Abstract
Purpose
Primary repair is the standard surgical method for treating duodenal ulcer perforations, with very good results usually anticipated because of the simplicity of the associated surgical techniques. Therefore, this study aimed to analyze the risk factors that affect laparoscopic primary repair outcomes for duodenal ulcer perforation.
Methods
Between June 2010 and June 2020, 124 patients who underwent laparoscopic primary repair for duodenal ulcer perforations were reviewed. Early surgical outcomes were evaluated and risk factors for postoperative complications were assessed.
Results
All surgeries were performed laparoscopically without open conversion. Multivariate analysis showed that the elderly (over 70 years), and perforations that needed more than 2 stitches for closure were risk factors for overall postoperative complications. Perforations that needed more than 2 stitches and perforations on the superior side of the duodenum were major risk factors for severe postoperative complications. Severe postoperative complications occurred in 6 of the patients, and 1 of them died of multiorgan failure.
Conclusion
Based on our results, we suggest that laparoscopic primary repair can be safely performed in duodenal ulcer perforation. However, more careful surgery and postoperative care are needed to improve the surgical outcomes of patients who need more than 2 stitches to close their perforation or who have perforations on the superior side of the duodenum.
The incidence of peptic ulcers decreases each year, but 2%–14% of ulcer patients develop perforations due to ulcers [1]. Peptic ulcer perforations are associated with mortality rates that range from 10% to 30% [2], with a previous report finding that duodenal ulcer perforation results in postoperative mortality rates of 2.7%–13.8% [3].
In practice, several surgical methods are recommended depending on the size of the duodenal ulcer perforation [4]. According to the Sabiston textbook [4], primary repair with omentopexy is recommended when the size of the perforation is less than 1 cm. It is also reported that primary repair can be performed through laparoscopic surgery. Some studies indicate that laparoscopic surgery results in shorter operating time, less postoperative pain, and faster recovery compared to open surgery [56]. Therefore, most clinical physicians prefer to perform laparoscopic primary repair as an emergency surgical method for treating duodenal ulcer perforations.
There are several known risk factors for postoperative complications of peptic ulcer perforation treatment [789]. In particular, there is controversy over applying laparoscopic surgery as the procedure of choice for duodenal ulcer perforation [51011121314]. According to a recent meta-analysis, laparoscopic primary repair can be applied in low-risk patients [10].
In actual clinical practice, most emergency surgeries with low severity are performed by inexperienced surgeons who are not experts [15]. For these reasons, it is not easy to apply laparoscopic surgery as a top choice for duodenal ulcer perforation. Especially, laparoscopic surgery requires a long learning period.
Therefore, this study was designed to analyze the risk factors associated with laparoscopic duodenal ulcer perforation surgery by evaluating the surgical outcomes of laparoscopic primary repair performed by a single gastric surgery expert.
We retrospectively reviewed and prospectively collected data for 180 patients who underwent surgery for duodenal ulcer perforations between June 2010 and June 2020 at Hanyang University Guri Hospital. This study enrolled 124 patients who underwent laparoscopic primary repair. All surgeries were performed by a single surgeon who is an expert in laparoscopic gastric surgery [1617]. Laparoscopic primary repair was attempted in all patients, regardless of previous abdominal surgical history.
Forty-eight patients who underwent other types of surgical methods including gastrectomy were excluded from this study. In addition, 8 patients who were forced to undergo only primary repair due to unstable hemodynamic conditions were also excluded from this study. Among patients who had hypotension in the emergency department, patients who returned to normal blood pressure in response to simple fluid therapy were enrolled in this study.
Approval for this study was obtained from the Institutional Review Board of Hanyang University Guri Hospital in Guri, Korea (No. 2020-05-007). The requirement for informed consent was waived because of the retrospective nature of the study.
Three trocars were used for laparoscopic primary repair, and the size of the perforation was measured using surgical suture material. One or more stitches were used to close the perforation site. We did not select the size of perforation as a variable factor, because the size of an ulcer is not proportional to the size of the perforation hole. Instead of the size, we used the number of stitches needed to close the perforation. Black silk (3-0, 26 mm, 75 cm; Mersilk, Ethicon, Sommerville, NJ, USA) was used to close the site. Following closure of the perforation site, peritoneal irrigation was undertaken with a large volume of saline (usually 1- or 2-L) to minimize any infection source. A large mass of omentum was then placed above the primary suture site. We have previously published a paper that detailed these surgical techniques [18].
Primary repair has not been selected as a treatment method in the following cases. First, it is impossible to close the perforation despite multiple stitches due to a large perforation size. The second is when the ulcer tissues are crushed during the primary repair process, resulting in a larger hole.
In this study, shock was defined as a state of low blood pressure (systolic blood pressure below 90 mmHg or a diastolic blood pressure below 60 mmHg) in the emergency room. Laparoscopic surgery has been tried in all patients who were hemodynamically stable. Open surgery was applied in all hemodynamically unstable patients who required inotropic agents.
Clinical data obtained from medical records included patient age, sex, body mass index, history of previous major abdominal surgery, American Society of Anesthesiologists (ASA) physical status (PS) classification, and others. Early surgical outcomes included operation time, postoperative complications, day of commencement of a soft diet, and postoperative hospital stay. The location of the perforation was defined as the superior side when it occurred toward the hepatoduodenal ligament (Fig. 1).
Statistical analyses were performed using IBM SPSS Statistics for Windows ver. 21.0 (IBM Corp., Armonk, NY, USA). All values are expressed as mean ± standard deviation. Categorical variables were assessed with the chi-square test and all continuous variables were assessed using the Student t-test, depending on the data. Multivariate analyses were performed to identify prognostic factors associated with postoperative complications. The Cox proportional hazards model was employed for multivariate regression analysis. Hazard ratios with 95% confidence intervals were estimated for each variable in the multivariate analysis. A P-value of <0.05 was considered statistically significant.
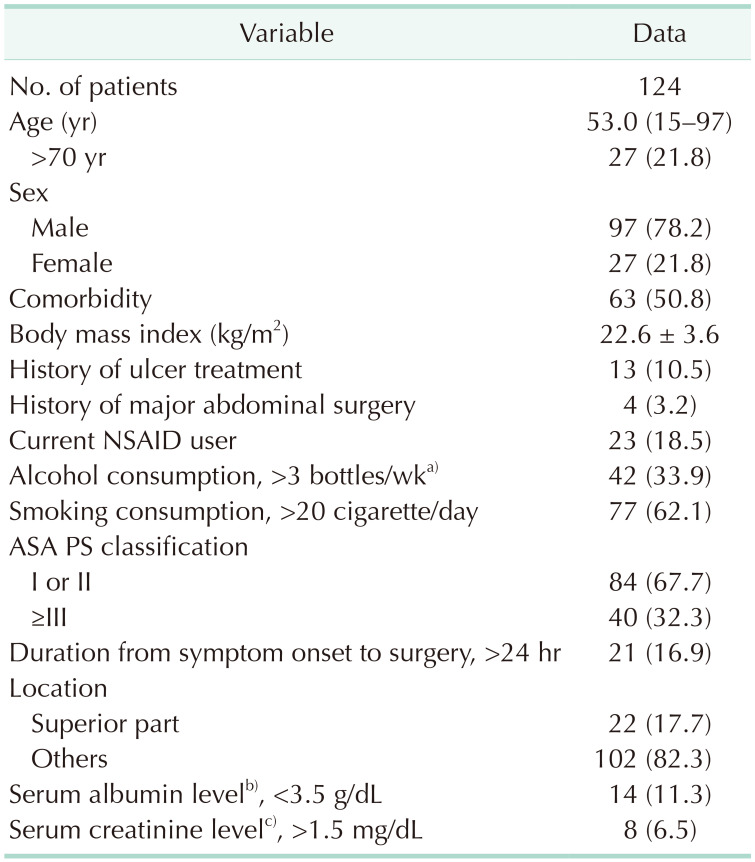
Patient clinical characteristics are presented in Table 1. Median age was 53.0 years and most patients (78.2%) were male. About half of the patients had comorbidities. Thirteen patients (10.5%) had histories of ulcer treatment. Twenty-three patients (18.5%) were taking NSAIDs. Forty-two patients (33.9%) were heavy drinkers, and 77 patients (62.1%) were heavy smokers. Forty patients (32.3%) had an ASA PS classification of 3 or higher. Twenty-one patients (16.9%) arrived at the emergency department 2 days after the onset of symptoms. Twenty-two patients (17.7%) had ulcer perforations on the superior side of the duodenum. Fourteen patients (11.3%) showed hypoalbuminemia and 8 patients (6.5%) had an elevated creatinine level (over 1.5 mg/dL).
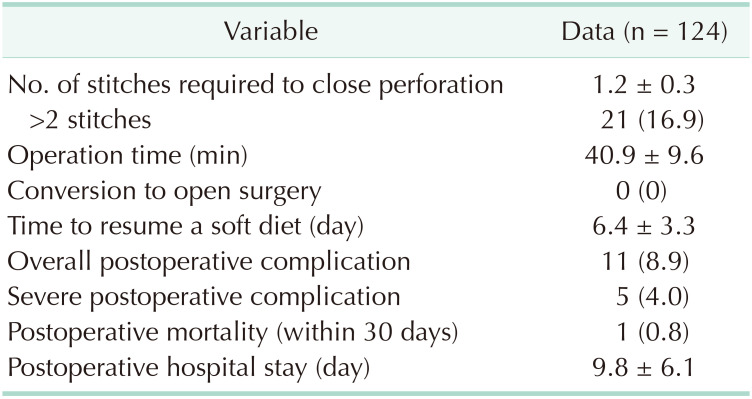
One stitch was sufficient to close the perforation site in all patients except for 21 patients. The mean operation time was 40.9 minutes. There were no cases of conversion to open surgery. Postoperative complications occurred in 11 patients (8.9%). Eight of 11 patients had severe postoperative complications. One patient died within 1 month after surgery (Table 2).
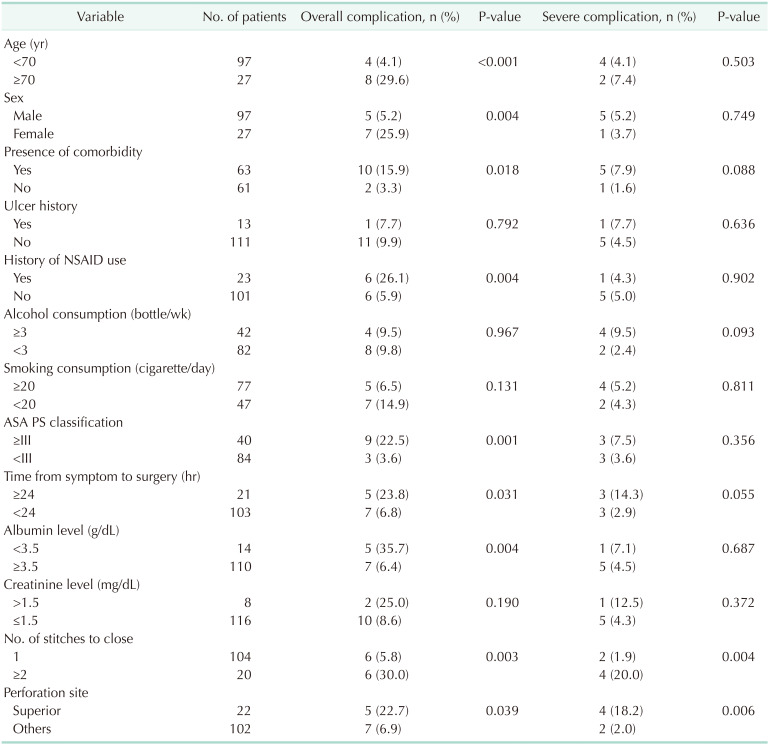
Table 3 lists the risk factors for early surgical outcomes. A statistically significant postoperative complication rate was observed in patients who were elderly, females, patients with comorbidities, NSAIDs users, patients with high ASA PS classification, delayed operation times, low albumin levels, over 2 stitches, and superior perforations. The rate of severe postoperative complications was significantly higher in perforations which needed more than 2 stitches, and perforations on the superior side of the duodenum.
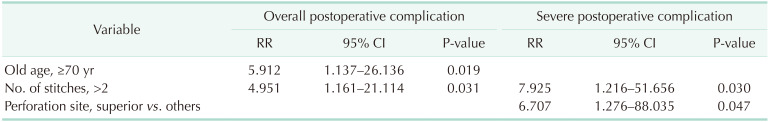
The results of multivariate analysis of complication risk factors are listed in Table 4. Being elderly, and a perforation which needed more than 2 stitches were significant risk factors for overall postoperative complications. Perforations which needed more than 2 stitches and perforations on the superior side of the duodenum were significant risk factors for severe postoperative complications.
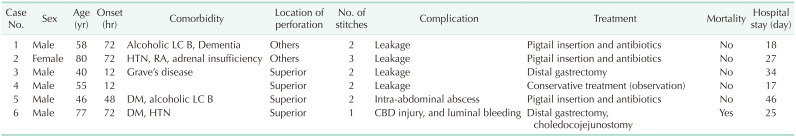
Severe postoperative complications occurred in 6 of all patients (Table 5). Except for one, most of the patients had comorbidities. Two patients who underwent reoperation had comorbidities and their perforation sites were on the superior side of the duodenum. Especially, 1 of them underwent choledocojejunostomy due to common bile duct injury caused by the suturing process. Eventually, he did not recover after reoperation and died of septic shock and multiorgan failure.
Up to now, many papers have been published on surgical methods, surgical outcomes, and risk factors for duodenal ulcer perforation. Based on the evidence of several published reports and the views of surgeons, primary repair is strongly recommended for duodenal ulcer perforations with small perforation size [518].
Combining the results of several studies [2321222324], high ASA PS classification (over 3), elderly status (65 years), large perforation size (over 0.9–1.0 cm), shock on admission, and blood test abnormalities are considered to affect postoperative complications and mortality. Our analyses also showed similar results compared with previous studies.
Our multivariate analysis confirmed that elderly patients (over 70 years old), and perforations which needed more than 2 stitches were significant risk factors for overall postoperative complications. Especially, it was confirmed that perforations which needed more than 2 stitches, and perforations on the superior side of the duodenum were major significant risk factors for severe postoperative complications.
There are some reports that complication rates of primary repair can be increased when perforation size is greater than 1.0–1.5 cm [2425]. Therefore, most surgeons consider primary repair to be a very safe procedure if the size of the perforation is less than 1 cm. In this study, we did not use length of perforation as an objective variable factor. It is very difficult to measure the perforation size laparoscopically in emergency situations. Moreover, the size of a perforation is not proportional to the size of a duodenal ulcer. There was a report that simple closure with or without omental patch is a safe surgical procedure in duodenal ulcer perforations up to 2 cm in size [26]. In practice, we experienced that a perforation larger than 1.0 cm can be closed easily with 1 stitch, or even a perforation smaller than 1.0 cm can be closed by over 2 stitches.
Several authors suggested their perforation cutoff sizes predicted conversion to open surgery [5824]. They proposed a cutoff perforation size of 1 cm. However, we have never experienced conversion to open surgery. Therefore, we are confident that the size of perforation is not related to conversion to open surgery. In practice, most cases of primary repair were performed by trainee surgeons [2728]. On the other hand, our surgeries (more than 100 cases) were performed by a single expert surgeon.
Our study suggests a new risk factor that differs from those of previous studies. It was confirmed that the location of the duodenal perforation could be an important risk factor for severe postoperative complications. From the experiences of 124 laparoscopic primary repair cases, we have found that a perforation on the superior side needs to be closed very carefully. Especially, injury to the common bile duct may occur during the suturing process due to severe adhesion of the perforation site. Therefore, if the perforation occurs on the superior side of the duodenum (Fig. 1), the duodenum including the ulcer should be separated from the hepatoduodenal ligament area to expose the perforation site. After that, the degree of perforation should be re-evaluated and the appropriate surgical method must be selected.
Based on our experiences and analysis of surgical outcomes, we suggest that the primary duodenal ulcer repair method can be safely performed laparoscopically. However, more careful surgical techniques and postoperative care are needed to improve surgical outcomes of patients who need more than 2 stitches to close a perforation or who have a perforation on the superior side of the duodenum.
References
1. Bertleff MJ, Lange JF. Perforated peptic ulcer disease: a review of history and treatment. Dig Surg. 2010; 27:161–169. PMID: 20571260.

2. Møller MH, Shah K, Bendix J, Jensen AG, Zimmermann-Nielsen E, Adamsen S, et al. Risk factors in patients surgically treated for peptic ulcer perforation. Scand J Gastroenterol. 2009; 44:145–152. PMID: 18785067.

3. Boey J, Choi SK, Poon A, Alagaratnam TT. Risk stratification in perforated duodenal ulcers: a prospective validation of predictive factors. Ann Surg. 1987; 205:22–26. PMID: 3800459.
4. Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL. Sabiston textbook of surgery: the biological basis of modern surgical practice. 20th ed. Philadelphia (PA): Elsevier Saunders;2017.
5. Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, et al. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg. 2002; 235:313–319. PMID: 11882751.
6. Bertleff MJ, Halm JA, Bemelman WA, van der Ham AC, van der Harst E, Oei HI, et al. Randomized clinical trial of laparoscopic versus open repair of the perforated peptic ulcer: the LAMA Trial. World J Surg. 2009; 33:1368–1373. PMID: 19430829.

7. Kim MG. Laparoscopic surgery for perforated duodenal ulcer disease: analysis of 70 consecutive cases from a single surgeon. Surg Laparosc Endosc Percutan Tech. 2015; 25:331–336. PMID: 25799260.
8. Lee FY, Leung KL, Lai PB, Lau JW. Selection of patients for laparoscopic repair of perforated peptic ulcer. Br J Surg. 2001; 88:133–136. PMID: 11136326.

9. Lunevicius R, Morkevicius M. Systematic review comparing laparoscopic and open repair for perforated peptic ulcer. Br J Surg. 2005; 92:1195–1207. PMID: 16175515.

10. Lau H. Laparoscopic repair of perforated peptic ulcer: a meta-analysis. Surg Endosc. 2004; 18:1013–1021. PMID: 15136924.

11. Lau WY, Leung KL, Kwong KH, Davey IC, Robertson C, Dawson JJ, et al. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg. 1996; 224:131–138. PMID: 8757375.

12. Matsuda M, Nishiyama M, Hanai T, Saeki S, Watanabe T. Laparoscopic omental patch repair for perforated peptic ulcer. Ann Surg. 1995; 221:236–240. PMID: 7717776.

13. Michelet I, Agresta F. Perforated peptic ulcer: laparoscopic approach. Eur J Surg. 2000; 166:405–408. PMID: 10881954.
14. Siu WT, Chau CH, Law BK, Tang CN, Ha PY, Li MK. Routine use of laparoscopic repair for perforated peptic ulcer. Br J Surg. 2004; 91:481–484. PMID: 15048752.

15. Kim HS, Lee JH, Kim MG. Outcomes of laparoscopic primary gastrectomy with curative intent for gastric perforation: experience from a single surgeon. Surg Endosc;2020. 8. 28. [Epub]. . DOI: 10.1007/s00464-020-07902-z.
16. Lee HH, Son SY, Lee JH, Kim MG, Hur H, Park DJ. Surgeon's experience overrides the effect of hospital volume for postoperative outcomes of laparoscopic surgery in gastric cancer: multi-institutional study. Ann Surg Oncol. 2017; 24:1010–1017. PMID: 27834031.

17. Kim MG, Kim KC, Yook JH, Kim BS, Kim TH, Kim BS. A practical way to overcome the learning period of laparoscopic gastrectomy for gastric cancer. Surg Endosc. 2011; 25:3838–3844. PMID: 21656323.

18. Ma CH, Kim MG. Laparoscopic primary repair with omentopexy for duodenal ulcer perforation: a single institution experience of 21 cases. J Gastric Cancer. 2012; 12:237–242. PMID: 23346496.

19. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.
20. Clavien PA, Strasberg SM. Severity grading of surgical complications. Ann Surg. 2009; 250:197–198. PMID: 19638901.

21. Sharma SS, Mamtani MR, Sharma MS, Kulkarni H. A prospective cohort study of postoperative complications in the management of perforated peptic ulcer. BMC Surg. 2006; 6:8. PMID: 16780583.

22. Hermansson M, Staël von Holstein C, Zilling T. Surgical approach and prognostic factors after peptic ulcer perforation. Eur J Surg. 1999; 165:566–572. PMID: 10433141.
23. Blomgren LG. Perforated peptic ulcer: long-term results after simple closure in the elderly. World J Surg. 1997; 21:412–415. PMID: 9143574.

24. Kim JH, Chin HM, Bae YJ, Jun KH. Risk factors associated with conversion of laparoscopic simple closure in perforated duodenal ulcer. Int J Surg. 2015; 15:40–44. PMID: 25644542.

25. Abd Ellatif ME, Salama AF, Elezaby AF, El-Kaffas HF, Hassan A, Magdy A, et al. Laparoscopic repair of perforated peptic ulcer: patch versus simple closure. Int J Surg. 2013; 11:948–951. PMID: 23806652.

26. Sartelli M, Viale P, Catena F, Ansaloni L, Moore E, Malangoni M, et al. 2013 WSES guidelines for management of intraabdominal infections. World J Emerg Surg. 2013; 8:3. PMID: 23294512.
27. Sauerland S, Agresta F, Bergamaschi R, Borzellino G, Budzynski A, Champault G, et al. Laparoscopy for abdominal emergencies: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc. 2006; 20:14–29. PMID: 16247571.
28. Søreide K, Thorsen K, Søreide JA. Strategies to improve the outcome of emergency surgery for perforated peptic ulcer. Br J Surg. 2014; 101:e51–e64. PMID: 24338777.

Fig. 1
Ulcer perforation on the superior side of the duodenum. (A) Laparoscopic image. (B) Detailed illustration.
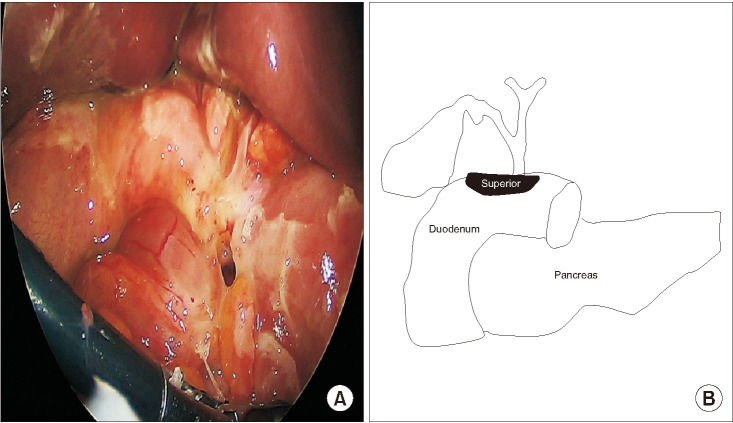
Table 1
Pre- and intraoperative characteristics of patients who underwent laparoscopic primary repair




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download