Abstract
Purpose
Despite increasing number of reports on Enhanced Recovery After Surgery program (ERAS) and readmission after pancreaticoduodenectomy (PD) from Western countries, there are very few reports on this topic from Asian countries. This study aimed to evaluate the effects of ERAS on hospital stay and readmission and to identify reasons and risk factors for readmission after PD.
Methods
This retrospective cohort study included 670 patients who underwent open PD from January 2003 to December 2017. The patients were classified into ERAS (n = 352) and non-ERAS (n = 318) groups. Patients' characteristics, perioperative outcomes, and readmission rates were compared.
Results
There were no significant differences in the postoperative complication rates between the groups. The mean postoperative hospital stay was significantly shorter in the ERAS group (24.5 vs. 18.0 days, P < 0.001), but the 90-day readmission rate was similar in the 2 groups (9.1% vs. 8.5%, P = 0.785). Complications associated with pancreatic fistula (42.4%) were the most common cause for readmission. In the multivariate analysis, diabetes mellitus (odds ratio [OR], 1.84; 95% confidence interval [CI], 1.05–3.24; P = 0.034), preoperative non-jaundice (OR, 0.45; 95% CI, 0.25–0.82; P = 0.009) and severe postoperative complications (OR, 4.12; 95% CI, 2.34–7.26; P < 0.001) were identified as risk factors for readmission.
Pancreaticoduodenectomy (PD) is associated with high morbidity and mortality due to the innate complexity of the procedure. Although operative mortality at specialized centers have recently decreased to less than 1%–2%, morbidity continues to remain high ranging from 27% to 47%. This inevitably results in a prolonged postoperative hospital stay compared to other gastrointestinal surgeries [12].
Enhanced Recovery After Surgery (ERAS) programs were introduced to provide standardized management of patients and prevent dissipation of medical resources caused by increased hospital stay related to postoperative complications. They were initially implemented in colorectal surgery. Several studies have shown that earlier hospital discharge and reduced complications were associated with introduction of ERAS program after colorectal surgery [34]. With extension to a variety of surgical fields, the ERAS guideline for PD was proposed by the ERAS society in 2012 [5]. Some non-randomized studies and a recent randomized controlled trial have shown that utilization of ERAS protocols in patients undergoing PD contributed to early recovery without compromising surgical outcomes [6] like other abdominal surgeries [78910]. However, concerns were raised that ERAS might inadvertently increase hospital readmission [11]. The advantage of ERAS against the risk of readmission remains unclear in patients undergoing PD, especially with its high risk of morbidity because full postoperative recovery compared to other gastrointestinal surgeries is known to take longer [12]. Unintended readmission after PD, that is reported to increase hospital cost for patients as well as morbidity and mortality, is considered to be a quality metric for surgery [13]. Therefore, it is important to evaluate the association between ERAS and readmission and to identify the risk factors for the same. This will help prepare strategies for such ‘high-risk patients’ and prevent unnecessary expenses caused by readmission.
Several studies have analyzed the risk factors for readmission after PD in efforts to improve surgical standards and reduce preventable hospital expenses caused by readmission. However, most of studies were published from Western countries, especially from the United States, after implementation of the Medicare act. The impact of ERAS on postoperative hospital stay and readmission after PD has been rarely investigated in Asian institutions. They have a different healthcare system and hospital environment when compared to Western institutions. Hence, this study aimed to evaluate the effect of ERAS on postoperative hospital stay and readmission after PD and to identify common reasons and risk factors for readmission in a Korean tertiary care center.
A total of 867 patients who underwent PD from January 2003 to December 2017 at Seoul National University Bundang Hospital were identified from a prospectively collected database. The operation was performed by 4 experienced surgeons who had specialized in hepato-pancreato-biliary surgery: 2 surgeons had mainly been performing PD for 15 years, 1 surgeon for 10 years (from 2008 to 2017), and the other surgeon had been performing the same for 4 years (from 2011 to 2014). Operations by the first 2 surgeons accounted for 82% of all PD cases. Minimally invasive surgery was performed in 197 patients, mainly after the implementation of the ERAS protocol. These patients were excluded to rule out the possibility of minimally invasive surgery affecting hospital stay after PD. Finally, 670 patients were enrolled in this retrospective study.
Readmission was defined as ‘unintended readmission within 90 days after discharge from the hospitalization for PD’. The patients were classified into 2 groups according to the timing of introduction of ERAS in 2012 as ERAS group (n = 352) and non-ERAS group (n = 318). We compared postoperative outcomes between the groups to evaluate the effect of the ERAS program on length of postoperative hospital stay and readmission. We also investigated the incidence of and reasons for readmission within 90 days and analyzed the predictive factors for readmission. In the multivariate analysis for readmission, 16 patients who died during index admission were excluded.
This study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Institutional Review Board at Seoul National University Bundang Hospital (No. B-2006-618-111). Written informed consent was waived due to its retrospective nature.
The following data were retrieved from the database and analyzed. Preoperative variables (age, sex, body mass index [BMI], American Society of Anesthesiologists [ASA] physical status classification, underlying disease, operative indication, preoperative albumin, presence of jaundice, and preoperative biliary drainage), operative data (type of surgery, combined resection of other organs, operative time, estimated blood loss, and intraoperative transfusion), and postoperative data (complication rate and severity according to the Clavien-Dindo classification, clinically relevant postoperative pancreatic fistula [CR-POPF], delayed gastric emptying, biliary fistula, ileus, wound complications, postoperative hemorrhage [PPH], pulmonary complications, and postoperative hospital stay). CR-POPF and delayed gastric emptying was based on the definitions laid down by the International Study Group of Pancreatic Surgery [1415].
Enhanced recovery after surgery (ERAS) protocol and conventional protocol were presented in Table 1. An ERAS program was implemented for all patients who underwent PD from January 2012. Patients were allowed to have food till midnight on the day before the operation, without bowel preparation. Nasogastric tube was not inserted preoperatively. To prevent deep vein thrombosis, intermittent pneumatic compression was applied from the operation room till the patient was transferred to the ward after surgery. Patients were allowed to drink water on postoperative day (POD) 1 and soft blended diet from POD 2. Meanwhile, patients on the conventional management protocol were allowed to have a soft blended diet only after passage of flatus. Intravenous patient-controlled pain relief was administered till POD 3–5 following which oral analgesics were used. One of the major differences between ERAS and conventional protocol is the establishment of criteria for specific management. Abdominal drains were removed after performing an abdominal CT scan on POD 5 if the following criteria were met: (1) drain fluid amylase of <600 U/L, (2) drain volume of <300 mL, and (3) no complicated intra-abdominal fluid collection observed on CT. Patients who (1) had no evidence of infection, (2) had their abdominal drain removed, (3) could tolerate an oral diet without intravenous fluid infusion, and (4) had achieved adequate pain control with oral analgesics were discharged.
Continuous data are presented as the mean ± standard deviation. The chi-square test was used to compare categorical variables. Independent samples (Student t-test), one-way analysis of variance, and repeated-measures analysis of variance were used, as appropriate, to compare continuous variables between the groups. The linear regression model was used in multivariate analysis to determine the prognostic significance of the variables that were found to be significant in univariate analyses. In all analyses, a P-value of <0.05 (2-sided) was considered statistically significant. IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA) was used for all analyses.
To estimate the yearly trend effect of ERAS on hospital stay, we considered a segmented linear regression, which is one of the interrupted time series analyses. We regarded the year 2012 as the intervention time point for the implementation of ERAS and divided the time series into pre- and post-2012 segments. Segmented linear regression was able to compare the changes in trends of the hospital before and after the introduction of ERAS protocol. Segmented regression requires data collected regularly over time, and organized at equally spaced intervals. The time series of the outcome of interest is used to establish an underlying trend, which is “interrupted” by an intervention at a known point in time. Segmented regression models fit a least squares regression line to each segment of the independent variable, time, and thus, assume a linear relationship between time and the outcome within each segment.
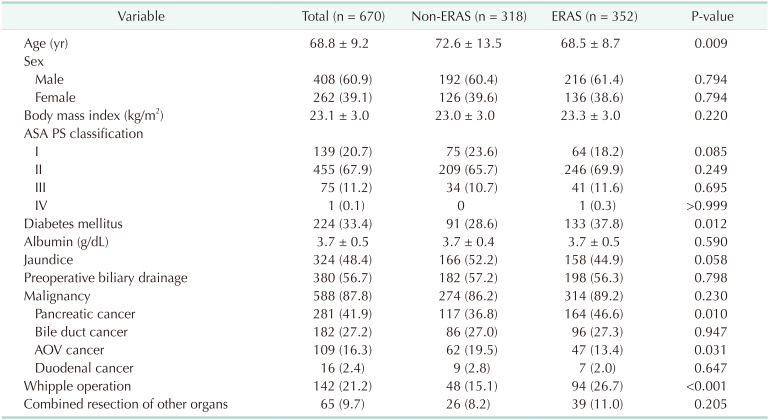
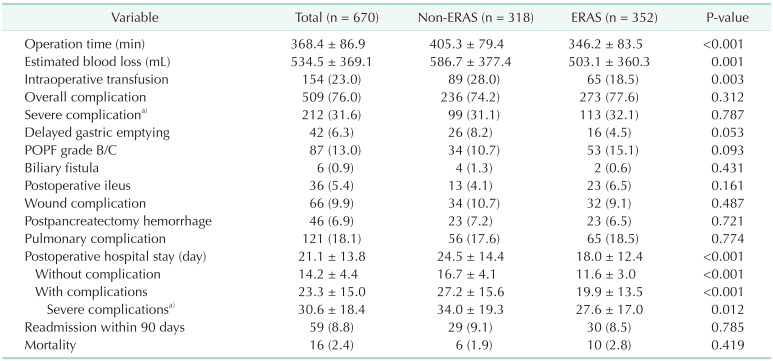
A comparison of patient demographics between the ERAS and non-ERAS groups is shown in Table 2. There were no significant differences between the groups in terms of sex, BMI, ASA classification, preoperative albumin level, preoperative jaundice, preoperative biliary drainage, and combined resection of other organs. However, the non-ERAS group was significantly older than the ERAS group (68.5 vs. 72.6 years, P = 0.009). The ERAS group had more patients with diabetes mellitus (DM) than the non-ERAS group (37.8% vs. 28.6%, P = 0.012). Proportions of pancreatic cancer (36.8% vs. 46.6%, P = 0.010) and Whipple operation (15.1% vs. 26.7%, P < 0.001) were higher in the ERAS group. When postoperative outcomes were compared between the groups (Table 3), the operative time (405.3 ± 79.4 minutes vs. 346.2 ± 83.5 minutes, P < 0.001), estimated blood loss (586.7 ± 377.4 mL vs. 503.1 ± 360.3 mL, P = 0.001) and the rate of intraoperative transfusion (28.0% vs. 18.5%, P = 0.003) were significantly greater in the non-ERAS group. There were no differences between the groups in terms of overall/severe (Clavien-Dindo classification ≥ IIIa) postoperative complications and mortality. The postoperative hospital stay was notably shorter in the ERAS group (24.5 ± 14.4 days vs. 18.0 ± 12.4 days, P < 0.001) regardless of complications, but 90-day readmission rates were similar between the groups (9.1% vs. 8.5%, P = 0.785).
Among 670 patients, 59 patients (8.8%) were readmitted after their index admission for surgery. The median time from discharge to readmission was 14 days. Fig. 1A shows the temporal change in readmission rate and length of postoperative hospital stay per year. While a steadily decreasing trend was seen in postoperative hospital stay, a slight increase was noted in the trend of readmission rates. Fig. 1B shows that the decreasing rate of postoperative hospital day was faster after introduction of ERAS protocol (2012) and its trend was statistically significant (adjusted R square = 0.6893, P < 0.001). Table 4 describes the reasons for readmission and outcomes of readmission. The most common cause of readmission was intra-abdominal abscess (n = 15, 25.4%) followed by bleeding (n = 14, 23.7%), wound complication (n = 8, 13.6%), fever (n = 6, 10.2%), small bowel obstruction (n = 4, 6.8%), delayed gastric emptying (n = 4, 6.8%), abdominal pain (n = 3, 5.1%), and poor oral intake (n = 2, 3.4%) (Table 4). There were no significant differences of readmission reasons between the groups, except intra-abdominal abscess that was associated with POPF. The intra-abdominal abscess was treated by percutaneous drainage and antibiotics. Bleeding was controlled by transcatheter arterial embolization and transfusion. Wound complications were mostly treated by antibiotics and frequent dressing, but wound revision was required in some severe cases. The duration of hospital stay, requirement of intensive care unit admission, and mortality after readmission were similar between the ERAS and non-ERAS groups.
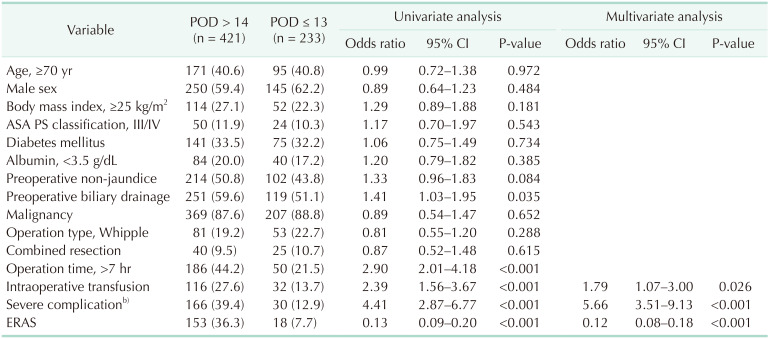
In the univariate analysis, preoperative biliary drainage (P = 0.035), long operation time (>7 hours, P < 0.001), intraoperative transfusion (P < 0.001), and other severe complications (P < 0.001) were significantly associated with prolonged hospital stay (>POD 14) (Table 5). ERAS was negatively associated with prolonged hospital stay (P < 0.001). In the multivariate analysis, intraoperative transfusion (odds ratio [OR] 1.79; 95% confidence interval [CI], 1.07–3.00; P = 0.026) and severe complications (OR, 5.66; 95% CI, 3.51–9.13; P < 0.001) were identified as significant risk factors for prolonged hospital stay, whereas ERAS was a significantly negative factor (OR, 0.12; 95% CI, 0.08–0.18; P < 0.001).
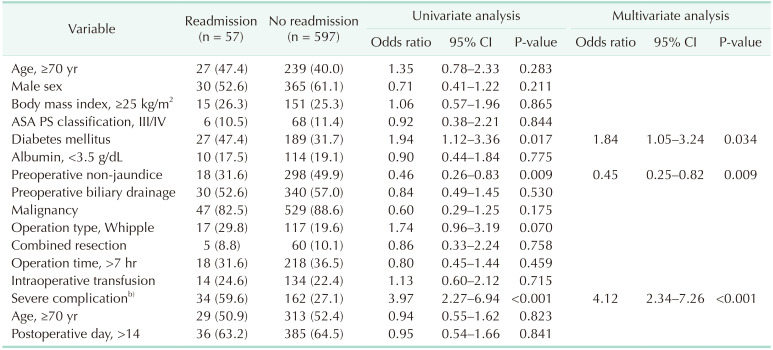
In the univariate analysis, DM (P = 0.017), preoperative nonjaundice (P = 0.009), and severe complications (P < 0.001) were significantly associated with readmission after PD (Table 6). In the multivariate analysis, DM (OR, 1.84; 95% CI, 1.05–3.24; P = 0.034), preoperative non-jaundice, and severe complications (OR, 4.12; 95% CI, 2.34–7.26; P < 0.001) were statistically significant risk factors for 90-day readmission.
This study evaluated the effect of ERAS on postoperative hospital stay and readmission after PD in a Korean medical care milieu that is different from institutions in Western countries. The results showed that implementation of ERAS in patients who underwent PD did not significantly decrease the postoperative complication rate, but it reduced postoperative hospital stay without increasing 90-day readmission rate. Segmented regression analysis of interrupted time series data showed an additional yearly decline of hospital stay after the implementation of ERAS. The effect of ERAS on reduction of postoperative hospital stay was present in patients, with and without postoperative complications. These findings were similar to reports published from Western countries. In the multivariate analysis, ERAS was seen to significantly reduce postoperative hospital stay but was not associated with an increased readmission rate. In comparison, DM and severe postoperative complications were identified as significant risk factors for readmission. These findings suggest that the beneficial effect of ERAS on reduction of postoperative hospital stay in patients who underwent PD is not attenuated by the increased risk of readmission. They further indicate that expedient discharge of patients who experienced severe postoperative complications may lead to a higher rate of readmission.
PD is a complex procedure that has been associated with prolonged postoperative hospital stays compared with other gastrointestinal operations. Hospital stay after PD is determined by various factors, including patient comorbidities, postoperative complications, hospital volumes, and the healthcare system. Postoperative hospital stay after PD documented in several studies ranged from 13 to 41 days [16] with longer durations in Asia than in Western countries. A recent comparative study of German and Dutch audits showed that hospital stay and readmission were different between the 2 countries, despite no distinction in mortality rate or pancreas-specific complications. An analysis of the United States Nationwide Inpatient Sample data showed that nonprivate insurance status was associated with prolonged hospital stay. These findings indicate that the disparity in healthcare or insurance systems in each country may contribute to varied outcomes of hospital stay in actual clinical practice. Despite the above, most studies from both Western and Asian countries demonstrated that ERAS had contributed to reduction in hospital stay after PD without compromising surgical outcomes. In this study, the mean duration of postoperative stay under the conventional postoperative program was approximately 25 days, which was much longer than that seen in the Western countries. However, implementation of ERAS effectively reduced postoperative hospital stay by 7 days. These findings suggest that the impact of ERAS on hospital stay is universal, and is not specific for a particular healthcare system. It is presumed that preoperative counseling and standardized postoperative care based on established discharge criteria contributed to reduction in the postoperative hospital stay.
Despite the advantage of the ERAS program in reducing the hospital stay, its effect on postoperative complications is controversial in the field of pancreatic surgery. Although the ERAS programs are intended to reduce postoperative complications and promote recovery in patients, the results of this study revealed that implementation was not associated with reduction of severe postoperative complications including CR-POPF. Nonetheless, the ERAS program effectively reduced the hospital stay even in patients who experienced severe complications. These findings suggest that ERAS programs for high-risk procedures may have limitations in reducing postoperative complications but standardized perioperative care as per ERAS protocols may be helpful in promoting recovery from and preventing the progression of complications. No bowel preparation before surgery and early oral intake after surgery could possibly promote recovery of gastrointestinal function, protect the mucosal barrier, and reduce the incidence of complications such as delayed gastric emptying and sepsis. In this study, the ERAS program reduced the incidence of delayed gastric emptying with a minor significance. Early drain removal might have mitigated POPF-associated complications and shortened hospital stay by avoiding prolonged drain insertions as demonstrated in previous studies [17], although it was not associated with reduction in POPF rate in this study.
One of major concerns regarding implementation of ERAS in high-risk procedures including hepatobiliary and pancreatic surgery is that early discharge may lead to increased readmission. In our study, the 90-day readmission rate after PD was 8.8%, which is lower than our Western counterparts who reported a 19%–42% incidence [181920]. This was probably because longer hospital stays in Korea potentially allowed more time for healing in patients and reduced the risk of readmission. In contrast to other studies [21], our results demonstrated that a decreased postoperative hospital stay under the ERAS program was not associated with an increased readmission rate. Multivariate logistic regression analysis revealed that severe postoperative complications and DM were independent risk factors for readmission, while preoperative jaundice was a negative predictive factor. Among those risk factors, severe postoperative complication was the strongest predictor of readmission, which is similar to the findings of past studies [22]. There are some controversies about the relationship between postoperative hospital stay and readmission. Reddy et al. [23] reported longer postoperative length of stay (≥10 days) as a risk factor for readmission, while contrastingly Valero et al. [21] showed that a shorter length of stay (≤10 days) had higher risk of readmission. In this study, late discharge (>POD 14) in patients with no or minor complications did not increase the readmission rate. However, the readmission rate of patients with severe complications after early discharge (≤POD 14) was approximately 43%, which was significantly higher than that (12%) after late discharge. These findings emphasize that discharge planning in patients who had experienced severe postoperative complications requires careful consideration. The risk of potential readmission should be informed to patients and their families before discharge.
POPF-associated complications such as intra-abdominal abscess and bleeding were the main causes for readmission followed by wound infection and delayed gastric emptying. These findings were similar to the results of previous studies [181924]. A unique finding of this study was that POPF-associated complications such as abscesses or bleeding were recurring reasons for readmission, after implementation of ERAS. Therefore, it should be noted that incompletely managed POPF during the index admission or delayed POPF may cause severe complications requiring readmission, especially bleeding which could lead to fatality even after discharge.
This study has several limitations. First, the retrospective nature and long study period of this study cannot exclude the possibility that factors other than ERAS program might have affected postoperative recovery. During the study period, perioperative outcomes such as operative time and intraoperative blood loss significantly decreased after implementation of ERAS program. This suggests that advances in surgical technique with accumulation of experiences, rather than ERAS program possibly contributed to reduction in postoperative hospital stay. However, improvement of surgical techniques did not reduce severe postoperative complications, and the ERAS program shortened postoperative hospital stay even in such patients. In addition, segmented regression analysis of interrupted time series data to minimize the bias of the chronologic effect revealed that the ERAS protocol had an effect on reducing postoperative hospital stay in addition to the chronologic effect. ERAS also had a significantly negative effect on prolonged hospital stay in the multivariate analysis. These findings may indicate that contribution of the ERAS program was higher than other factors in reducing the postoperative hospital stay. Second, this study applied only a limited number of items among the ERAS guidelines for PD which was proposed by the ERAS Society. Use of different protocols may lead to heterogeneous results regarding the effect of ERAS on postoperative outcomes. Nonetheless, it seems that standardization of perioperative care that is suitable for each institution is more important than the contents of the program because of weak evidence. Third, it is possible that readmission rate in this study was underrepresented as we did not trace nonindex institutional readmissions. However, considering that Korea is a small country with relatively easy access to tertiary centers and that patients generally prefer to be readmitted in their index hospital, it is likely that this number was not high. Recently, a randomized controlled trial from a Korean highvolume center was published, showing the noninferiority of ERAS compared to conventional protocol [25]. The limitations of this study were that it was a single-center study which included only a small number of patients. To overcome limitations such as those mentioned above and evaluate the role of ERAS program in the management of patients with PD in the Korean medical environment, multicenter prospective studies are needed.
In conclusion, this study confirms the usefulness of ERAS program for PD in the Korean medical environment similar to reports in Western literature. ERAS program could effectively reduce postoperative hospital stay without increasing the risk of readmission. However, as severe complications were the most potent risk factor for readmission, proper discharge planning and medical support after discharge should be considered in patients who experience severe complications.
References
1. Grobmyer SR, Pieracci FM, Allen PJ, Brennan MF, Jaques DP. Defining morbidity after pancreaticoduodenectomy: use of a prospective complication grading system. J Am Coll Surg. 2007; 204:356–364. PMID: 17324768.

2. Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 2000; 232:786–795. PMID: 11088073.

3. Varadhan KK, Neal KR, Dejong CH, Fearon KC, Ljungqvist O, Lobo DN. The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr. 2010; 29:434–440. PMID: 20116145.

4. Teeuwen PH, Bleichrodt RP, Strik C, Groenewoud JJ, Brinkert W, van Laarhoven CJ, et al. Enhanced recovery after surgery (ERAS) versus conventional postoperative care in colorectal surgery. J Gastrointest Surg. 2010; 14:88–95. PMID: 19779947.

5. Lassen K, Coolsen MM, Slim K, Carli F, de Aguilar-Nascimento JE, Schäfer M, et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin Nutr. 2012; 31:817–830. PMID: 23079762.

6. Takagi K, Yoshida R, Yagi T, Umeda Y, Nobuoka D, Kuise T, et al. Effect of an enhanced recovery after surgery protocol in pat ients undergoing pancreaticoduodenectomy: a randomized controlled trial. Clin Nutr. 2019; 38:174–181. PMID: 29373148.
7. Pearson SD, Kleefield SF, Soukop JR, Cook EF, Lee TH. Critical pathways intervention to reduce length of hospital stay. Am J Med. 2001; 110:175–180. PMID: 11182102.

8. Porter GA, Pisters PW, Mansyur C, Bisanz A, Reyna K, Stanford P, et al. Cost and utilization impact of a clinical pathway for pat ients undergoing pancreaticoduodenectomy. Ann Surg Oncol. 2000; 7:484–489. PMID: 10947015.
9. Vanounou T, Pratt W, Fischer JE, Vollmer CM Jr, Callery MP. Deviation-based cost modeling: a novel model to evaluate the clinical and economic impact of clinical pathways. J Am Coll Surg. 2007; 204:570–579. PMID: 17382215.

10. Montiel Casado MC, Pardo Sánchez F, Rotellar Sastre F, Martí Cruchaga P, Alvarez Cienfuegos FJ. [Experience of a cephalic pancreatoduodenectomy fast-track program]. Cir Esp. 2010; 87:378–384. Spanish. PMID: 20462572.

11. Brown EG, Yang A, Canter RJ, Bold RJ. Outcomes of pancreaticoduodenectomy: where should we focus our efforts on improving outcomes. JAMA Surg. 2014; 149:694–699. PMID: 24849180.
12. Schneider EB, Hyder O, Wolfgang CL, Hirose K, Choti MA, Makary MA, et al. Patient readmission and mortality after surgery for hepato-pancreatobiliary malignancies. J Am Coll Surg. 2012; 215:607–615. PMID: 22921328.

13. Hicks CW, Tosoian JJ, Craig-Schapiro R, Valero V 3rd, Cameron JL, Eckhauser FE, et al. Early hospital readmission for gastrointestinal-related complications predicts long-term mortality after pancreatectomy. Am J Surg. 2015; 210:636–642. PMID: 26384793.

14. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017; 161:584–591. PMID: 28040257.
15. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007; 142:761–768. PMID: 17981197.

16. Schneider EB, Hyder O, Wolfgang CL, Dodson RM, Haider AH, Herman JM, et al. Provider versus patient factors impacting hospital length of stay after pancreaticoduodenectomy. Surgery. 2013; 154:152–161. PMID: 23889945.

17. Van Buren G 2nd, Bloomston M, Hughes SJ, Winter J, Behrman SW, Zyromski NJ, et al. A randomized prospective multicenter trial of pancreaticoduodenectomy with and without routine intraperitoneal drainage. Ann Surg. 2014; 259:605–612. PMID: 24374513.

18. Grewal SS, McClaine RJ, Schmulewitz N, Alzahrani MA, Hanseman DJ, Sussman JJ, et al. Factors associated with recidivism following pancreaticoduodenectomy. HPB (Oxford). 2011; 13:869–875. PMID: 22081922.

19. Ahmad SA, Edwards MJ, Sutton JM, Grewal SS, Hanseman DJ, Maithel SK, et al. Factors influencing readmission after pancreaticoduodenectomy: a multi-institutional study of 1,302 patients. Ann Surg. 2012; 256:529–537. PMID: 22868373.
20. Yermilov I, Bentrem D, Sekeris E, Jain S, Maggard MA, Ko CY, et al. Readmissions following pancreaticoduodenectomy for pancreas cancer: a population-based appraisal. Ann Surg Oncol. 2009; 16:554–561. PMID: 19002528.

21. Valero V 3rd, Grimm JC, Kilic A, Lewis RL, Tosoian JJ, He J, et al. A novel risk scoring system reliably predicts readmission after pancreatectomy. J Am Coll Surg. 2015; 220:701–713. PMID: 25797757.

22. Fisher AV, Fernandes-Taylor S, Campbell-Flohr SA, Clarkson SJ, Winslow ER, Abbott DE, et al. 30-day readmission after pancreatic resection: a systematic review of the literature and meta-analysis. Ann Surg. 2017; 266:242–250. PMID: 28323675.
23. Reddy DM, Townsend CM Jr, Kuo YF, Freeman JL, Goodwin JS, Riall TS. Readmission after pancreatectomy for pancreatic cancer in Medicare patients. J Gastrointest Surg. 2009; 13:1963–1974. PMID: 19760307.

24. Fong ZV, Ferrone CR, Thayer SP, Wargo JA, Sahora K, Seefeld KJ, et al. Understanding hospital readmissions after pancreaticoduodenectomy: can we prevent them?: a 10-year contemporary experience with 1,173 patients at the Massachusetts General Hospital. J Gastrointest Surg. 2014; 18:137–144. PMID: 24002770.
25. Hwang DW, Kim HJ, Lee JH, Song KB, Kim MH, Lee SK, et al. Effect of Enhanced Recovery After Surgery program on pancreaticoduodenectomy: a randomized controlled trial. J Hepatobiliary Pancreat Sci. 2019; 26:360–369. PMID: 31152686.

Fig. 1
(A) Temporal change of postoperative hospital stay (PHS) and readmission rate. (B) Comparison of the changes in trends of PHS before and after Enhanced Recovery After Surgery (ERAS).
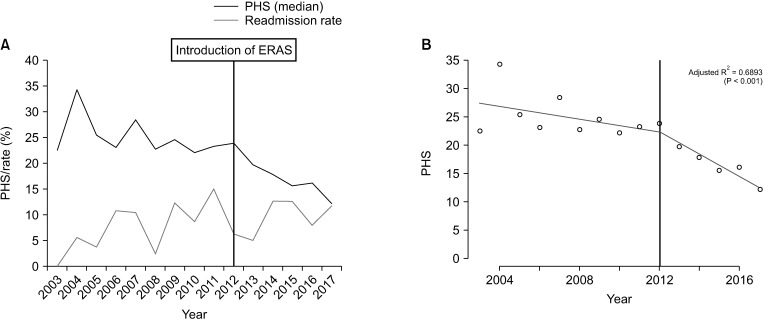
Table 1
Details of Enhanced Recovery After Surgery (ERAS) protocol and conventional protocol after pancreaticoduodenectomy
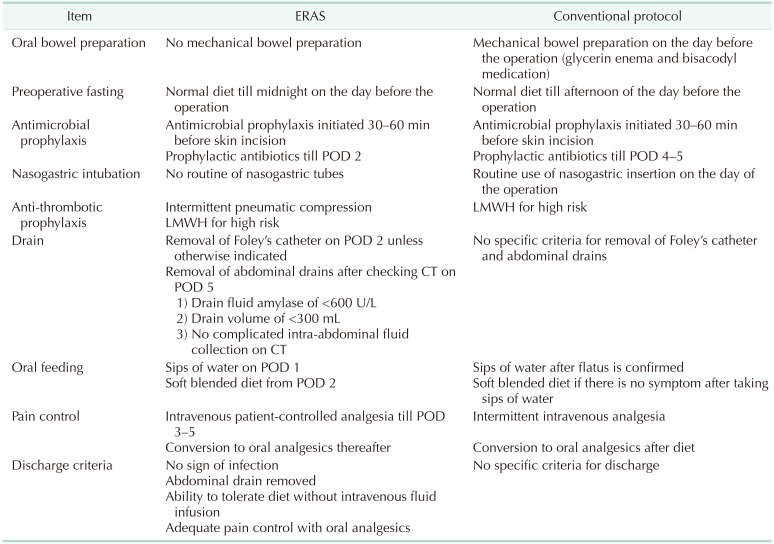
Table 4
Reasons for 90-day readmission and outcomes after readmission
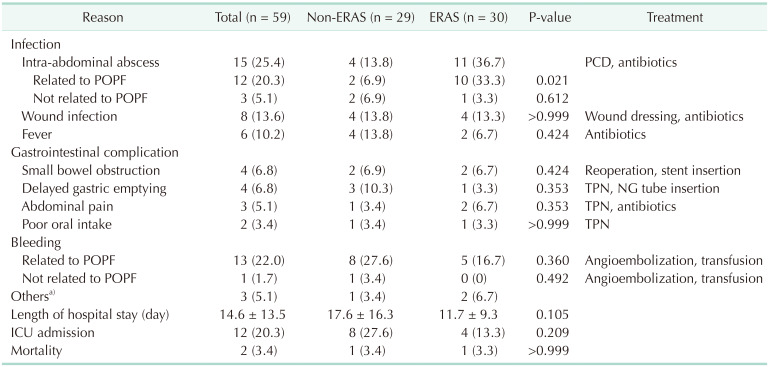
Values are presented as number (%) or mean ± standard deviation.
ERAS, Enhanced Recovery After Surgery; PCD, percutaneous tube drain; POPF, postoperative pancreatic fistula; TPN, total parenteral nutrition; NG, nasogastric tube; ICU, intensive care unit.
a)Others including the following: chylous ascites, portal vein thrombosis, and bile reflux gastritis.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download