1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424. PMID:
30207593.

2. Hundahl SA, Phillips JL, Menck HR. The National Cancer Data Base Report on poor survival of U.S. gastric carcinoma patients treated with gastrectomy: Fifth Edition American Joint Committee on Cancer staging, proximal disease, and the “different disease” hypothesis. Cancer. 2000; 88:921–932. PMID:
10679663.
3. Feng F, Tian Y, Xu G, Liu Z, Liu S, Zheng G, et al. Diagnostic and prognostic value of CEA, CA19-9, AFP and CA125 for early gastric cancer. BMC Cancer. 2017; 17:737. PMID:
29121872.

4. Tian SB, Yu JC, Kang WM, Ma ZQ, Ye X, Cao ZJ, et al. Combined detection of CEA, CA 19-9, CA 242 and CA 50 in the diagnosis and prognosis of resectable gastric cancer. Asian Pac J Cancer Prev. 2014; 15:6295–6300. PMID:
25124614.

5. Mellor KL, Powell AG, Lewis WG. Systematic review and meta-analysis of the prognostic significance of Neutrophil-Lymphocyte Rat io (NLR) af ter R0 gastrectomy for cancer. J Gastrointest Cancer. 2018; 49:237–244. PMID:
29949048.
6. Kim JH, Han DS, Bang HY, Kim PS, Lee KY. Preoperative neutrophil-to-lymphocyte ratio is a prognostic factor for overall survival in patients with gastric cancer. Ann Surg Treat Res. 2015; 89:81–86. PMID:
26236697.

7. Xu Z, Xu W, Cheng H, Shen W, Ying J, Cheng F, et al. The prognostic role of the platelet-lymphocytes ratio in gastric cancer: a meta-analysis. PLoS One. 2016; 11:e0163719. PMID:
27684077.

8. Tanaka H, Tamura T, Toyokawa T, Muguruma K, Kubo N, Sakurai K, et al. C-reactive protein elevation ratio as an early predictor of postoperative severe complications after laparoscopic gastrectomy for gastric cancer: a retrospective study. BMC Surg. 2019; 19:114. PMID:
31429742.

9. Xu BB, Lu J, Zheng ZF, Xie JW, Wang JB, Lin JX, et al. The predictive value of the preoperative C-reactive proteinalbumin ratio for early recurrence and chemotherapy benefit in patients with gastric cancer after radical gastrectomy: using randomized phase III trial data. Gastric Cancer. 2019; 22:1016–1028. PMID:
30739259.

10. Ranzani OT, Zampieri FG, Forte DN, Azevedo LC, Park M. C-reactive protein/ albumin ratio predicts 90-day mortality of septic patients. PLoS One. 2013; 8:e59321. PMID:
23555017.
11. YXMLLink_XYZlmaz EM, Kandemir A. Significance of red blood cell distribution width and C-reactive protein/albumin levels in predicting prognosis of acute pancreatitis. Ulus Travma Acil Cerrahi Derg. 2018; 24:528–531. PMID:
30516251.
12. Wu J, Tan W, Chen L, Huang Z, Mai S. Clinicopathologic and prognostic significance of C-reactive protein/albumin ratio in patients with solid tumors: an updated systemic review and metaanalysis. Oncotarget. 2018; 9:13934–13947. PMID:
29568406.

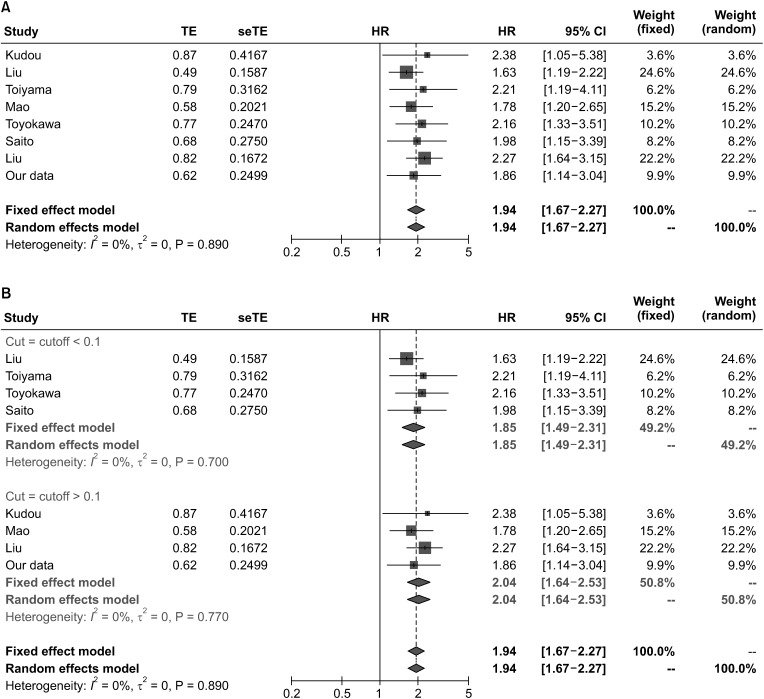
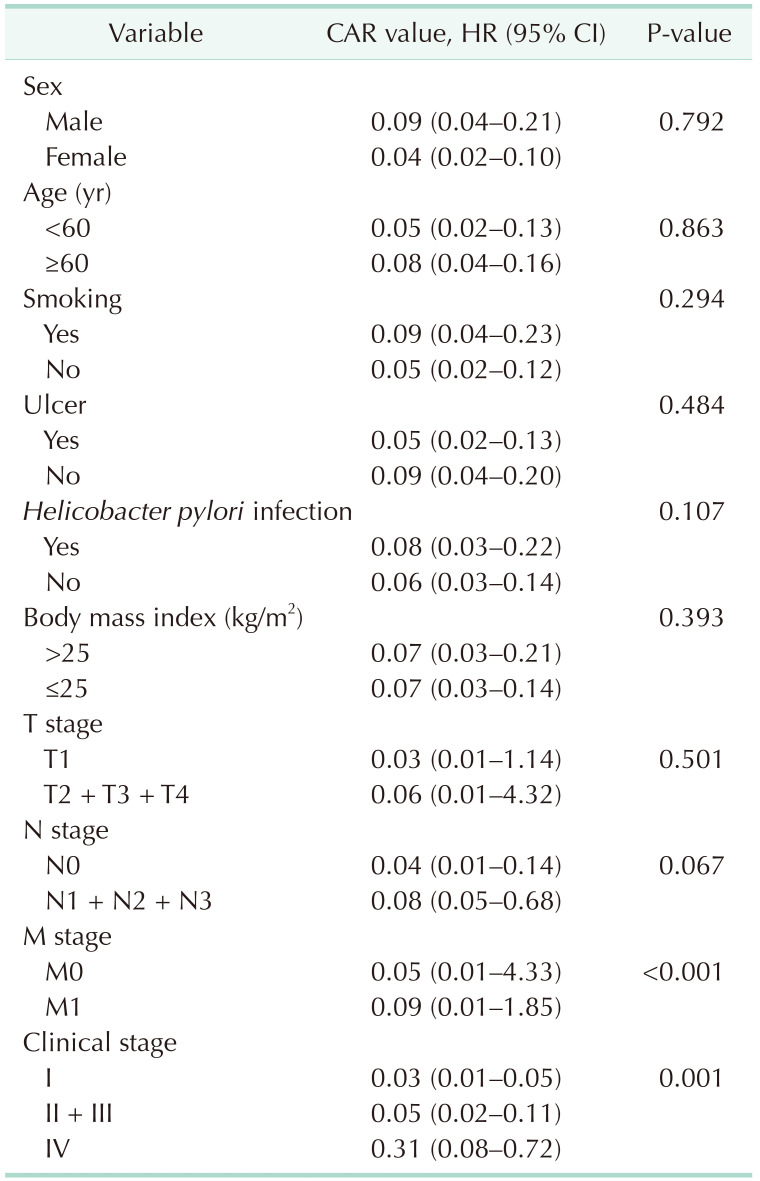
13. Mao M, Wei X, Sheng H, Chi P, Liu Y, Huang X, et al. C-reactive protein/albumin and neutrophil/lymphocyte ratios and their combination predict overall survival in patients with gastric cancer. Oncol Lett. 2017; 14:7417–7424. PMID:
29344182.

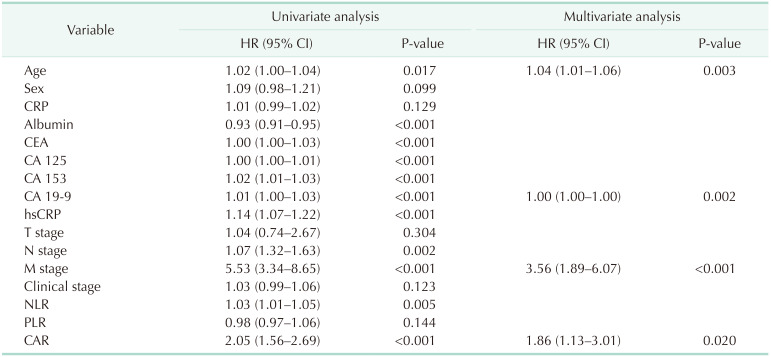
14. Saito H, Kono Y, Murakami Y, Shishido Y, Kuroda H, Matsunaga T, et al. Prognostic significance of the preoperative ratio of C-Reactive protein to albumin and neutrophil-lymphocyte ratio in gastric cancer patients. World J Surg. 2018; 42:1819–1825. PMID:
29270656.

15. Toiyama Y, Shimura T, Yasuda H, Fujikawa H, Okita Y, Kobayashi M, et al. Clinical burden of C-reactive protein/albumin ratio before curative surgery for patients with gastric cancer. Anticancer Res. 2016; 36:6491–6498. PMID:
27919972.

16. Amin MB, Edge SB, Greene F, Byrd DR, Brookland RK, Washington MK, et al. AJCC Cancer Staging Manual. 8th ed. Cham, Switzerland: Springer;2017.
17. Fu YJ, Li KZ, Bai JH, Liang ZQ. C-reactive protein/albumin ratio is a prognostic indicator in Asians with pancreatic cancers: a meta-analysis. Medicine (Baltimore). 2019; 98:e18219. PMID:
31770284.
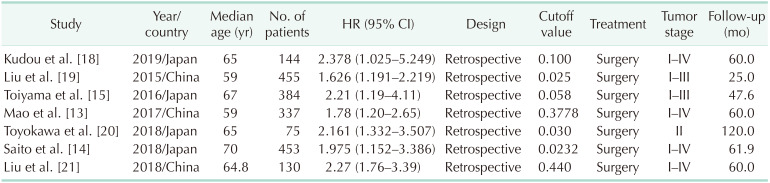
18. Kudou K, Saeki H, Nakashima Y, Kamori T, Kawazoe T, Haruta Y, et al. C-reactive protein/albumin ratio is a poor prognostic factor of esophagogastric junction and upper gastric cancer. J Gastroenterol Hepatol. 2019; 34:355–363. PMID:
30119141.

19. Liu X, Sun X, Liu J, Kong P, Chen S, Zhan Y, et al. Preoperative C-reactive protein/ albumin ratio predicts prognosis of patients after curative resection for gastric cancer. Transl Oncol. 2015; 8:339–345. PMID:
26310380.
20. Toyokawa T, Muguruma K, Tamura T, Sakurai K, Amano R, Kubo N, et al. Comparison of the prognostic impact and combination of preoperative inflammation-based and/or nutritional markers in patients with stage II gastric cancer. Oncotarget. 2018; 9:29351–29364. PMID:
30034622.

21. Liu HC, Chen YJ, Xu YF, Xu ZH, Xu CY. Effect of preoperative ratio of C reactive protein to albumin on prognosis of patients with gastric cancer. Chin J Lab Diagn. 2018; 22:27–29.
22. Abdi E, Latifi-Navid S, Zahri S, Yazdanbod A, Pourfarzi F. Risk factors predisposing to cardia gastric adenocarcinoma: insights and new perspectives. Cancer Med. 2019; 8:6114–6126. PMID:
31448582.

23. Liu Y, Chen S, Zheng C, Ding M, Zhang L, Wang L, et al. The prognostic value of the preoperative c-reactive protein/albumin ratio in ovarian cancer. BMC Cancer. 2017; 17:285. PMID:
28431566.

24. Uchimoto T, Komura K, Fujiwara Y, Saito K, Tanda N, Matsunaga T, et al. Prognostic impact of C-reactive protein-albumin ratio for the lethality in castration-resistant prostate cancer. Med Oncol. 2019; 37:9. PMID:
31754918.

25. Khedher S, Fouthaili N, Maoui A, Lahiani S, Salem M, Bouzid K. The diagnostic and prognostic values of C-reactive protein and procalcitonin during bacterial infections in decompensated cirrhosis. Gastroenterol Res Pract. 2018; 2018:5915947. PMID:
31582968.

26. Chen IM, Johansen AZ, Dehlendorff C, Jensen BV, Bojesen SE, Pfeiffer P, et al. Prognostic value of combined detection of serum IL6, YKL-40, and C-reactive protein in patients with unresectable pancreatic cancer. Cancer Epidemiol Biomarkers Prev. 2020; 29:176–184. PMID:
31685562.

27. Lee SH, Kim KH, Choi CW, Kim SJ, Kim DH, Choi CI, et al. Reduction rate of C-reactive protein as an early predictor of postoperative complications and a reliable discharge indicator after gastrectomy for gastric cancer. Ann Surg Treat Res. 2019; 97:65–73. PMID:
31384611.

28. Takeda K, Umezawa R, Takahashi N, Matsushita H, Kozumi M, Ishikawa Y, et al. Impact of change in serum albumin level during and after chemoradiotherapy in patients with locally advanced esophageal cancer. Esophagus. 2018; 15:190–197. PMID:
29951984.

29. Lim WS, Roh JL, Kim SB, Choi SH, Nam SY, Kim SY. Pretreatment albumin level predicts survival in head and neck squamous cell carcinoma. Laryngoscope. 2017; 127:E437–E442. PMID:
28561532.

30. Dupré A, Malik HZ. Inf lammation and cancer: what a surgical oncologist should know. Eur J Surg Oncol. 2018; 44:566–570. PMID:
29530345.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download