Abstract
Purpose
The study was aimed at assessing the prevalence of depression in individuals with fecal incontinence (FI) and the relationship between the symptoms of depression and the severity of objective test parameters.
Methods
Patients with FI for over 3 months were included in the study. The exclusion criteria were (1) diagnosis or treatment of the pelvic organ prolapse syndrome, (2) previous anorectal surgery, (3) inflammatory bowel disease, (4) previous diagnosis of psychiatric disorder, and (5) inability to read or understand the questionnaire themselves. The questionnaire included the Beck Depression Inventory-II (BDI-II) for measuring depression, and 142 patients were included for analysis.
Results
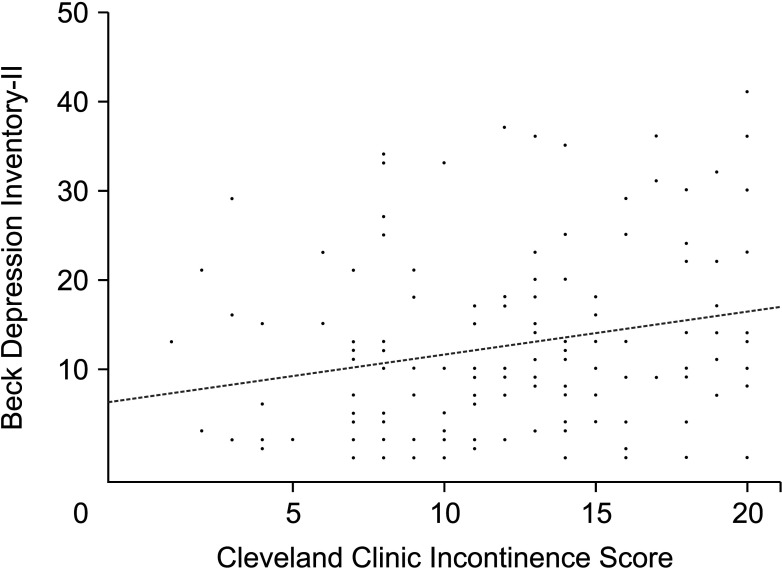
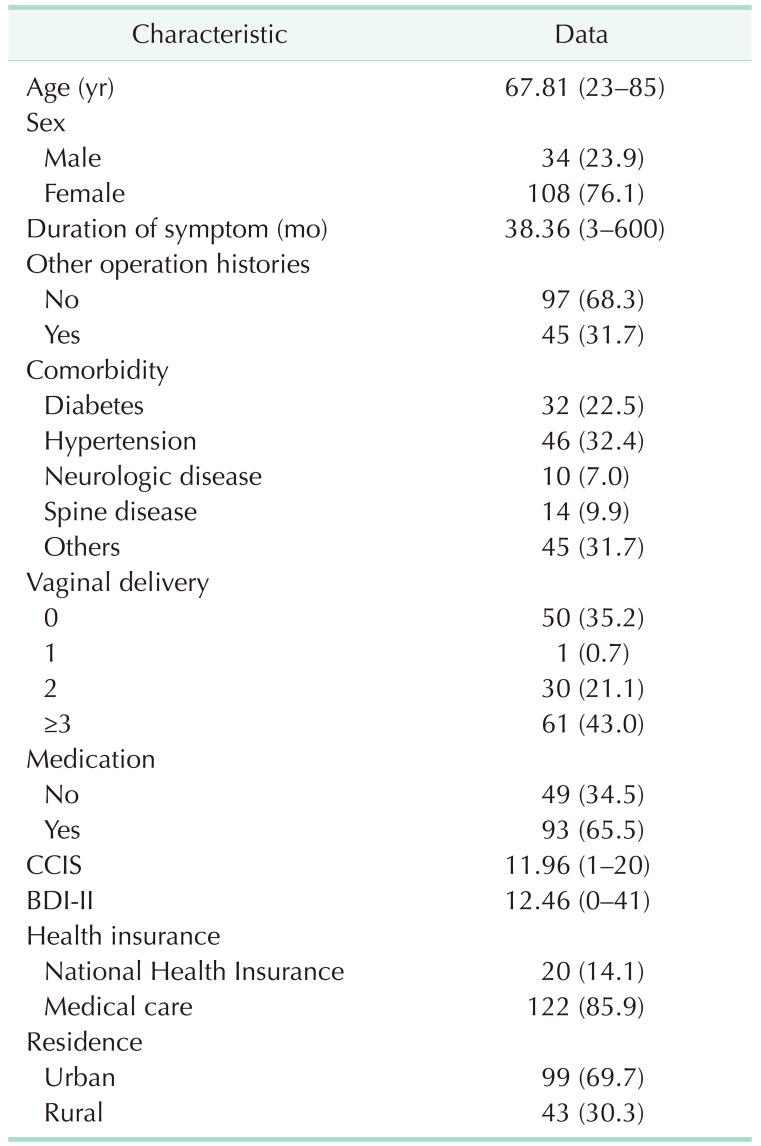
Of the 142 patients, 34 were males and 108 were females, with a mean age of 67.8 years. The mean duration of FI symptoms was 38.36 months (range, 3–600 months). The mean Cleveland Clinic Incontinence Score and BDI-II were 11.96 ± 4.76 and 12.46 ± 9.84, respectively. The Cleveland Clinic Incontinence Score showed a positive correlation with the BDI-II score (P = 0.005). Of the 142 patients, 99 showed minimal to mild BDI-II scores, and 43 showed moderate-to-severe BDI-II scores. The multivariable logistic regression analysis showed that health insurance status was related to the depression in FI patients.
Fecal incontinence (FI) refers to the involuntary passage or uncontrolled discharge of feces or flatus [1]. FI is common in women, elderly patients, and institutionalized patients [12]. The prevalence of FI is unclear, and it might differ based on the method, target population, clinical setting, and definition [3]. The prevalence of FI is increasing rapidly with the surge in the number of elderly patients [3]. The prevalence of FI is approximately 7%–9% in women [24]. One report predicted that the number of patients with FI within the United States would increase by 59% from 2010 to 2050 [5].
Patients with FI experienced several problems, including emotional distress. These individuals frequently experience abnormalities during defecation, such as diarrhea and constipation [2]. Patients with FI also undergo pruritus ani, skin irritation, or urinary tract infections due to leaking stools [6]. Of the patients with FI, 47% used pads, and 53% had altered their lifestyle [2]. These symptoms affected the quality of life of the patients [6]. Although there is little research on the relationship between FI and depression, patients with pelvic organ prolapse show significant depression symptoms [7].
Albeit several studies have reported the relationship between depression and the severity of the pelvic organ relapse symptoms, few studies have assessed the association of depression symptoms and the severity of FI [89]. While FI also occurs during pelvic organ prolapses, there needs to be an independent understanding of FI and depression. This becomes important with the increasing incidence of FI in the population and its prevalence is only expected to increase in the future [5]. The study aimed at assessing the prevalence of depression symptoms during FI, the relationship between these symptoms and FI, and the severity of objective test parameters.
This retrospective study was conducted at the Yeungnam University Medical Center and Hwanggeumbit Surgery Clinic (Daegu, Korea) between January 2015 and October 2019. The study was approved by the Institutional Review Board (IRB) of the Yeungnam University Medical Center (No. 2020-02-008). IRB exempted the study from obtaining informed consent from the patients.
The patients who were diagnosed with FI and were symptomatic for over 3 months were included. Patients diagnosed or treated for pelvic organ prolapse syndrome, those with previous anorectal surgery, those with inflammatory bowel disease, those with a previous diagnosis of psychiatric disease, and those unable to read or understand the questionnaire themselves were excluded. A total of 184 patients were enrolled in this study, of which 5 had previous pelvic organ prolapse syndrome, 28 had previous anal surgery, 2 had major depressive disorders, and 2 could not understand the questionnaire. Finally, 142 patients were included in this study.
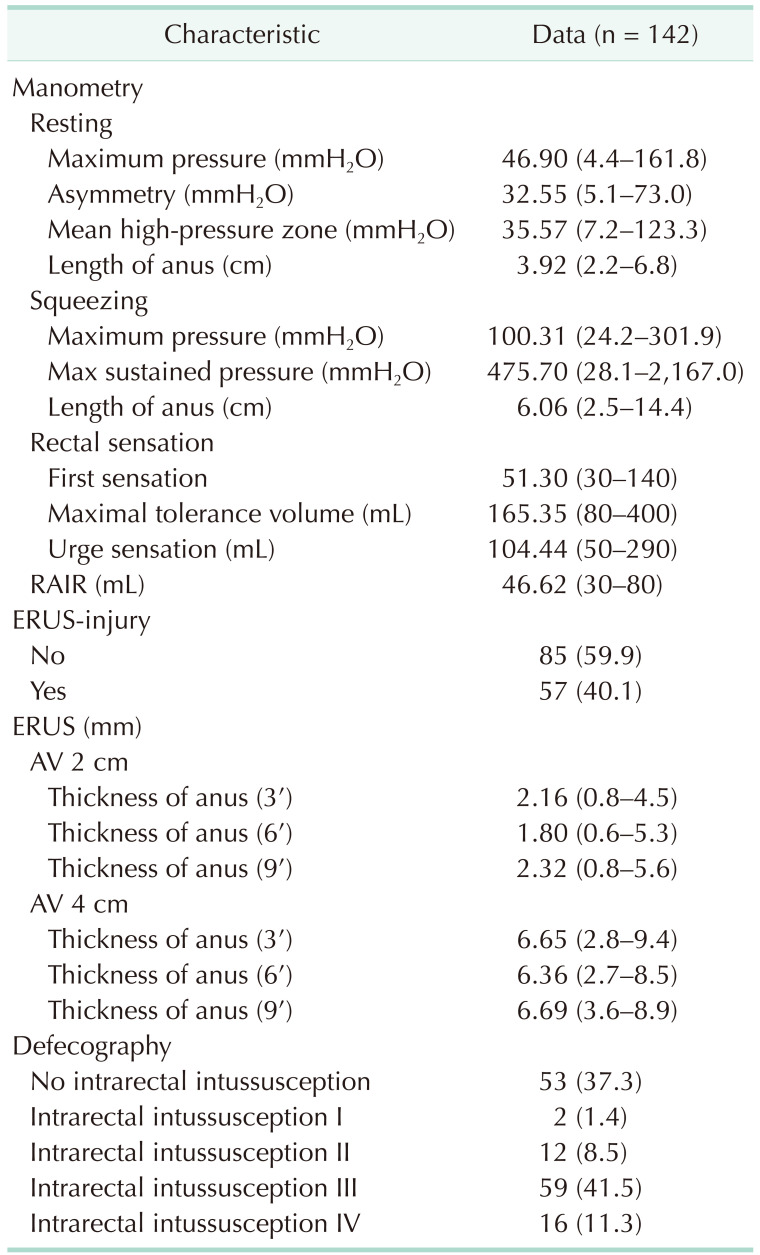
The patients underwent standardized evaluations by colorectal surgeons. The physicians evaluated the patient's symptoms, medical history, Cleveland Clinic Incontinence Score (CCIS), and social status. The patients underwent anorectal manometry, transrectal ultrasonography, and defecography. Anorectal manometry variables in the resting state included maximal pressure, mean maximal pressure zone, and length of the anus. The variables of anorectal manometry in the squeezing status included maximal pressure, maximal sustain pressure, and the length of the anus. The physicians also checked for anal sphincter injury using transrectal ultrasonography. The variable of transrectal ultrasonography included the thickness of the anal sphincter at anal verge 2 cm and anal verge 4 cm. All patients underwent defecography to evaluate anorectal conditions. The authors used Oxford rectal prolapse grading system to access internal rectal prolapse [10].
Questionnaires for depression and anxiety were completed during the anorectal physiological tests. The questionnaires used were the Beck Depression Inventory-II (BDI-II). The BDI-II is one of the most widely used tests for measuring depression [1112]. The BDI is a self-report scale designed to evaluate the presence and severity of depression symptoms. It consists of 21 items, including cognitive, emotional, motivational, and physical symptoms of depression. Each question is scored from 0 to 3 points, and the total score ranges from 0 to 63, indicating that higher the total score, the more severe is the depression. It considers a total score of 0–9 as the minimal range, 10–15 mild, 16–23 moderate, and 24–63 severe.
Statistical analyses were conducted using IBM SPSS Statistics ver. 25 (IBM, Armonk, NY, USA). The results of quantitative variables were expressed as mean ± standard deviation. The results of the qualitative variables were expressed as numbers and percentages. All continuous data were analyzed using the Student t-test. All categorical data were analyzed using the chisquare or Fisher exact test. Univariate and multivariate analyses were performed using a linear logistic regression analysis. Statistical significance was indicated when the P-value was less than 0.05.
Of the 142 patients, 34 were males, and 108 were females with a mean age of 67.8 years (range, 13–83 years). The mean duration of FI symptoms was 38.36 months (range, 3–600 months). Among the women, 61 of 108 patients (56.5%) underwent over 3 vaginal deliveries. The mean CCIS and BDI-II were 11.96 ± 4.76 and 12.46 ± 9.84, respectively. Table 1 summarizes the clinical and demographic characteristics of the patients. The CCIS was positively correlated with the BDI-II score (P = 0.005) (Fig. 1).
Table 2 shows the physiological characteristics of patients with FI. The patient showed lower maximal resting pressure and maximal squeezing pressure. Fifty-seven patients (40.1%) had anal injuries as determined by the endorectal ultrasonography. Of the 142 patients, 89 (62.7%) underwent concomitant rectal intussusception.
Of the 142 patients, 64 and 35 patients showed minimal and mild BDI-II scores, respectively. Twenty-three patients and 20 patients showed moderate and severe BDI-II scores, respectively. As per their score, 99 patients were placed in the non-depressive mood group, while 43 patients were placed in the depressive mood group.
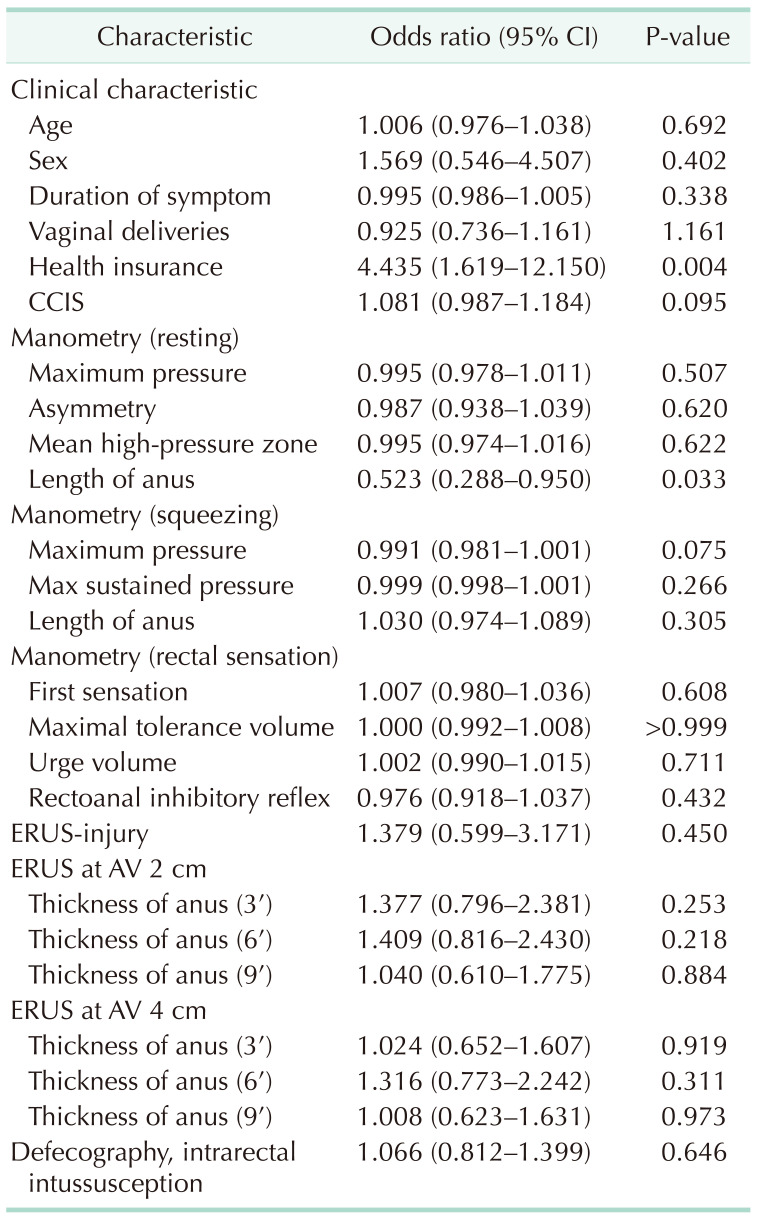
Univariate logistic regression analysis showed that the status of health insurance and length of the anus of manometry were related to the depressed mood in FI patients (Table 3). The multivariable logistic regression analysis showed that the status of health insurance increased the odds of depression in FI patients (odds ratio, 4.617; 95% confidence interval, 1.617–13.182; P = 0.004).
FI is ubiquitous and affects people of all ages. However, its prevalence is under-reported, and its manifestation is challenging to assess because of the associated embarrassment and taboo nature. While reported estimates of prevalence vary widely depending on the clinical setting, incontinence increases with age and is common in women and nursing home residents [1]. The United States National Health and Nutrition Examination Survey reported a prevalence of 8.4% among non-institutionalized adults [3]. A telephone survey in the United States revealed a prevalence of 2.2% and a women-to-men ratio of 63% vs. 37% [13]. In another study, FI occurred in 25%–35% of institutionalized patients and 10%–25% of hospitalized elderly patients [14]. In Korea, the prevalence of FI was reportedly 15.5% and in most cases, it affected the quality of life of the patients [15].
The evaluation of FI involves obtaining a detailed history of the affected individual, imaging tests of the anorectum, and an appropriate physiological test. Of these, anorectal manometry with rectal sensory testing is used to confirm the functional problems of the anal sphincter and abnormal rectal sensation [16]. In patients with FI, most resting and squeeze sphincter pressures show low pressure [1718]. Patients with FI showed significantly lower anal mean sustained squeeze pressure and maximal squeeze pressure [16]. Sensory testing by rectal balloon distention can be used to evaluate sensory responses and compliance for the rectum. In sensory testing, the rectal capacity was smaller and the volume for inducing reflex anal relaxation was higher in FI patients than in controls [181920]. Patients with FI frequently show internal rectal intussusception [21]. The symptoms of FI are associated with worsening grades of intussusception [21]. The length of surgical anal canal in normal people was reported as approximately 4.2 cm [22]. The anal length of resting status in patients with FI was reported 2.16 ± 1.22 mm [23]. Although this study was conducted in patients with FI, the anal length was similar to that of other studies.
There have been fewer reports on the relationship between FI and depression. FI affects patient's lives and is perceived as a severe loss that accelerates anger, grief, shame, and depression [24]. In a study that included patients with functional gastrointestinal disorders, patients with soiling showed higher depression scores than patients without soiling [25]. Female patients with pelvic floor dysfunction showed a threefold higher prevalence of depression symptoms [8]. In another study, approximately one-third of postmenopausal women with pelvic floor dysfunction experienced symptoms of depression [9].
In this study, we focused on the psychological burden, especially depression, among the various infirmities caused by FI. Among the factors related to FI, the CCIS and the social status of the patients were related to depression. Patients with a high CCIS showed higher BDI-II scores. The authors also considered the relationship between several objective results and depression in patients with FI, but these indicators are not directly related to depression. The length of the anus in resting was not significant in multivariate analysis. In other studies, the length of the anus was significantly correlated with the pressures in the resting and squeezing phases [23]. However, the anal length did not show any association with Fecal Incontinence Severity Index and Fecal Incontinence Quality of Life Scale [23]. The authors believe that anal length may be an important factor in several functional aspects in patients with FI, but this suggests that it may be less correlated with subjective symptoms. Therefore, the treatment of FI itself is important in the treatment of depression by FI, but the improvement of the patient's surroundings, emotional support, and empathy are also important. Patients do not spontaneously report their symptoms to their doctors, and at least of them neglect their illness mainly due to shyness, fear of surgery, and false beliefs [26]. In addition to psychological progress, FI is a decisive risk factor for institutionalization and debilitation [27]. The factors related to depression were the patient's symptoms or the social status to which the patient belonged. Recent meta-analysis showed that individuals with low socioeconomic status had higher odds of being depressed [28]. Socioeconomic disadvantages can lead to imbalances in access to treatment and care. In addition to that, individuals with low socioeconomic status are exposed to more stress, social challenges, and adversity, but have fewer interpersonal resources to cope with these stressful events [29]. There's also compelling evidence that low social status affects multimodality and increases depressive symptoms in general medical conditions [30]. However, the exact mechanism by which social status can affect the risk of depression in FI was not fully understood and need to be investigated.
We recognize that this study has several limitations, including the fact that is based on retrospective data collection and a small sample size. This study did not have a controlled group and did not compare the observations with the normal group. However, based on this study, it is expected to be the basis for conducting a study on the effect of FI treatment on mood disorders.
In this study, we confirm the degree and incidence of mood disorders in patients with FI and identify the factors that influence the deterioration of mood disorders. Mood disorders related to FI are also affected by the severity of the subjective symptoms or the surrounding environment than the objective indicators derived from the test.
References
1. Rao SS. American College of Gastroenterology Practice Parameters Committee. Diagnosis and management of fecal incontinence. American College of Gastroenterology Practice Parameters Committee. Am J Gast roenterol. 2004; 99:1585–1604.
2. Melville JL, Fan MY, Newton K, Fenner D. Fecal incontinence in US women: a population-based study. Am J Obstet Gynecol. 2005; 193:2071–2076. PMID: 16325618.

3. Ditah I, Devaki P, Luma HN, Ditah C, Njei B, Jaiyeoba C, et al. Prevalence, trends, and risk factors for fecal incontinence in United States adults, 2005-2010. Clin Gastroenterol Hepatol. 2014; 12:636–643. PMID: 23906873.

4. Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008; 300:1311–1316. PMID: 18799443.

5. Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in US women: 2010 to 2050. Obstet Gynecol. 2009; 114:1278–1283. PMID: 19935030.
6. Saldana Ruiz N, Kaiser AM. Fecal incontinence: challenges and solutions. World J Gastroenterol. 2017; 23:11–24. PMID: 28104977.
7. Ghetti C, Lowder JL, Ellison R, Krohn MA, Moalli P. Depressive symptoms in women seeking surgery for pelvic organ prolapse. Int Urogynecol J. 2010; 21:855–860. PMID: 20333505.

8. Mazi B, Kaddour O, Al-Badr A. Depression symptoms in women with pelvic floor dysfunction: a case-control study. Int J Womens Health. 2019; 11:143–148. PMID: 30863189.
9. Ai F, Deng M, Mao M, Xu T, Zhu L. Depressive symptoms screening in postmenopausal women with symptomatic pelvic organ prolapse. Menopause. 2018; 25:314–319. PMID: 29040216.

10. Gosselink MP, Adusumilli S, Gorissen KJ, Fourie S, Tuynman JB, Jones OM, et al. Laparoscopic ventral rectopexy for fecal incontinence associated with high-grade internal rectal prolapse. Dis Colon Rectum. 2013; 56:1409–1414. PMID: 24201396.

11. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961; 4:561–571. PMID: 13688369.

12. Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996; 67:588–597. PMID: 8991972.
13. Nelson R, Norton N, Cautley E, Furner S. Community-based prevalence of anal incontinence. JAMA. 1995; 274:559–561. PMID: 7629985.

14. Szurszewski JH, Holt PR, Schuster M. Proceedings of a workshop entitled “Neuromus cul a r func t ion and dysfunction of the gastrointestinal tract in aging”. Dig Dis Sci. 1989; 34:1135–1146. PMID: 2545427.
15. Joh HK, Seong MK, Oh SW. Fecal incontinence in elderly Koreans. J Am Geriatr Soc. 2010; 58:116–121. PMID: 20002514.

16. Mion F, Garros A, Brochard C, Vitton V, Ropert A, Bouvier M, et al. 3D high-definition anorectal manometry: values obtained in asymptomatic volunteers, fecal incontinence and chronic constipation: results of a prospective multicenter study (NOMAD). Neurogastroenterol Motil. 2017; 29:e13049.

17. Read NW, Bartolo DC, Read MG. Differences in anal function in patients with incontinence to solids and in patients with incontinence to liquids. Br J Surg. 1984; 71:39–42. PMID: 6689968.

18. Felt-Bersma RJ, Klinkenberg-Knol EC, Meuwissen SG. Anorectal function investigations in incontinent and continent patients: differences and discriminatory value. Dis Colon Rectum. 1990; 33:479–486. PMID: 2351000.
19. Read NW, Harford WV, Schmulen AC, Read MG, Santa Ana C, Fordtran JS. A clinical study of patients with fecal incont inence and diarrhea. Gastroenterology. 1979; 76:747–756. PMID: 422003.
20. Sun WM, Read NW, Donnelly TC. Anorectal function in incontinent patients with cerebrospinal disease. Gastroenterology. 1990; 99:1372–1379. PMID: 2210244.

21. Hawkins AT, Olariu AG, Savitt LR, Gingipally S, Wakamatsu MM, Pulliam S, et al. Impact of rising grades of internal rectal intussusception on fecal continence and symptoms of constipation. Dis Colon Rectum. 2016; 59:54–61. PMID: 26651113.

22. Nivatvongs S, Stern HS, Fryd DS. The length of the anal canal. Dis Colon Rectum. 1981; 24:600–601. PMID: 7318624.

23. Zutshi M, Salcedo L, Hammel J, Hull T. Anal physiology testing in fecal incontinence: is it of any value? Int J Colorectal Dis. 2010; 25:277–282. PMID: 19902225.

24. Specht JK. 9 Myths of incontinence in older adults: both clinicians and the over-65 set need to know more. Am J Nurs. 2005; 105:58–68.
25. Bouchoucha M, Devroede G, Rompteaux P, Bejou B, Sabate JM, Benamouzig R. Clinical and psychological correlates of soiling in adult patients with functional gastrointestinal disorders. Int J Colorectal Dis. 2018; 33:1793–1797. PMID: 29987361.

26. Erdem N, Chu FM. Management of overactive bladder and urge urinary incontinence in the elderly patient. Am J Med. 2006; 119(3 Suppl 1):29–36. PMID: 16483866.

27. Brown JS, Vittinghoff E, Wyman JF, Stone KL, Nevitt MC, Ensrud KE, et al. Urinary incontinence: does it increase risk for falls and fractures?: study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 2000; 48:721–725. PMID: 10894308.
28. Lorant V, Deliège D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003; 157:98–112. PMID: 12522017.

29. Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annu Rev Psychol. 2011; 62:501–530. PMID: 20636127.

30. Sullivan S, Vaccarino V. Low socioeconomic status and depression: a double jeopardy for cardiovascular disease? J Psychosom Res. 2019; 121:6–7. PMID: 31014547.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download