1. Hartwig W, Gluth A, Hinz U, Bergmann F, Spronk PE, Hackert T, et al. Total pancreatectomy for primary pancreatic neoplasms: renaissance of an unpopular operation. Ann Surg. 2015; 261:537–546. PMID:
24979606.
2. Müller MW, Friess H, Kleeff J, Dahmen R, Wagner M, Hinz U, et al. Is there still a role for total pancreatectomy? Ann Surg. 2007; 246:966–974. PMID:
18043098.

3. Epelboym I, Winner M, DiNorcia J, Lee MK, Lee JA, Schrope B, et al. Quality of life in patients after total pancreatectomy is comparable with quality of life in patients who undergo a partial pancreatic resection. J Surg Res. 2014; 187:189–196. PMID:
24411300.

4. Suzuki S, Kajiyama H, Takemura A, Shimazaki J, Nishida K, Shimoda M. The clinical outcomes after total pancreatectomy. Dig Surg. 2017; 34:142–150. PMID:
27701159.

5. Datta J, Lewis RS Jr, Strasberg SM, Hall BL, Allendorf JD, Beane JD, et al. Quantifying the burden of complications following total pancreatectomy using the postoperative morbidity index: a multiinstitutional perspective. J Gastrointest Surg. 2015; 19:506–515. PMID:
25451733.

6. Zakaria HM, Stauffer JA, Raimondo M, Woodward TA, Wallace MB, Asbun HJ. Total pancreatectomy: short- and long-term outcomes at a high-volume pancreas center. World J Gastrointest Surg. 2016; 8:634–642. PMID:
27721927.

7. Ryska M, Rudis J. Pancreatic fistula and postoperative pancreatitis after pancreatoduodenectomy for pancreatic cancer. Hepatobiliary Surg Nutr. 2014; 3:268–275. PMID:
25392838.
8. Kusakabe J, Anderson B, Liu J, Williams GA, Chapman WC, Doyle MMB, et al. Long-term endocrine and exocrine insufficiency after pancreatectomy. J Gastrointest Surg. 2019; 23:1604–1613. PMID:
30671791.

9. Watanabe Y, Ohtsuka T, Matsunaga T, Kimura H, Tamura K, Ideno N, et al. Longterm outcomes after total pancreatectomy: special reference to survivors' living conditions and quality of life. World J Surg. 2015; 39:1231–1239. PMID:
25582768.

10. Billings BJ, Christein JD, Harmsen WS, Harrington JR, Chari ST, Que FG, et al. Quality-of-life after total pancreatectomy: is it really that bad on long-term follow-up? J Gastrointest Surg. 2005; 9:1059–1066. PMID:
16269376.

11. Pulvirenti A, Pea A, Rezaee N, Gasparini C, Malleo G, Weiss MJ, et al. Perioperative outcomes and long-term quality of life after total pancreatectomy. Br J Surg. 2019; 106:1819–1828. PMID:
31282569.

12. Scholten L, Latenstein AE, van Eijck C, Erdmann J, van der Harst E, Mieog JS, et al. Outcome and long-term quality of life after total pancreatectomy (PANORAMA): a nationwide cohort study. Surgery. 2019; 166:1017–1026. PMID:
31500907.
13. Scholten L, Stoop TF, Del Chiaro M, Busch OR, van Eijck C, Molenaar IQ, et al. Systematic review of functional outcome and quality of life after total pancreatectomy. Br J Surg. 2019; 106:1735–1746. PMID:
31502658.

14. Struyvenberg MR, Fong ZV, Martin CR, Tseng JF, Clancy TE, Fernández-Del Castillo C, et al. Impact of treatments on diabetic control and gastrointestinal symptoms after total pancreatectomy. Pancreas. 2017; 46:1188–1195. PMID:
28902790.

15. Yang DJ, Xiong JJ, Liu XT, Li J, Dhanushka Layanthi Siriwardena KM, Hu WM. Total pancreatectomy compared with pancreaticoduodenectomy: a systematic review and meta-analysis. Cancer Manag Res. 2019; 11:3899–3908. PMID:
31123419.
16. Suzuki S, Miura J, Shimizu K, Tokushige K, Uchigata Y, Yamamoto M. Clinicophysiological outcomes after total pancreatectomy. Scand J Gastroenterol. 2016; 51:1526–1531. PMID:
27461044.

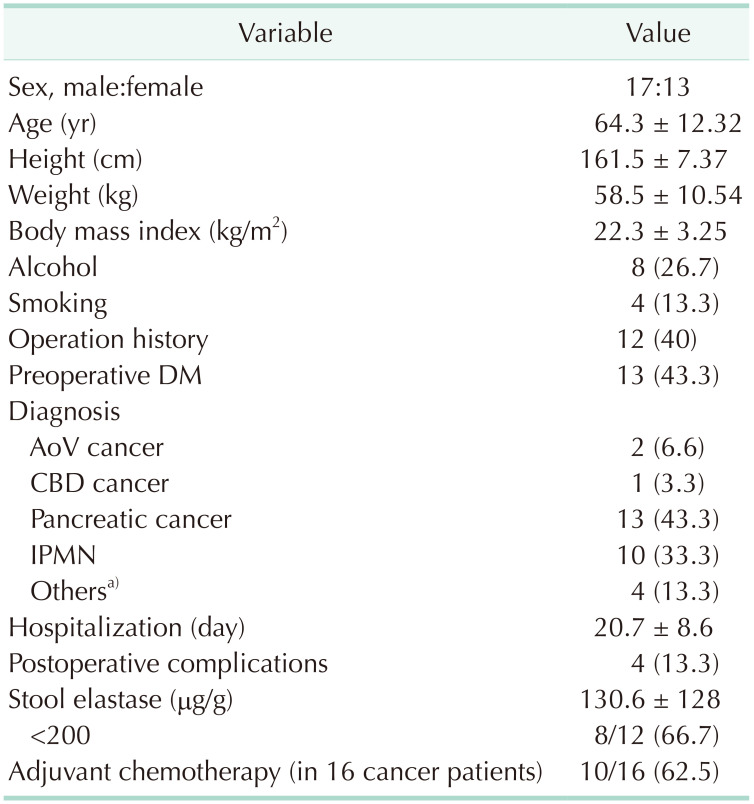
17. Kim H, Yoon YS, Han Y, Kwon W, Kim SW, Han HS, et al. Effects of pancreatic enzyme replacement therapy on body weight and nutritional assessments after pancreatoduodenectomy in a randomized trial. Clin Gastroenterol Hepatol. 2020; 18:926–934. PMID:
31520730.

18. Maker AV, Sheikh R, Bhagia V. Diabetes Cont rol and Compl icat ions Tr ial (DCCT) Research Group. Perioperative management of endocrine insufficiency after total pancreatectomy for neoplasia. Langenbecks Arch Surg. 2017; 402:873–883. PMID:
28733926.

19. Guigoz Y. The Mini Nutritional Assessment (MNA) review of the literature: what does it tell us? J Nutr Health Aging. 2006; 10:466–485. PMID:
17183419.
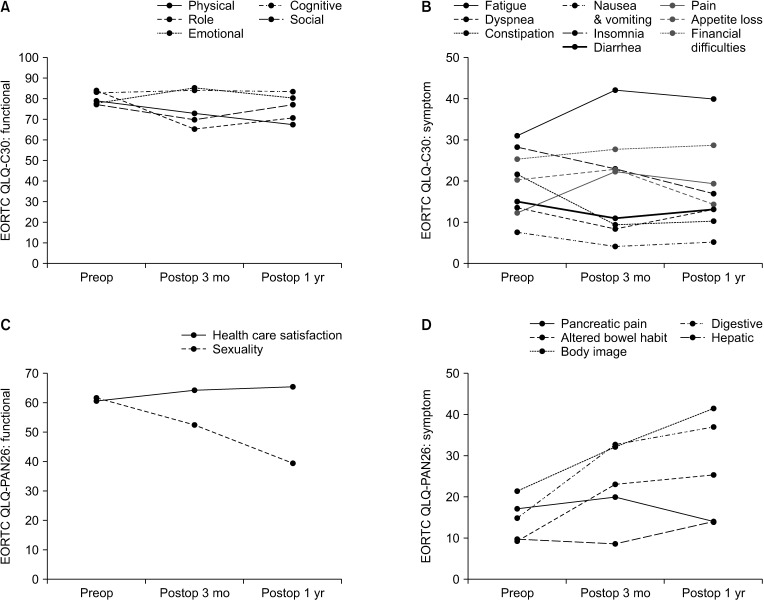
20. Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993; 85:365–376. PMID:
8433390.

21. Fitzsimmons D, Johnson CD, George S, Payne S, Sandberg AA, Bassi C, et al. Development of a disease specific quality of life (QoL) questionnaire module to supplement the EORTC core cancer QoL questionnaire, the QLQ-C30 in patients with pancreatic cancer. EORTC Study Group on Quality of Life. Eur J Cancer. 1999; 35:939–941. PMID:
10533475.
22. Anwar S, Tan W, Yu J, Hutson A, Javle M, Iyer R. Quality-of-life (QoL) as a predictive biomarker in patients with advanced pancreatic cancer (APC) receiving chemotherapy: results from a prospective multicenter phase 2 trial. J Gastrointest Oncol. 2014; 5:433–439. PMID:
25436122.
23. Lis CG, Gupta D, Grutsch JF. Patient satisfaction with quality of life as a predictor of survival in pancreatic cancer. Int J Gastrointest Cancer. 2006; 37:35–44. PMID:
17290079.

24. Stoop TF, Ateeb Z, Ghorbani P, Scholten L, Arnelo U, Besselink MG, et al. Impact of endocrine and exocrine insufficiency on quality of life after total pancreatectomy. Ann Surg Oncol. 2020; 27:587–596. PMID:
31562603.

25. Rijssen LB, Gerritsen A, Henselmans I, Sprangers MA, Jacobs M, Bassi C, et al. Core set of outcomes in pancreatic cancer (COPRAC): an international Delphi study among patients and health care providers. Ann Surg. 2019; 270:158–164. PMID:
29261524.
26. Struyvenberg MR, Martin CR, Freedman SD. Practical guide to exocrine pancreatic insufficiency: breaking the myths. BMC Med. 2017; 15:29. PMID:
28183317.

27. Dresler CM, Fortner JG, McDermott K, Bajorunas DR. Metabolic consequences of (regional) total pancreatectomy. Ann Surg. 1991; 214:131–140. PMID:
1867520.

28. Gilliland TM, Villafane-Ferriol N, Shah KP, Shah RM, Tran Cao HS, Massarweh NN, et al. Nutritional and metabolic derangements in pancreatic cancer and pancreatic resection. Nutrients. 2017; 9:243.

29. Nanashima A, Hiyoshi M, Imamura N, Yano K, Hamada T, Hamada R, et al. Clinical significance of preoperative nutritional parameter and patient outcomes after pancreatectomy: a retrospective study at two academic institute. Ann Hepatobiliary Pancreat Surg. 2019; 23:168–173. PMID:
31225419.

30. Roberts KJ, Blanco G, Webber J, Marudanayagam R, Sutcliffe RP, Muiesan P, et al. How severe is diabetes after total pancreatectomy? A case-matched analysis. HPB (Oxford). 2014; 16:814–821. PMID:
24344937.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download