INTRODUCTION
Hirschsprung disease (HD) is a distinctive congenital disease. The absence of ganglion cells in the distal intestine leads to distal bowel obstruction and defecation disorders, which can trigger colitis and sepsis [
1]. HD is a rare disease, with a reported incidence of 1:5,000, requiring proper and meticulous surgical treatment for the maintenance of normal bowel habits.
Traditional pull-through procedures have shown favorable outcomes. Transanal single-stage endorectal pull-through (TERPT) procedure was introduced for short-segment HD in 1998 by De la Torre-Mondragón et al. [
2]. Several studies have revealed that TERPT procedure has favorable short- and mid-term results, with lower complication rates. However, in some patients, various degrees of bowel dysfunction and defects in fecal continence persist for a long time [
34]. Regarding long-term outcomes after finishing bowel training, some debates have remained, and few studies have investigated a large number of patients who are suitable for meta-analysis in relation to long-term results after bowel training [
3].
In this study, we attempted to reveal the mid- and long-term functional outcomes of TERPT procedure performed during the infantile period for patients who completed toilet training using the Bowel Function Score (BFS) [
5].
Go to :

METHODS
We investigated 160 patients who underwent definite corrective operations after the pathological diagnosis of HD at a single center between 2001 and 2013. Among them, 106 cases of TERPT procedure were performed, and 103 were performed during the patient's infantile period. All TERPT procedures were performed by a single surgeon. All patients who underwent TERPT procedure had short-segment diseases that confined the rectosigmoid colon, and cases with endorectal pull-through with laparotomy or laparoscopy were excluded. For HD evaluation, colon study and rectal manometry were performed preoperatively. Preoperative biopsy was not conducted in all cases. Rectal full-thickness biopsy with frozen examination for the presence of ganglion cells under general anesthesia was performed just before TERPT procedure. After confirming the HD by frozen section, the mucosal incision was made 0.5 cm above the dentate line. Submucosal dissection was conducted until peritoneal reflection with a long muscular cuff, and posterior myomectomy was performed approximately 3–4 mm in width. After peritoneal reflection, full layers of the colon were dissected. When the frozen section was positive for the presence of ganglion cells twice in a row, dissection of the colon was stopped and the colon was anastomosed just above the dentate line.
Eighty-two patients followed up until 42 months of age were enrolled, and 21 were excluded due to follow-up loss or a short follow-up period. In our institution, follow-up schedules at the outpatient clinic depended on the patient's condition until approximately 2 years, when their bowel functions become stable. After that, unless any problems occurred, patients visited the outpatient clinic every 6 months. When patients were 7–8 years old and had favorable bowel function, regular follow-ups at the outpatient clinic were discontinued.
During follow-up, unavoidable dysfunctions, such as severe constipation or acute colonic distension due to spasm, were also managed. If the patient could not defecate for more than 3 days or when the patient experienced severe difficulty in defecating, laxatives such as lactulose were administered orally. If it was not effective, glycerin enemas were performed once a day or every 2 days at home, until difficulties in defecating were improved. If there was acute colonic distension due to spasm, a rectal tube was inserted, and irrigation with warm saline was performed. When the colonic distension and spasm were relieved, the tube was removed and the patient was observed in the outpatient clinic.
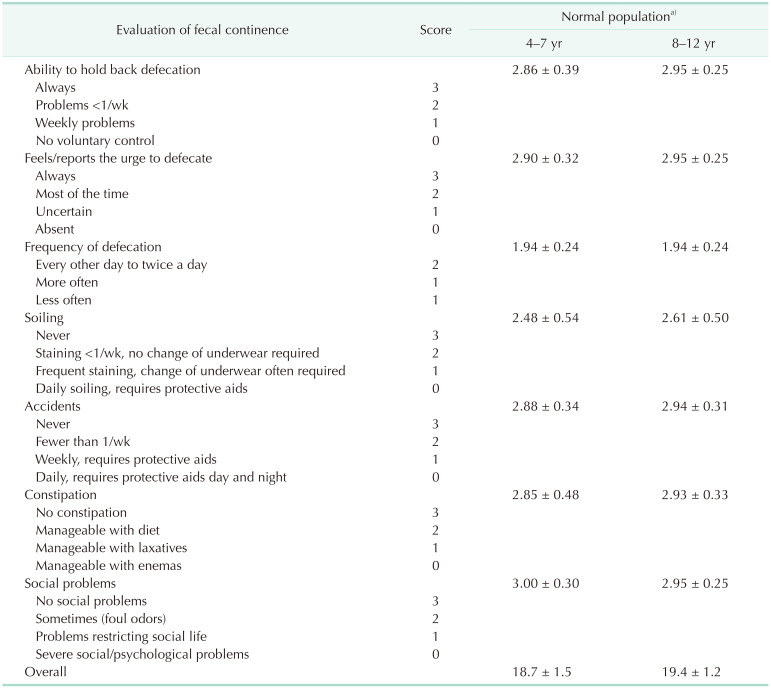
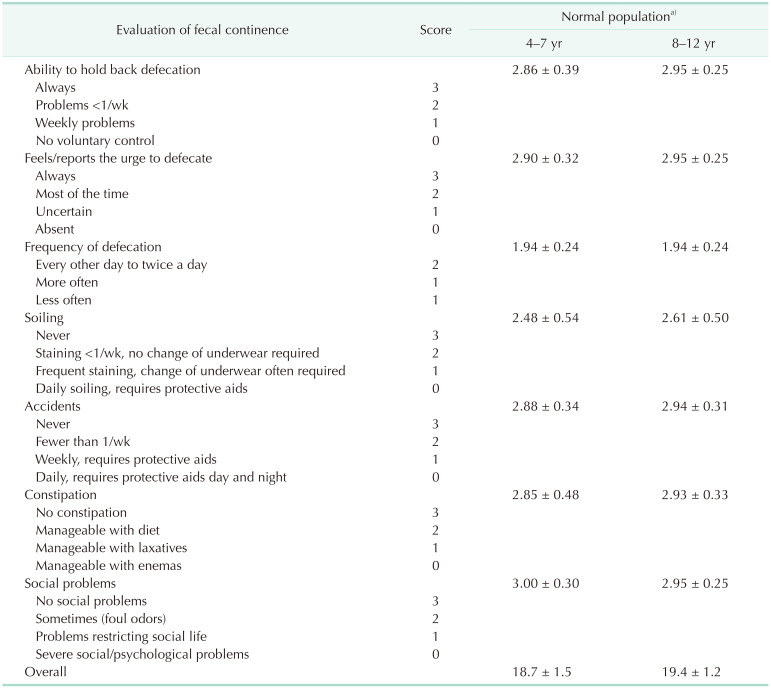
Functional outcomes were investigated according to the BFS (
Table 1) [
56] at the outpatient clinic, when each regular follow-up day from 42 months until the end of follow-up, by a single investigator who had performed the operation, The BFS questionnaire consists of 7 items and was developed to evaluate the functional outcomes of surgery for anorectal malformations and other colonic disorders. The BFS was then validated. BFS of ≥17 for 4–7 years of age (mean, 18.9 years) and BFS of ≥18 for 8–12 years of age (mean, 19.2 years) were archived by ≥90% of the normal population [
5].
Table 1
Bowel Function Score (BFS) and BFS of normal population

The clinicopathologic data, operative findings, operative methods, and outcomes, including BFS, were investigated using a retrospective medical record review. Statistical analysis was performed using IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA). BFS was analyzed using a one-sample t-test. Statistical significance was set at P < 0.05. The one-sample t-test examines whether the mean of a population is statistically different from a known or hypothesized value. In a one-sample t-test, the test variable's mean is compared against a “test value,” which is a known or hypothesized value of the mean in the population. In this study, the values obtained through the questionnaire were compared with the normal values reported in previous studies.
This study was approved by the Institutional Review Board of Pusan National University Yangsan Hospital (No. 05–2020–020). The requirement for informed consent was waived because of the retrospective nature of the study.
Go to :

RESULTS
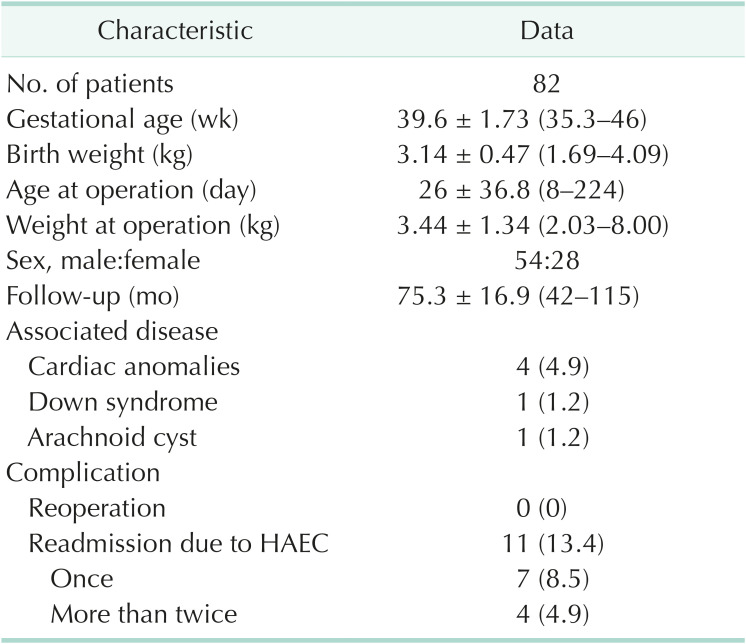
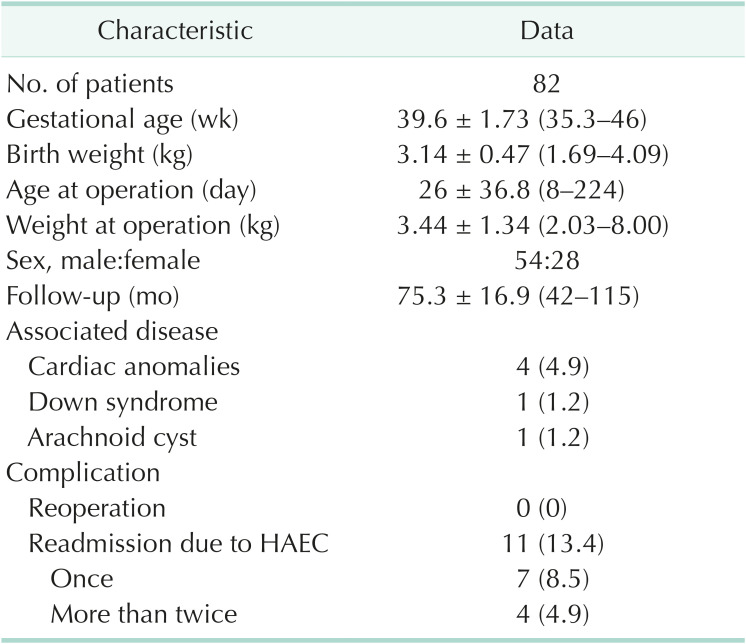
Patient characteristics
Fifty-four male and 28 female children were included in the study. The mean age and weight at operation were 26 ± 36.8 days (range, 8–224 days) and 3.44 ± 1.34 kg (range, 2.03–8.00 kg), respectively. The mean follow-up period was 75.3 ± 16.9 months (range, 42–115 months). Six patients had associated diseases: 4 patients had cardiac anomalies, including atrial septal defects, ventricular septal defects, and pulmonary stenosis; 1 patient had Down syndrome; and 1 patient had an arachnoid cyst (
Table 2).
Table 2
Characteristics of the study population

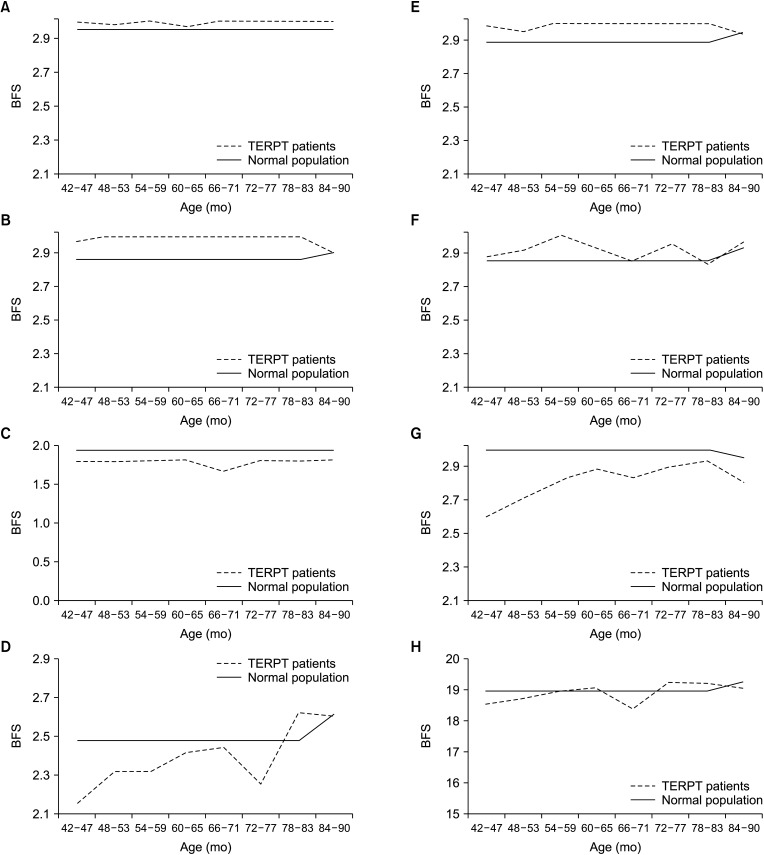
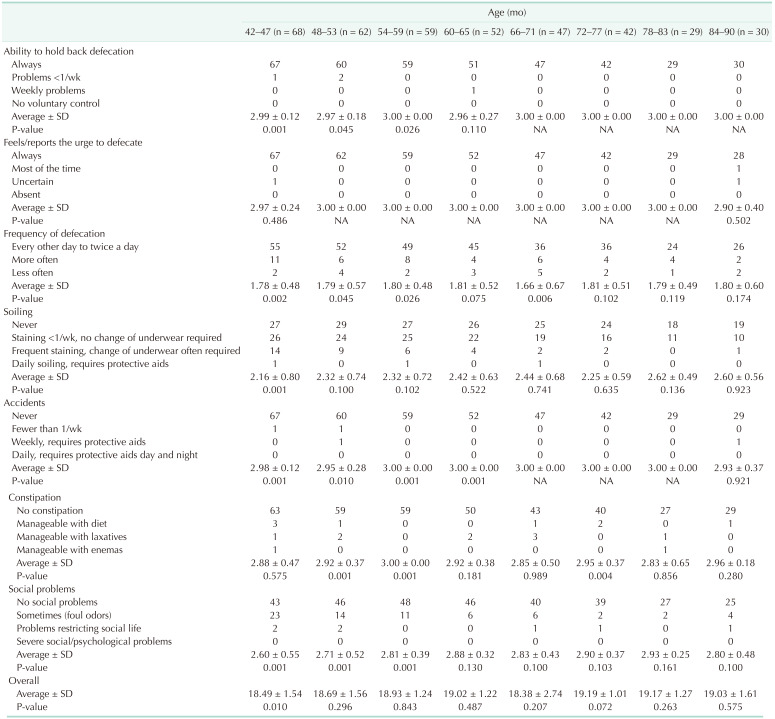
Ability to hold back defecation and recognition of the urge to defecate
The ability to hold back defecation was excellent during the entire investigation period. Only 4 patients had temporary problems. Recognition of the urge to defecate was also good. Apart from 1 patient in the 42-month-old group and 2 patients in the 84–90-month-old group, every patient answered that they felt the urge to defecate. Regarding those 2 questions, similar scores were obtained from the normal population (
Table 3,
Fig. 1).
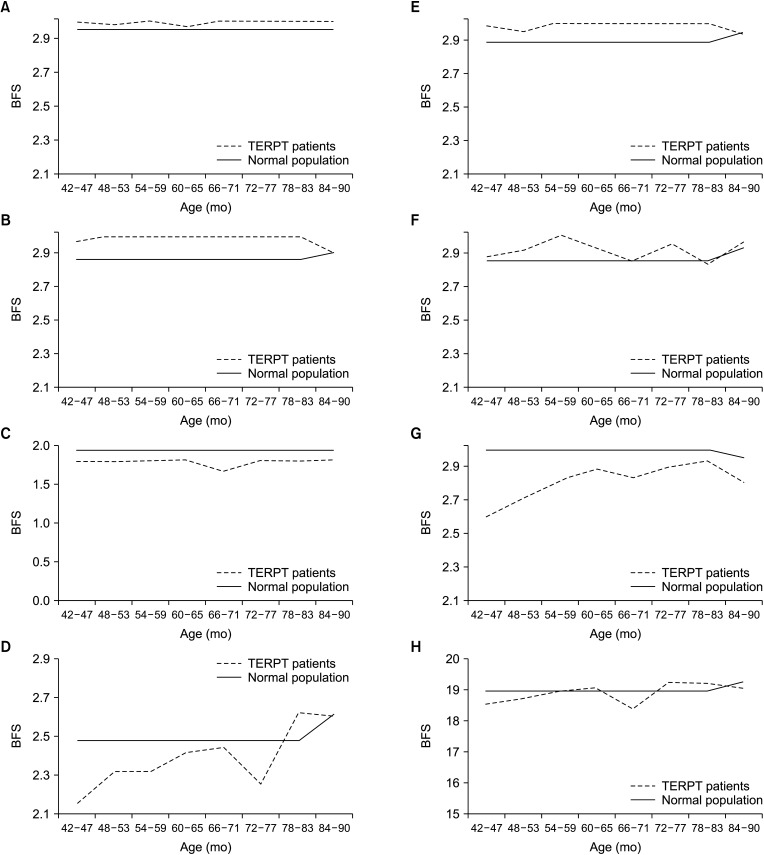 | Fig. 1Average Bowel Function Score (BFS) of the patients who underwent transanal single-stage endorectal pull-through (TERPT) procedure and the normal population. (A) Ability to hold back defecation, (B) feels/reports the urge to defecate, (C) frequency of defecation, (D) fecal soiling, (E) fecal accidents, (F) constipation, (G) social problems, and (H) overall.
|
Table 3
Bowel Function Score by age
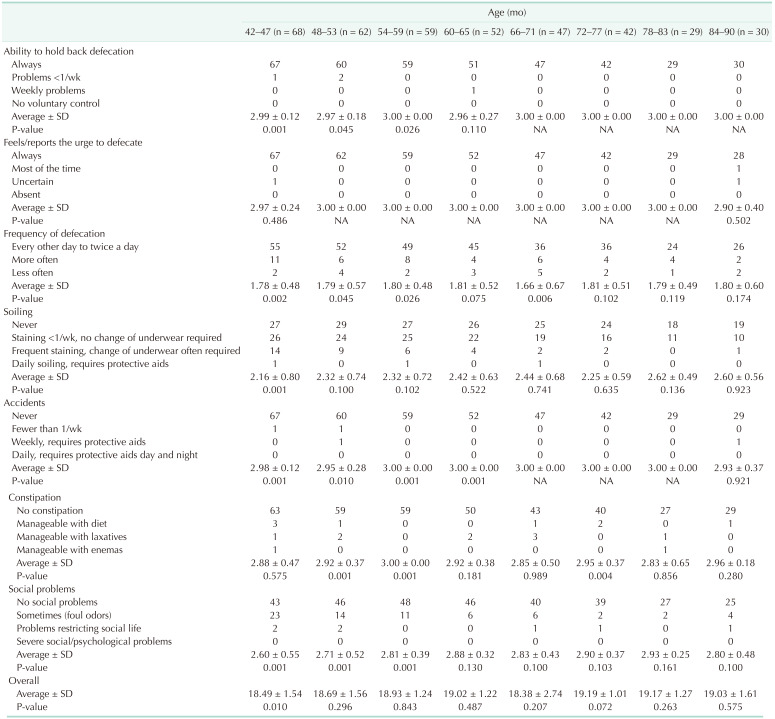

Stooling frequency
During the investigation period, TERPT patients seemed to have more frequent defecation. In patients younger than 7 years of age, the BFS of this session was significantly lower than that of the normal population. During that period, the rates of patients with more frequent defecation (more than 2 times a day) were higher than those in the normal population. In patients older than 72 months of age, the differences decreased and became statistically insignificant (
Table 3,
Fig. 1).
Fecal incontinence: soiling and fecal accidents
Only at 42–47 months of age, the scores of TERPT patients regarding fecal soiling were statistically lower than those of the normal population. The scores were continuously low until 7 years of age but were statistically insignificant. After 7 years of age, the scores were similar. Regarding fecal accidents, TERPT patients showed good outcomes, and only 4 patients experienced accidents (
Table 3,
Fig. 1).
Constipation
During the overall investigation period, most patients did not experience constipation. The rates of patients requiring laxatives or enemas were very low and not inferior to those of the normal population. However, some patients required regular laxatives and enemas (
Table 3,
Fig. 1). No patients required a rectal biopsy for presumed acquired aganglionosis after surgery for constipation.
Social problems and overall scores
The score for social problems was significantly low until 60 months of age. Most patients who had problems answered “Sometimes (foul odor).” This score also improved with age, and at 6–7 years of age, the scores were not statistically different from those of the normal population.
Overall scores improved with age and were not statistically different from those of the normal population (
Table 3,
Fig. 1).
Readmission due to Hirschsprung disease-associated enterocolitis
Eleven patients (13.4%) were admitted because of HD-associated enterocolitis. Three patients were admitted twice, and 1 patient was admitted 3 times. The mean age at admission was 4.0 ± 7.8 months (range, 2–26 months). The mean hospital stay for 1 admission was 3.0 ± 4.87 days (range, 1–18 days). The sum of hospital stay for each patient was 11.5 ± 7.34 days (range, 2–23 days). All patients recovered with conventional treatment, including hydration, intravenous antibiotics, and bowel irrigation.
Survival and reoperation
Two patients died and were not included in this study for the investigation of functional outcomes due to the short follow-up period.
One patient died 11 months after TERPT procedure at 13 months of age. A colon study was conducted to evaluate postoperative constipation. During the colon study, he had sudden onset cardiac arrest and died despite attempting resuscitation. He was dehydrated because of HD-associated enterocolitis when the colon study was performed. Gastrografin, which was used in the colon study, worsened dehydration and induced a fatal electrolyte imbalance and hypovolemic shock. The other patients underwent TERPT procedure performed at 15 days of age. Although the resected specimen was proven to have HD and all aganglionic segments were excised, the patient had severe feeding intolerance and no bowel movement. After 1 month, an exploratory laparotomy was performed to examine the bowel. The results of the biopsy of the colon and appendix were normal. He died the month after due to a multiorgan failure. He was the only patient who underwent reoperation.
Go to :

DISCUSSION
The operation for HD has been developed since it was described by Swenson in the late 1940s [
7]. Then, the Duhamel and Soave procedures were introduced as alternatives to avoid injury to neighboring structures during deep pelvic dissection for the Swenson procedure [
8]. These 3 operations are performed worldwide and show similar outcomes [
89]. However, all 3 classic operations require laparotomy with abdominal skin incisions in the 1990s, and in the era of minimally invasive surgery, laparoscopic surgery was adopted for the operation of HD [
10]. The laparoscopic approaches were made with a smaller incision of the skin and showed good outcomes in both the short and long term in many studies [
81112]. For short-segment lesions from the rectum to the sigmoid colon, a transanal approach without laparotomy has been introduced and is now widespread [
213].
However, some controversy persists, where TERPT procedure showed worse results than a pull-through operation with laparoscopy or laparotomy [
1415]. Incontinence due to traction of the anal sphincter was considered a weakness of TERPT procedure. Traction of the anal sphincter is required to perform TERPT procedure for endorectal dissection and anastomosis. Traction of the anal canal is known to cause serious problems in adults. In some studies, TERPT procedure had inferior outcomes to pull-through with an abdominal incision with regard to incontinence [
15]. The reliability of intraoperative frozen sections during TERPT procedure is another point of controversy. Some studies have revealed a discrepancy between the frozen section and final pathologic diagnosis, with significant impact on clinical outcomes. Some surgeons preferred staged operations with enterostoma formation and pathologic confirmation [
1617]. Despite these issues and controversies, TERPT procedure is preferred as a surgical option for short-segment HD, if we can get reliable pathologic results and good surgical skills.
Other studies revealed that HD patients had small problems with fecal control only at the early stage, which improved with age without social problems [
4]. Furthermore, anorectal manometry revealed no significant differences between TERPT procedure and pull-through with abdominal incisions [
18]. In this study, incontinence was not a serious problem at all investigated ages. Minor soiling (staining <1/week, no change in underwear required) was not reported as a rare condition in the normal population (<33%) [
5]. Therefore, minor soiling without any accompanying problems would not be considered a poor postoperative functional outcome, and providing strict treatment should be carefully considered. Increased stooling frequency could be affected by traction of the anal canal or weakness of the sphincter muscle. The stooling frequency scores also improved with age. The traction of the anus would not cause severe problems when it was not too excessive.
Nearly 15% of all patients with HD who underwent TERPT procedure have been reported to experience persistent bowel symptoms, with constipation as the main problem [
3]. Abnormalities in the innervation and function of the pulled through colon and internal anal sphincter, and surgical complications may contribute to the development of constipation [
11920]. Previous studies have reported that constipation in HD becomes milder or subsides with time after early childhood, similar to functional constipation [
1]. In this study, 4.9% of patients suffered from constipation, which is a similar ratio to that of the normal population (8%) [
5]. Of the patients, 5.4% defecated every other day. However, the enrolled patients (or parents) in this study might have thought that it was not constipation. In the questionnaire, there was no explanation for constipation. TERPT patients would seem to have an excellent defecation ability in this study; lower rates of constipation than those in other studies may be affected by it.
In the normal population of a previous study, patients aged 4–7 years did not experience social problems, despite the occurrence of fecal soiling [
5]. In the TERPT patients (or their parents) in this study, minor degrees of fecal soiling caused them to experience social problems, for example, the foul odor. It is difficult to determine the exact causes. TERPT patients might be more sensitive to smell because of their experiences. The thought that HD patients frequently have problems with defecation, which relates to a bad smell, could have an effect. The changes in social problem scores were similar to those in the fecal soiling scores. Despite better or similar scores in constipation, fecal accident, and ability to hold back defecation, lower scores in social problems were obtained in some age groups of TERPT patients. It might be suggested that fecal soiling affected the scores of social problems more than any other part and might explain the discrepancy between better scores in constipation, fecal accidents, and ability to hold back defecation, and lower scores in social problems. Further in-depth interviews and studies are needed to clarify these differences.
Overall, the BFS of TERPT patients was similar to that of the normal population. Before this investigation, the authors presupposed that TERPT patients could have problems with soiling, accidents, constipation, and social issues. As the patients get older, the overall BFS is improved and is close to that of the normal population. In a previous study consisting of adults, with more than 70% having undergone a Duhamel operation for HD, patients had significant impairment in bowel function [
6]. Little information is available regarding the adult outcomes of TERPT procedure. Therefore, further studies are required. HD-associated enterocolitis has been reported to occur in 6%–45% of patients and usually occurs within the first few years after pull-through. The lack of consensus on the definition of HD-associated enterocolitis has been affected by a wide range of reported incidences [
21]. In this study, we defined HD-associated enterocolitis as enterocolitis that required admission therapy without other infections or inducible factors. Our incidence of HD-associated enterocolitis is 13.4%, which seems to be tolerable.
This study has some limitations. Validation of BFS for the normal population was performed on individuals of the Finnish ethnicity [
5]. These days, Koreans are much more westernized, but there are still significant differences in race, lifestyle, and eating habits. Although there was an article about the bowel habits of Korean children, the questionnaire and answers were not appropriate for investigating the functional outcome of TERPT procedure [
22]. The BFS used in this study was received at an outpatient clinic along with the questionnaire in front of the operator. This introduces considerable potential for bias, as patients may be unwilling to report unfavorable results to their surgeon. However, this study has value in that it presents mid- and long-term results after bowel training of TERPT procedure in a relatively large number of HD patients. This study included only 1 patient with developmental delay (1 with Down syndrome) and no syndromic cases. The small number of these patients may have contributed to the good functional outcomes in this study.
In conclusion, TERPT patients would have favorable mid-and long-term results compared to the normal population. Most patients who had a lower BFS at an early age had improved functional outcomes with age in general. However, some patients had persistently poor functional outcomes. Further investigation is needed to explore the factors that interfere with the improvement of functional outcomes.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download