. Ten surgeons performed laparoscopic surgery for acute appendicitis during the study period. The surgical technique has been described in detail in our previous study [14].
In Korea, patients with COVID-19 were exclusively cared for by a designated care center and were not included in this study. However, to ensure the safety of the medical staff in the operating theater, each hospital established a preoperative screening strategy before surgery. All patients who required admission received a COVID-19 test first, and the admission process could proceed only if the result was confirmed as negative. When a patient showed a positive result for COVID-19, the patient was transferred to one of the hospitals designated for the treatment of COVID-19 by the Korean government. Polymerase chain reaction (PCR) tests for COVID-19 were performed at our institution during the study period. The antigen test, which took less than 2 hours, was not available. The PCR test, which requires several hours, was performed for all patients diagnosed with acute appendicitis, irrespective of whether they were admitted to an emergency room or an outpatient department. The results of the PCR tests for COVID-19 were listed 3 times each working day (11:30, 16:30, and 20:00) and twice a day on weekends (11:30 and 16:30). The negative COVID-19 results of all patients who needed surgery had to be confirmed before entering the surgery theater. If a patient had close contact with infected people before surgery but showed a negative result, the surgery was rescheduled to the last order of the day, and healthcare workers who participated in the surgery had to use protective equipment to reduce the possibility of infection. All of these policies regarding COVID-19 were in effect from March 2020, and we divided the patient groups for analysis based on that time.
Continuous variables were analyzed using the Student t-test, whereas categorical variables were analyzed using the chi-square test. Statistical significance was set at P < 0.05. After assessing differences and tendencies by comparing the groups before and after the pandemic, propensity score matching was performed to evaluate whether delayed surgery itself affected perioperative outcomes after balancing baseline characteristics. Matching was estimated based on sex, age, BMI, and ASA PS classification using a logistic regression model and matched at a 1:1 ratio. All statistical analyses were performed using the IBM SPSS Statistics ver. 20.0 (IBM Corp., Armonk, NY, USA).
A total of 495 patients underwent laparoscopic surgery for acute appendicitis. Overall, appendectomies did not decrease compared to 1 year before the study period (474 patients between November 2018 and October 2019). All cases were confirmed by imaging studies such as ultrasonography, CT, or both, and there was no significant difference between the pre- and pandemic groups. If ultrasonography failed to diagnose appendicitis for any reason (e.g., intestinal gas, appendix location, or obesity), a CT scan was subsequently performed. Four patients who underwent delayed surgery after conservative management or percutaneous drainage of intraabdominal abscess were excluded (3 in the prepandemic group and 1 in the pandemic group). None of the patients in the prepandemic group received the PCR test for COVID-19 (n = 161), and all patients in the pandemic group received the test (n = 330). None of the 330 patients had positive COVID-19 results.
The baseline characteristics of the 2 groups were slightly different (Table 1). The mean age and BMI in the pandemic group were higher than those in the prepandemic group (4.1 years, P = 0.033 and 0.9 kg/m2, P = 0.021, respectively). The pandemic group tended to have a lower ASA PS classification, with a borderline P-value (P = 0.052). More patients were admitted from an emergency room than from an outpatient clinic in the pandemic group than in the prepandemic group (73.3% vs. 82.1%, P = 0.025). The proportion of peritonitis based on preoperative imaging studies seemed to be higher in the pandemic group, but the difference was not significant (P = 0.089). The time between admission and surgery increased more in the pandemic group than in the prepandemic group (17.6 hours vs. 9 hours, P < 0.001). Although the operation type was not significantly different between the 2 groups, the OT was longer in the pandemic group than in the prepandemic group (P = 0.014, Table 2). Pathologic reports revealed that inflammation was more severe in the pandemic group than in the prepandemic group (50.9% vs. 60.9%, P = 0.036). There were no significant differences in postoperative complications and LOS. All resected specimens underwent pathologic assessment, and there were no negative appendectomies.
After propensity score matching to adjust for the imbalance in baseline characteristics between the 2 groups, all variables were well-balanced except for the admission route (through an emergency room rather than an outpatient clinic, 84.5% vs. 73.3%; P = 0.020) and the time between admission and surgery (17.3 hours vs. 9 hours, P < 0.001) (Table 1). The perioperative outcomes, including OT, postoperative complications, and LOS, were similar between the 2 groups (Table 2). Severe inflammation on pathology, which was noted before matching, did not differ significantly between the groups.
In the COVID-19 era, several variables of patients with acute appendicitis worsened compared to those in the prepandemic era. The time to surgery was almost twice as long (9 hours vs. 17.6 hours) because preoperative COVID-19 tests were required. Although more patients were admitted through emergency rooms than outpatient clinics, and the OT increased, there was no significant difference in the postoperative clinical course. However, after balancing potentially confounding variables, we found no significant difference in postoperative outcomes despite a delay in the time to surgery (8.3 hours). Therefore, whether the delay itself affects the severity of appendicitis or the perioperative outcomes remains unclear.
Most studies on acute appendicitis have reported increased severity and worsened postoperative outcomes. A report from Germany showed that appendectomies decreased by 13.5%, and the severity of appendicitis increased in the first 2020 COVID-19 lockdown compared to 2019 [13]. The authors explained that patients’ fear of an in-hospital COVID-19 infection might result in a delay to contact a surgeon, and subsequently, the inflammation would progress or a self-limiting course might occur. Another possible reason is the scarcity of resources and prioritization. Other investigators in the UK reported a similar phenomenon, with higher inflammatory markers and more severe disease of the appendix during the pandemic than before [10]. Fisher et al. [15] warned that disruption to local healthcare delivery systems might negatively impact surgical disease, and reported higher rates of perforated appendicitis in children from New York. Another study from the United States showed an increased rate of perforated appendicitis, LOS, OT, and complications [12]. In our study, age, BMI, greater use of an emergency room, and inflammation severity were also found to be higher in the pandemic group than in the prepandemic group, similar to other countries; however, no significant difference was found in the number of patients and perioperative outcomes between the groups, except for OT.
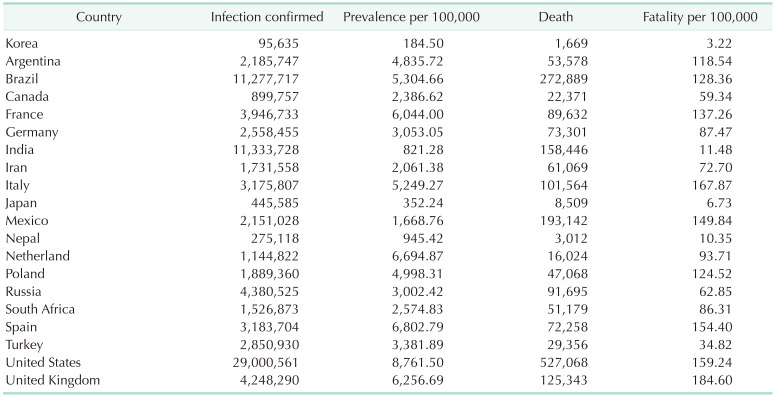
The Korean healthcare system is well-known among the countries of Organisation for Economic Co-operation and Development (OECD) for providing medical services with high quality and low cost [16]. Accessibility to medical services is fundamentally good, with 17 doctor consultations per person per year, whereas the OECD average was 6.8 in 2017. There are sufficient healthcare workers, and an extremely cost-effective healthcare system has been established in Korea. However, older age, higher BMI, higher ASA PS classification, greater use of the emergency room, and more severe inflammation in the pandemic group suggest that patients tended to endure symptoms and visited the hospital late, even under the well-established healthcare system. Moreover, identification of the patients’ medical use before and after the pandemic using large population-based data would be helpful to clarify the blind points. In addition, the prevalence of COVID-19 was insufficient to affect established healthcare systems. Only 95,635 patients were infected with COVID-19 and 1,669 died in Korea up to March 14, 2021 (prevalence per 100,000 = 184.5, fatalities per 100,000 = 3.22), whereas other countries showed much worse results (Table 3) [17]. Finally, the 3T strategy (testing-tracing-treatment), established by the government, was effective in allowing hospitals to maintain their work without delaying scheduled procedures [18]. Therefore, we did not need to investigate the time delay between symptom onset and medical consultation.
Some authors have reported that the rate of diagnosis by CT scan increased (38.1% to 64.5%), which subsequently resulted in a shorter time to the theater (24 hours to <24 hours) during the pandemic [10]. These previous studies revealed that prepandemic diagnoses of appendicitis relied heavily on clinical examination, with an overall negative appendectomy (i.e., no evidence of appendicitis by histopathology postoperatively) rate of 10%, but the negative appendectomy rate decreased in the pandemic. In contrast, none of the patients underwent negative appendectomy in our study because all patients underwent CT and/or ultrasonography imaging studies in addition to clinical and laboratory examinations. Moreover, the time to theater lengthened, although the lengthened results were even shorter than those of other countries.
Conservative management of appendicitis, rather than surgery, has increased during the pandemic [1011]. The results might be based on the scarcity of resources and prioritization; however, although some authors have suggested that conservative management is comparable to appendectomy, we believe that surgery is the gold standard for treating acute appendicitis. A report showed that 29% of the patients who received antibiotics eventually underwent appendectomy, although the report concluded that antibiotics were not inferior to appendectomy [7]. Moreover, complications were more common in the group treated with antibiotics than in those who underwent appendectomy. Because all diagnostic modalities can be easily used in Korea, a diagnosis is usually confirmed, and the decision to perform surgery is not as difficult as it is in countries following different national policies.
After assessing the tendency of the group of patients and the impact of pandemic on the perioperative outcomes, we attempted to establish a clinically meaningful influence of delayed time to surgery using propensity score matching; however, we found no significant difference, except for the admission route and delay in surgery. As mentioned above, more visits to emergency rooms might reflect variations in patients’ medical use during the pandemic. However, based on our results, more emergency room visits and an 8.6-hour delay did not cause problems for patients with both non-complicated and complicated appendicitis.
This study has some limitations that must be noted. First, the retrospective nature of the study may have resulted in a selection bias. Second, the authors could only investigate the impact of COVID-19 tests on perioperative outcomes of acute appendicitis, and not the impact of COVID-19 infection itself. The data of COVID-19 patients with acute appendicitis may be obtained from designated hospitals to treat COVID-19. Third, the results of this study cannot be applied to other populations because the healthcare system and situations encountering COVID-19 vary from country to country. Fourth, some authors suggested that complicated appendicitis was associated with a delay in surgery from symptom onset rather than a delay in-hospital arrival [19]. However, data on the time from symptom onset to hospitalization could not be assessed because it was both unclear and unreliable in this retrospective study.
In conclusion, pat ients in Korea who underwent appendectomy for appendicitis during the COVID-19 pandemic tended to have a few factors that were worse than those in prepandemic patients. Although the time from admission to theater was delayed due to the need for COVID-19 tests and the severity of appendicitis increased, there was no definite deterioration in postoperative outcomes, including postoperative complications or LOS. A lthough acute appendicitis is an emergent condition, preoperative COVID-19 tests should be performed to ensure the safety of both the patients and the healthcare workers involved in the surgery.
ACKNOWLEDGEMENTS
This work was presented at the 54th annual congress of the Korean Society of Coloproctology, April 2–4, 2021, Seoul, Korea.
Notes
References
1. World Health Organization (WHO). WHO announces COVID-19 outbreak a pandemic [Internet]. Geneva: WHO;2020. cited 2021 Mar 15. Available from: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic.
2. COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020; 396:27–38. PMID: 32479829.
3. Doglietto F, Vezzoli M, Gheza F, Lussardi GL, Domenicucci M, Vecchiarelli L, et al. Factors associated with surgical mortality and complications among patients with and without coronavirus disease 2019 (COVID-19) in Italy. JAMA Surg. 2020; 155:691–702. PMID: 32530453.

4. Morris M, Pierce A, Carlisle B, Vining B, Dobyns J. Pre-operative COVID-19 testing and decolonization. Am J Surg. 2020; 220:558–560. PMID: 32466826.

5. Veziant J, Bourdel N, Slim K. Risks of viral contamination in healthcare professionals during laparoscopy in the Covid-19 pandemic. J Visc Surg. 2020; 157:S59–S62. PMID: 32340900.

6. National Health Insurance Service (NHIS). Main surgery statistical yearbook for 2019 [Internet]. Wonju: NHIS;2019. cited 2021 Mar 15. Available from: https://www.nhis.or.kr/nhis/together/wbhaec06800m01.do?mode=view&articleNo=10803657&article.offset=0&articleLimit=10.
7. CODA Collaborative, Flum DR, Davidson GH, Monsell SE, Shapiro NI, Odom SR, et al. A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med. 2020; 383:1907–1919. PMID: 33017106.

8. Javanmard-Emamghissi H, Boyd-Carson H, Hollyman M, Doleman B, Adiamah A, Lund JN, et al. The management of adult appendicitis during the COVID-19 pandemic: an interim analysis of a UK cohort study. Tech Coloproctol. 2021; 25:401–411. PMID: 32671661.

9. Orthopoulos G, Santone E, Izzo F, Tirabassi M, Pérez-Caraballo AM, Corriveau N, et al. Increasing incidence of complicated appendicitis during COVID-19 pandemic. Am J Surg. 2021; 221:1056–1060. PMID: 33012500.

10. Bajomo O, Hampal R, Sykes P, Miah A. Managing appendicitis during the COVID-19 era: a single centre experience& implications for future practice. Ann Med Surg (Lond). 2021; 63:102168. PMID: 33614025.
11. Baral S, Chhetri RK, Thapa N. Comparison of acute appendicitis before and within lockdown period in COVID-19 era: a retrospective study from rural Nepal. PLoS One. 2021; 16:e0245137. PMID: 33406126.

12. Finkelstein P, Picado O, Muddasani K, Wodnicki H, Mesko T, Unger S, et al. A retrospective analysis of the trends in acute appendicitis during the COVID-19 pandemic. J Laparoendosc Adv Surg Tech A. 2021; 31:243–246. PMID: 33181062.

13. Willms AG, Oldhafer KJ, Conze S, Thasler WE, von Schassen C, Hauer T, et al. Appendicitis during the COVID-19 lockdown: results of a multicenter analysis in Germany. Langenbecks Arch Surg. 2021; 406:367–375. PMID: 33550453.

14. Kim CW, Jeon SY, Paik B, Bong JW, Kim SH, Lee SH. Resident learning curve for laparoscopic appendectomy according to seniority. Ann Coloproctol. 2020; 36:163–171. PMID: 32054238.

15. Fisher JC, Tomita SS, Ginsburg HB, Gordon A, Walker D, Kuenzler KA. Increase in pediatric perforated appendicitis in the New York City Metropolitan region at the epicenter of the COVID-19 outbreak. Ann Surg. 2021; 273:410–415. PMID: 32976285.

16. Organisation for Economic Co-operation and Development (OECD). Health at a glance 2019: OECD indicators. Paris: OECD Publishing;2019.
17. Central Disease Control Headquarters. Coronavirus disease-19, Republic of Korea: global locations with COVID-19 [Internet]. Sejong, KR: Ministry of Health and Welfare;2021. cited 2021 Mar 14. Available from: http://ncov.mohw.go.kr.
18. Park Y, Huh IS, Lee J, Kang CR, Cho SI, Ham HJ, et al. Application of testing-tracing-treatment strategy in response to the COVID-19 outbreak in Seoul, Korea. J Korean Med Sci. 2020; 35:e396. PMID: 33230987.

19. Kim M, Kim SJ, Cho HJ. Effect of surgical timing and outcomes for appendicitis severity. Ann Surg Treat Res. 2016; 91:85–89. PMID: 27478814.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download