Abstract
Purpose
Cyst excision with hepaticojejunostomy has been the classic procedure for treating choledochal cysts, and the use of laparoscopic treatment has been favored recently. The purpose of this study was to compare the long-term biliary complication of laparoscopic operation with open surgery for choledochal cyst presenting in children.
Methods
A retrospective study comparing the laparoscopic and open procedures was performed in 185 patients with choledochal cyst in a single children's hospital. There were 109 patients who were operated with open surgery, and 76 patients operated with laparoscopic surgery. The primary outcome was long-term biliary complications and the secondary outcome included operative time, intraoperative transfusion, length of hospital stay, and other late postoperative complications.
Results
In the patient's demographics, there was no significant difference between the 2 groups. Notably, it was shown that the operative time was longer in the laparoscopic group. The number of patients requiring blood transfusion intraoperatively was lower in the laparoscopic group. It was noted that the hospital stay was not statistically different. The duration to resumption of diet and duration of drainage were longer in the laparoscopic group. Biliary complications were shown to be significantly higher in the open group. The risk factor for long-term biliary complications was noted with the intraoperative transfusion.
Go to : 
To begin with, choledochal cysts were found to be a congenital biliary tract anomaly, first described by Vater and Ezler [1] in 1723, and classified by Todani et al. [2] in 1977. In this sense, choledochal cysts occur more frequently in Asians than in Westerners and are known to have higher incidence in women than men [3]. It is often diagnosed in young children, and the main symptoms are abdominal pain, the presence of a palpable mass, and jaundice. This condition has the potential for malignancy transformation and usually requires surgical treatment. In these cases, it is standard to perform a Roux-en-Y hepaticojejunostomy (HJ) after excision of the choledochal cyst completely. Since the first laparoscopy surgery was described in 1995 by Farello et al. [4], its proportion of performing this procedure has been increasing, and most centers currently perform this type of laparoscopic surgery. This paper analyzed the long-term outcome on regards to the previous paper, which was published for the early experience of laparoscopic choledochal cyst excision in 2013 [5]. The purpose of this paper was to compare the long-term biliary complication and also the efficiency and stability of open and laparoscopy surgery with expanded experiences, and to examine any risk factors that could be shown affecting long-term complications.
Go to : 
We analyzed the total of 185 cases by exclusion of open conversion cases during 2 laparoscopies out of 187 cases, in which choledochal cyst was performed at Seoul National University Children's Hospital from October 2004 to September 2017. All data were obtained retrospectively by reviewing the electronic medical records of the patients being reviewed. We have collected data starting from October 2004, because this was the time when the electronic recording system in the center began being used to track patient data. The cases were performed by 2 surgeons, one was a veteran surgeon focusing on open surgery from before 2004 to 2013, and the other was a surgeon who started laparoscopic choledochal cyst surgery at our hospital in 2011.
Variables of interest included the patient's sex, the age at the time of operation, body weight, Todani's type, cyst size, preoperative presence of choledocholithiasis, presence of anomalous pancreaticobiliary duct union (APBDU), clinical manifestations, preoperative laboratory findings, presence of preoperative cholangitis and pancreatitis, operation time, presence of intraoperative transfusion, the periods of hospital stay, resumption of diet, duration of drainage, and the presence or experience of any postoperative complications.
Cholangitis was defined as when the levels of preoperative total bilirubin, AST, and ALT were noted above the normal range, with the symptoms of Charcot triad [6]. The condition of pancreatitis was defined as when the preoperative serum amylase or lipase level increased more than 3 times the normal upper limit when measured.
In the study, the variable and the differences according to type of operation were tested by a chi-square test or Fisher exact test, or by an analysis of variance. In addition, a multivariate analysis using a logistic regression was performed to identify factors affecting late biliary complications. The P-value of <0.05 was considered as a significant result in all results, and we used IBM SPSS Statistics ver. 25.0 (IBM Corp., Armonk, NY, USA).
The study has been approved by the Institutional Review Board of Seoul National University Hospital (No. 1909-100-1066). Written informed consent was waived due to its retrospective nature.
Go to : 
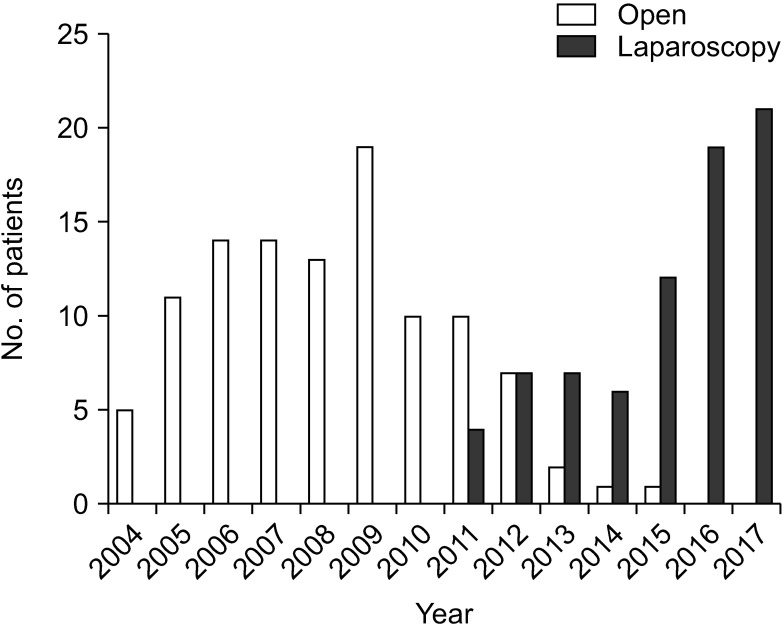
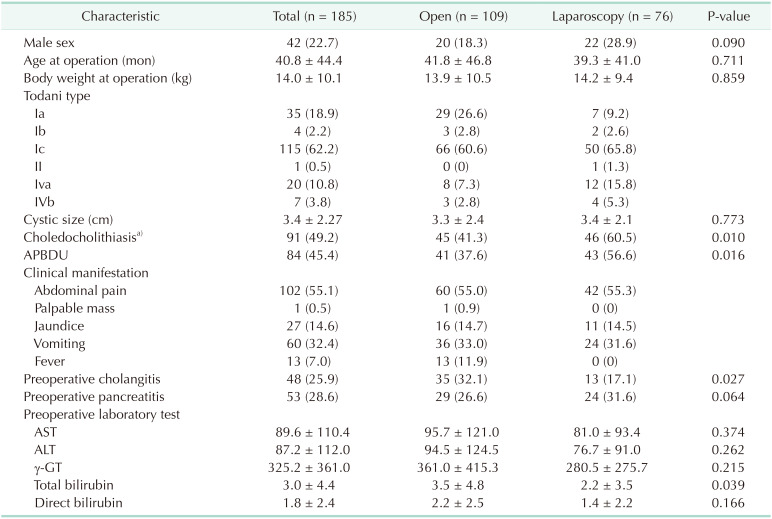
At initiation, among the 185 patients, there were 76 patients who underwent laparoscopic surgery. Looking at the yearly incidence of open and laparoscopy surgery from 2004 to 2017, the number of laparoscopy surgeries has increased significantly since 2011 (Fig. 1). The mean age of patients who underwent surgery was 40.8 months at the time of operation, and there was no significant difference between the 2 groups (41.8 vs. 39.3 months) (Table 1). Likewise, the mean body weight at the time of operation was 14.0 kg (13.9 vs. 14.2 kg), and there were no significant differences between the 2 groups at the Todani type, cystic duct size, the presence of choledocholithiasis, and APBDU. Broadly speaking, at the clinical manifestation, 102 patients presented with abdominal pain, 60 with vomiting, 27 with jaundice, and 13 with a fever. Additionally, 48 patients presented the symptoms of cholangitis at the time of admission and 53 patients had pancreatitis at that time.
The mean preoperative laboratory results were as follows (Table 1): total bilirubin, 3.0 mg/dL (0.2–18.8 mg/dL); AST, 89.6 IU/L (7–683 IU/L); ALT, 87.2 IU/L (3–492 IU/L). There were also no significant differences noted between the 2 groups in the above-mentioned categories.
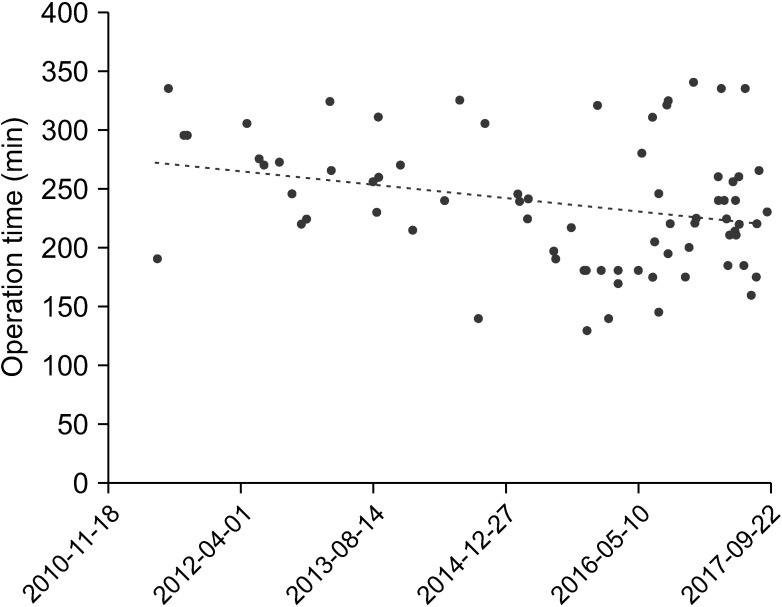
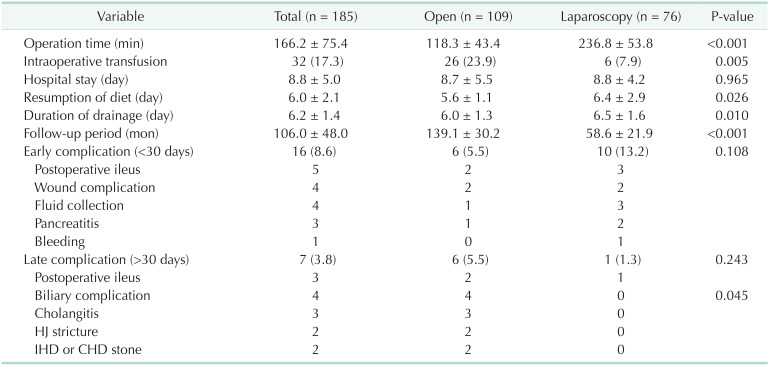
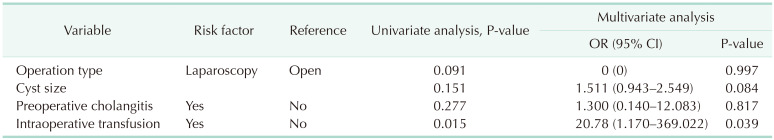
In this case, the mean operation time was 166.2 minutes (70–340 minutes) (Table 2). Open surgery was 118.3 minutes and laparoscopic surgery was noted as being longer as compared to open, at 236.8 minutes. When the operation time of laparoscopy surgery was analyzed, it tended to decrease (Fig. 2). The number of patients who needed to have intraoperative transfusion is higher in the open group (26 vs. 6). The length of hospital stay was similar between the 2 groups at 8.7 days and 8.8 days, respectively. Resumption of diet which means the period to start oral feeding after surgery was later at the laparoscopy one than in the open one (5.6 vs. 6.4 days). The duration of drainage also was longer at the laparoscopy one than the open one (6.0 vs. 6.5 days). In these terms, the mean follow-up period of patients was 106 months (139.1 and 58.6 months, respectively). Here it was noted that 16 patients had experienced an early complication and there were 5 with postoperative ileus, 4 with wound complication, 4 with fluid collection at operation site, 3 with pancreatitis, and 1 with bleeding, and there were no significant differences between the 2 groups. Notably, there were 7 patients who had a late complication and 3 with cholangitis, 3 with postoperative ileus, 2 with HJ stricture, and 2 with intrahepatic duct (IHD), and a common hepatic duct (CHD) stone. There were also no significant differences noted between the 2 groups. But the biliary complications which involve postoperative cholangitis, HJ stricture, IHD or CHD stone are shown to have been different between the 2 groups (open, 4 vs. laparoscopy, 0; P = 0.045). In order to find out the factors affecting the biliary complication, a univariate analysis was first performed. Among them, the factors with low P-values were selected, and there were as noted the operation type, cyst size, preoperative cholangitis, and intraoperative transfusion. Therefore, a multivariate analysis was performed with factors, operation type (odds ratio [OR], 0; 95% confidence interval [CI], 0; P = 0.997), cyst size (OR, 1.511; 95% CI, 0.943–2.549; P = 0.084), preoperative cholangitis (OR, 1.30; 95% CI, 0.140–12.083; P = 0.817), and intraoperative transfusion (OR, 20.78; 95% CI, 1.170–369.022; P = 0.039) (Table 3).
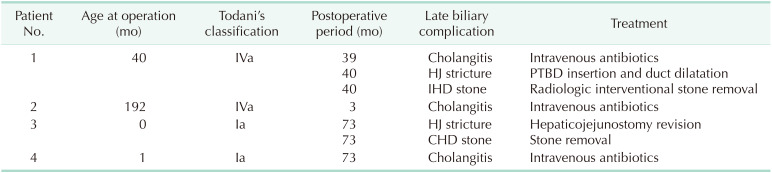
The clinical presentations and treatment for patients with late biliary complications are depicted in Table 4. In the case of patient 1, a choledochal cyst excision with Roux-en-Y HJ was performed at 40 months and there was continued follow-up. Furthermore, 39 months after the operation, it was noted that the patient was presented with abdominal pain and fever. At that time, there were elevations of liver function test, CRP and leukocytosis. After being diagnosed as cholangitis, we used intravenous antibiotics for about 2 weeks, and the patient was discharged with improved symptoms and laboratory findings. After 1 month, the patient was readmitted for abdominal pain and fever. We checked the abdomen sonography and CT and confirmed the IHD stone and HJ stricture. We inserted the percutaneous transhepatic biliary drainage (PTBD) and performed bile duct balloon dilatation twice. As observed, the radiologic interventional stone removal and PTBD removal were performed 2 months after PTBD insertion.
Patient 2 underwent a choledochal cyst excision with Roux-en-Y HJ at 16 years of age and had continued follow-up. At 3 months after the operation, she was presented with abdominal pain and fever. There were elevations of liver function test, CRP and an abdomen CT confirmed the diagnosis of cholangitis. We used intravenous antibiotics for about 3 days and she was discharged with improved symptoms and laboratory findings.
Patient 3 underwent a choledochal cyst excision with Roux-en-Y HJ at 14 days of age and had continued follow-up. At 73 months after the operation, the patient was presented with repeated abdominal pain. We found out that there was present IHD dilatation with sludge, CHD stone, HJ stricture by abdomen sonography and magnetic resonance cholangiopancreatography (MRCP), and at that time performed the HJ revision. After 1 month of reoperation, the HJ revision was performed again due to an HJ site leakage, which was found out as presenting as a symptom of peritonitis. There were no unusual findings after these reoperations.
Patient 4 underwent a choledochal cyst excision with a Roux-en-Y HJ at 1 month of age and had continued follow-up. At 73 months after the operation, the patient was presented with abdominal pain and fever. There were elevations of the liver function test, while the CRP and abdomen sonography confirmed the diagnosis of cholangitis. We used intravenous antibiotics for 1 week and oral antibiotics for 1 more week. Later, the patient was discharged with improved symptoms and laboratory findings. It is noted that after 20 months, 29 months, 31 months, and 34 months, the patient was hospitalized with recurred cholangitis, and was discharged later after undergoing antibiotic treatment.
Go to : 
In children, it is known that surgery for choledochal cyst is currently actively performed with laparoscopic surgery, and related papers are also published. In the papers, the researchers compared the overall outcomes of open and laparoscopy surgery and the patient's hospital stay, resumption of diet, and duration of drainage, to come up with conclusions noted in a meta-analysis paper [7].
In the results of our study, the proportion of APBDU in the patient's characteristics was confirmed to be relatively low at 45.4%. This is probably because the cases of the past patients did not perform the test of an MRCP as part of the preoperative workup and therefore had a sonogram only, whereby it is thought that the conclusion could be the result of many falsenegative cases [8]. In the case of operation time, the laparoscopy group was significantly longer, and in the case of intraoperative transfusion, it was found to be significantly less in the laparoscopy group. There was no significant difference in the noted hospital stay, and it was confirmed that the laparoscopy group was slightly delayed in the case of the resumption of diet and duration of drainage, but there was no statistically significant difference in the items compared to the recent 1.5 years results. It is similar to the comparison between open and laparoscopy groups in other study groups. For these reasons, as based on these outcomes, laparoscopy is considered to be a better method, but there are still controversial parts in the stability. Moreover, Yeung et al. [9] reported that 5 out of 20 patients needed reoperation during 67-month follow-up after the laparoscopic surgery (1 case of bile leakage, 4 cases of anastomosis site stricture, and 2 cases of residual choledochal cyst). In addition, there have been many studies that questioned stability of the patient in the long term, due to a significant postoperative complication after laparoscopic surgery [101112131415].
In this study, postoperative complication was compared to confirm stability, and there was no statistically significant difference in the open and laparoscopy group for noting an early complication that occurred within 30 days after the postoperation. There was no statistically significant difference when comparing the open and laparoscopy group in late complications occurring since 30 days after the postoperation. When categorizing cholangitis, biliary stricture, IHD, and CHD stone as biliary complications, the laparoscopy group had a smaller complication rate than the open group, and significant differences were found between the 2 groups. When examining other factors affecting the biliary complication, an intraoperative transfusion was significantly correlated and when analyzed by logistic regression, it was identified as the only influencing factor (Table 3). This is in turn related to the estimated blood loss in the operating room, and the patient's condition before surgery which is severely inflamed, resulting in blood loss occurring during dissection and resection. In the case of laparoscopic surgery, surgeons that overcome the learning curve to some extent can perform more precisely in the magnified field, thus reducing patient blood loss, and thus reducing the risk of a later biliary complication [101617]. Even in our hospital, surgeons are already experienced in other laparoscopic operations, and for this reason, the rate of complication is relatively small.
The limitation is that this is the first retrospective study, which has selection bias and limitations at the patient group distribution. There could have been selection bias from 2011 to 2012 when the laparoscopic surgery was introduced, but after that period, there were no open cases other than open conversion due to severe inflammation. If the learning curve describes the process of adapting to laparoscopic surgery, it can be thought that this selection bias might not be significant because there have been no open cases after 2015, and all operations were performed by laparoscopy. The second limitation is that the data obtained from a single center is reasonably considered to be small in sample size. In addition, 2 other surgeons performed surgery as a limitation, and the follow-up period of open and laparoscopy group is shown to be different as analyzed. The follow-up period of patients with laparoscopy surgery is known to be relatively short. Also, the number of cases of late complication is very small, and for that reason the statistical significance is low. If we can study in the future in a multicenter and follow-up for a longer period of time, we may be able to reach more accurate results.
In conclusion, it is shown that laparoscopic choledochal cyst excision with HJ is a safe and feasible technique even in a young patient. Upon review, the long-term biliary complication rate was lower using this procedure, as compared to open surgery.
Go to : 
References
1. Vater A, Ezler CS. Dissertatio de Scirrhis viscerum occasione sectionis viri tympanite defunte. Wittenburgae. 1723; 881:22.
2. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977; 134:263–269. PMID: 889044.
3. Lipsett PA, Pitt HA. Surgical treatment of choledochal cysts. J Hepatobiliary Pancreat Surg. 2003; 10:352–359. PMID: 14598135.

4. Farello GA, Cerofolini A, Rebonato M, Bergamaschi G, Ferrari C, Chiappetta A. Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc. 1995; 5:354–358. PMID: 8845978.
5. Lee JH, Kim SH, Kim HY, Choi YH, Jung SE, Park KW. Early experience of laparoscopic choledochal cyst excision in children. J Korean Surg Soc. 2013; 85:225–229. PMID: 24266013.

6. Kimura Y, Takada T, Kawarada Y, Nimura Y, Hirata K, Sekimoto M, et al. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007; 14:15–26. PMID: 17252293.

7. Shen HJ, Xu M, Zhu HY, Yang C, Li F, Li KW, et al. Laparoscopic versus open surgery in children with choledochal cysts: a meta-analysis. Pediatr Surg Int. 2015; 31:529–534. PMID: 25895070.

8. Park SW, Koh H, Oh JT, Han SJ, Kim S. Relationship between anomalous pancreaticobiliary ductal union and pathologic inflammation of bile duct in choledochal cyst. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:170–177. PMID: 25349833.

9. Yeung F, Chung PH, Wong KK, Tam PK. Biliary-enteric reconstruction with hepaticoduodenostomy following laparoscopic excision of choledochal cyst is associated with better postoperative outcomes: a single-centre experience. Pediatr Surg Int. 2015; 31:149–153. PMID: 25433691.

10. Lee KH, Tam YH, Yeung CK, Chan KW, Sihoe JD, Cheung ST, et al. Laparoscopic excision of choledochal cysts in children: an intermediate-term report. Pediatr Surg Int. 2009; 25:355–360. PMID: 19255762.
11. Jang JY, Yoon YS, Kang MJ, Kwon W, Park JW, Chang YR, et al. Laparoscopic excision of a choledochal cyst in 82 consecutive patients. Surg Endosc. 2013; 27:1648–1652. PMID: 23239299.

12. Kim NY, Chang EY, Hong YJ, Park S, Kim HY, Bai SJ, et al. Retrospective assessment of the validity of robotic surgery in comparison to open surgery for pediatric choledochal cyst. Yonsei Med J. 2015; 56:737–743. PMID: 25837180.

13. Margonis GA, Spolverato G, Kim Y, Marques H, Poultsides G, Maithel S, et al. Minimally invasive resection of choledochal cyst: a feasible and safe surgical option. J Gastrointest Surg. 2015; 19:858–865. PMID: 25519084.

14. Diao M, Li L, Cheng W. Recurrence of biliary tract obstructions after primary laparoscopic hepaticojejunostomy in children with choledochal cysts. Surg Endosc. 2016; 30:3910–3915. PMID: 26659232.

15. Diao M, Li L, Cheng W. Laparoscopic redo hepaticojejunostomy for children with choledochal cysts. Surg Endosc. 2016; 30:5513–5519. PMID: 27126624.

16. Diao M, Li L, Cheng W. Laparoscopic versus open Roux-en-Y hepatojejunostomy for children with choledochal cysts: intermediate-term follow-up results. Surg Endosc. 2011; 25:1567–1573. PMID: 21052722.

17. Senthilnathan P, Patel ND, Nair AS, Nalankilli VP, Vijay A, Palanivelu C. Laparoscopic management of choledochal cyst-technical modifications and outcome analysis. World J Surg. 2015; 39:2550–2556. PMID: 26067634.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download