Abstract
Purpose
Diverting stoma (DS) and transanal tube (TAT) are the 2 main procedures for reducing anastomotic leak (AL) in rectal cancer surgery. However, few studies have compared the protective effect of the 2 modalities against AL.
Methods
Total of 165 patients with mid rectal cancer, who underwent curative resection from 2012 to 2017, were included. Clinical characteristics and outcomes were compared. Risk factors for AL were identified using multivariate analysis.
Results
The DS group had lower tumor location, higher rates of neoadjuvant concurrent chemoradiotherapy, and longer operative time than the TAT group. However, the level of the anastomosis did not show statistically significant differences (DS: 4.6 cm vs. TAT: 4.9 cm, P = 0.061). AL occurred in 14 of the 165 patients (8.5%), with 10 (10.2%) in the DS group and 4 (6.0%) in the TAT group (P = 0.405). On multivariate analysis, only low body mass index (BMI) and smoking were significantly related to AL. Neither the protection method nor neoadjuvant chemoradiotherapy demonstrated statistical differences in AL. Seven of 10 patients in the DS group who experienced AL were treated conservatively, while all 4 in the TAT group underwent reoperation.
Conclusion
TAT seems to have comparable protective effect against AL to DS. However, in AL, DS appeared to be more effective in preventing reoperation. Therefore, DS is recommended in patients with low BMI or smoking, and with an expected higher probability of morbidity or mortality in case of reoperation. In other cases, TAT may be considered as an alternative to DS.
Anastomotic leak (AL) is defined as communication between intra- and extraluminal compartments caused by a defect in intestinal wall integrity at the anastomosis [1]. AL after colorectal surgery is one of the most dreadful complications because it can cause septic complications due to intraabdominal contamination from fecal content and may require reoperation often followed by creating a stoma [23]. In addition, AL after cancer surgery is known to increase locoregional recurrence and decrease survival rate [45].
Despite the development of novel surgical techniques and instruments, the incidence rate of AL has not declined in recent decades [6]. According to previous research that analyzed the results of rectal cancer surgeries from 1990 to 2008 in 84 prospective cohort studies, the AL rate was approximately 11% and remains considerably high [2]. Therefore, studies aimed at reducing AL are of ongoing interest, and the 2 most common protective methods for preventing AL are diverting stoma (DS) and transanal tube (TAT).
TAT is a newer protective method than DS and has advantages for reducing complications and/or the discomfort associated with DS. Recently, the benefit of using TAT was described in several studies including a multicenter retrospective cohort study [7] and meta-analysis [8]. However, while using TAT is considered useful compared to not applying any protective methods, little has been studied about to what extent the TAT will be able to replace DS, which is known to have the most powerful anastomosis protection effect.
The purpose of this study was to identify under which conditions the TAT was likely to replace DS by analyzing the criteria for selection of the protection methods (DS or TAT) and its clinical results including AL in the mid rectal cancer, where the use of DS is difficult to determine.
Prospectively collected data from patients who underwent curative resection for primary rectal cancer at Seoul St. Mary's Hospital (Seoul, Korea) between February 2012 and January 2017, were retrospectively reviewed. Data of rectal cancer cases located between 5 and 10 cm above the anal verge (AV) determined by initial colonoscopy or MRI was specifically selected. Patients who underwent robot-assisted operative, surgery with no anastomosis (abdominoperineal resection, Hartmann operation), coloanal anastomosis, transanal local excision (including laparoscopic-assisted operative like transanal endoscopic microsurgery), synchronous cancer surgery, using a different type of TAT, or stage IV were excluded. This study was approved by the Institutional Review Board (IRB) of the Catholic Medical Center, The Catholic University of Korea (No. KC19RESI0073). Patient' consent to participate in this study was waived according to the IRB's policy; however, informed consent for treatment, including an understanding of possible complications of the procedure, was provided by each patient before surgery.
Patients with clinically suspicious T3 and/or lymph node metastasis revealed on preoperative MRI examination underwent neoadjuvant concurrent chemoradiation therapy (CCRT). CCRT included radiation therapy (RT) using a dose of 50.4 Gy in 28 fractions to the pelvis accompanied by 2 cycles of 5-fluorouracil/leucovorin chemotherapy. Chemotherapy was restarted within 8 weeks after surgery using the same regimen (4 cycles). Patients who did not undergo neoadjuvant therapy and were diagnosed with locally advanced rectal cancer in the permanent pathology report after surgery underwent the same RT with 6 cycles of the same chemotherapy.
Every patient took 4 L of polyethylene glycol (Colyte powder, Taejoon Pharm Co., Seoul, Korea) for bowel preparation and was administered prophylactic antibiotics before surgery. Three specialized colorectal surgeons in the authors' institution performed the surgeries. Surgery was mostly performed according to the principle of inferior mesenteric artery high ligation (D3 lymphadenectomy) and end-to-end fashion anastomosis. Whether to use TAT or DS for reducing AL was left to the discretion of each surgeon according to individual patient clinical characteristics and intraoperative findings.
The authors' center has used TAT since 2012. It is made from silicone, which is a soft and flexible material. There are 2 parts to this tube: one is 17.5 × 7 × 150 mm in dimensions and a wide drainage part; and the other is a 30-Fr tube, which is connected to a drainage part. Usually, all drainage parts are located proximal to the anastomosis. Particular attention is devoted to ensuring the colon is not tented by TAT and to generate pressure. The TAT was anchored to the perianal region using a skin suture. Detailed characteristics with photographs are available in a previous report by the authors [9].
The TAT was removed median of 5 days (range, 4–7 days) after surgery according to diet progression. Patients were discharged on postoperative days 6–8 if they experienced no complications and/or problems with dietary intake. Patients visited the outpatient department 1–2 times weekly after discharge, and adjuvant treatment, if needed, was initiated within 8 weeks after surgery. The criteria for discharge and follow-up was the same for the DS group.
Variables including age, sex, body mass index (BMI), American Society of Anesthesiologists physical status (ASA PS) classification, diabetes mellitus (DM), smoking history, previous surgical history, preoperative stent insertion history, preoperative serum albumin, neoadjuvant CCRT, tumor location (distance from the AV), operative time, estimated blood loss, intraoperative transfusion, anastomosis fashion (end-to-end or end-to-side), vascular ligation type (high or low), approach type (laparotomy or laparoscopy), synchronous resection of other intra-abdominal organ(s), intraoperative complications, tumor size (≤3 or >3 cm), pathological stage, protection method (DS or TAT), and postoperative complications including AL were identified and analyzed. BMI was classified by 3 categories according to the 1st and 3rd quartile number, because its effect on AL would not be linear. Tumor location was determined by colonoscopy/sigmoidoscopy or MRI, and if neoadjuvant CCRT was performed, data checked after neoadjuvant treatment was adopted. Level of anastomosis was calculated by subtracting pathological distal resection margin figures from the tumor location.
The only concern in the present study was clinical AL, which was suspected when signs and/or symptoms, such as abdominal pain with tenderness, muscle guarding, fever, rectovesical or rectovaginal fistula, pus, or fecal discharge for the drain, discharge of abdominal material per rectum or chronic ileus with no improvement over 7 days, developed. The diagnosis was confirmed using one or a combination of CT, sigmoidoscopy, or surgery.
Continuous variables are expressed as median (range), and differences between the groups were compared using the Mann-Whitney U-test. Categorical variables are expressed as number (%) and were compared using the Fisher exact test. Logistic regression was used for multivariate analysis to identify significant factors affecting AL. Variables with P < 0.20 in the univariate analysis comparing patients who had AL and those who did not, neoadjuvant CCRT, and protection method were included and analyzed in the multivariate analysis. All analyses were performed using IBM SPSS Statistics ver. 24 (IBM Corp., Armonk, NY, USA); differences with P < 0.05 were considered to be statistically significant.
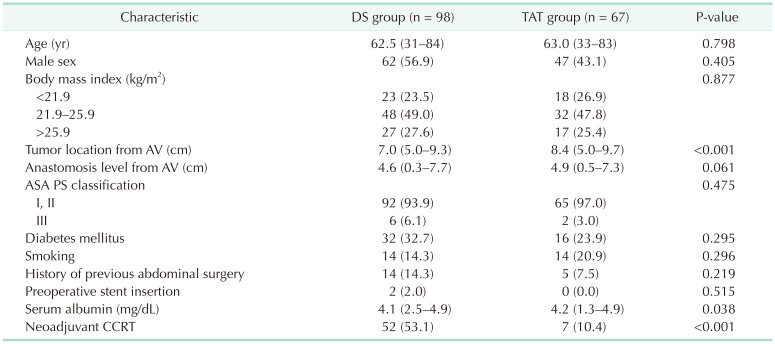
A total of 165 patients met the inclusion/exclusion criteria in the study period, with 98 in the DS group and 67 in the TAT group. There were no significant differences in age, sex, BMI, ASA PS classification, DM, smoking history, history of previous abdominal surgery, preoperative stent insertion, and serum albumin levels between the 2 groups. Level of the tumor lower margin from the AV was significantly lower in the DS group than in the TAT group (7.0 cm [range, 5.0–9.3 cm] vs. 8.4 cm [5.0–9.7 cm], P < 0.001). However, this difference disappeared in comparison of anastomosis level (4.6 [0.3–7.7] cm vs. 4.9 [0.5–7.3] cm, P = 0.061). The DS group had more patients who underwent neoadjuvant CCRT (52 [53.1%] vs. 7 [10.4%], P < 0.001) (Table 1).
Perioperative outcomes and pathological results are summarized in Table 2. Median operative time was significantly longer in the DS group (281 minutes [125–660 minutes] vs. 240 minutes [130–445 minutes], P < 0.001). Although there were trends that patients who received low vascular ligation (6 [6.1%] vs. 10 [14.9%], P = 0.105) and showed earlier stage (0–I) were applied TAT, but differences were not statistically significant. Estimated blood loss, transfusion, simultaneous other organ resection, pathologic (p) T and pN stage were also showed no difference between the groups. Resume of soft diet was faster in the DS group (3 days [1–30 days] vs. 5 days [2–10 days], P < 0.001). Postoperative hospital stay seemed to be similar, but statistically it was found to be longer for the DS group (7 days [3–44 days] vs. 7 days [5–18 days], P = 0.025). In total, 14 of 165 patients (8.5%) experienced AL, of whom 10 of 98 (10.2%) were in the DS group and 4 of 67 (6.0%) were in the TAT group; this difference, however, was not statistically significant (P = 0.405).
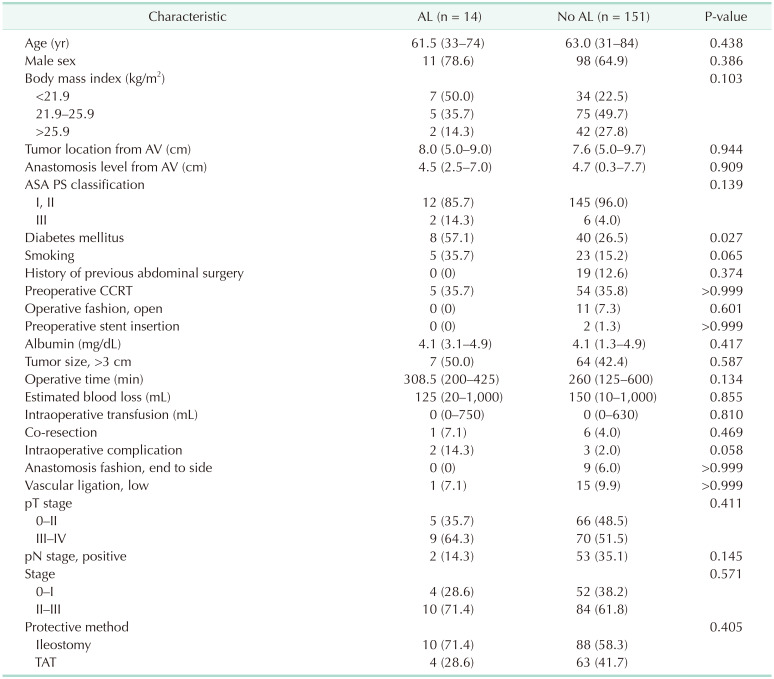
The 2 groups exhibited different characteristics such as tumor location, neoadjuvant CCRT, and operative time. To analyze the effect of multiple variables on AL, comparisons of clinical characteristics between patients who experienced AL (n = 14) and those who did not (n = 151) were performed (Table 3). Among patients who experienced AL, there were significantly more patients with DM (40 [26.5%] vs. 8 [57.1%], P = 0.027). Additionally, ASA PS classification, smoking history, operative time, intraoperative complication, and positive lymph nodes were identified as potential associated factors of AL (P < 0.20). However, neither preoperative CCRT (no leak: 54 [35.8%] vs. leak: 5 [35.7%], P > 0.999) nor protective method (DS; no leak: 88 [58.3%] vs. leak: 10 [71.4%], P = 0.405) showed significant difference between patients experienced AL and who did not.
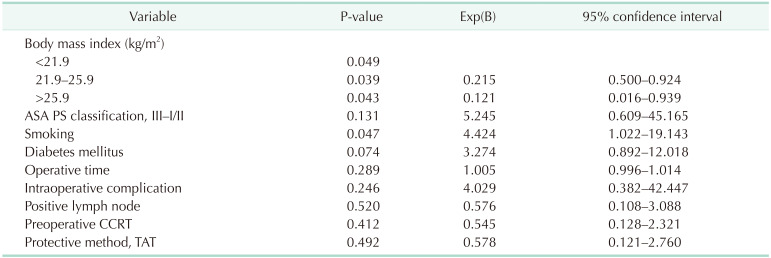
In multivariate analysis, choosing TAT compared to DS showed no significant influence on AL (odds ratio [OR], 0.578; 95% confidence interval [CI], 0.121–2.760; P = 0.492). Optimal BMI (OR, 0.215; 95% CI, 0.500–0.924; P = 0.039) or high BMI (OR, 0.121; 95% CI, 0.016–0.939; P = 0.043) was shown to have positive effect on AL than low BMI. History of smoking (OR, 4.424; 95% CI, 1.022–19.143; P = 0.047) appeared to have a significantly negative impact on the occurrence of AL. Neoadjuvant CCRT was not found to be a significant factor in our cohort (OR, 0.545; 95% CI, 0.128–2.321; P = 0.412) (Table 4).
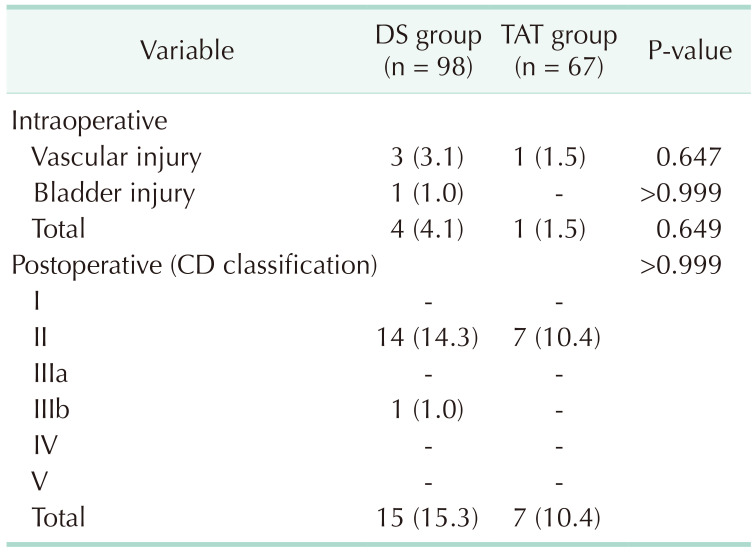
Intra- and postoperative complications except AL in the DS and TAT groups are summarized in Table 5. Intraoperative complications were mostly other organ injuries during the procedure. Ileus was the most common complication in both groups especially in the DS group, but the difference was not significant (12 [12.2%] vs. 4 [6.0%], P = 0.284). There was no difference in intra- and postoperative complications, and no complication was reported associated with applying TAT. In terms of Clavien-Dindo classification for postoperative complication, there was no difference also. All the patients were managed successfully with conservative care except for 1 postoperative bleeding case. Delayed stoma complication was not checked in this data.
Patients with AL were managed using additional treatment including antibiotics, percutaneous drainage, or reoperation. In the DS group, 3 of 10 patients were managed only with conservative care (including antibiotics), 4 patients were managed using a radiologic interventional procedure (percutaneous drainage), and the other 3 patients underwent reoperation. In contrast, all 4 patients with AL in the TAT group required emergent surgical management (Fig. 1).
The method to reduce AL is an important issue for all colorectal surgeons, and the most frequently used of which is DS and TAT currently. However, little has been studied about to what extent the TAT can replace DS. Especially in mid rectal cancer, where it is difficult to predict whether there will be an AL, it is hard to choose which method is beneficial for the patient. In our previous study, we compared effectiveness of DS and TAT retrospectively in patients with rectal cancer located 5–10 cm above the AV who did not undergo preoperative CCRT [9]. With the present study, which complements some limitations of the previous study such as small number of patients and no neoadjuvant CCRT case, the authors were able to identify the possibility of increasing the coverage of TATs.
DS is regarded as the most powerful protective method for AL because it prevents the passage of luminal contents past the anastomosis, and it is usually included as a part of the surgical procedure for treating AL. However, additional surgery with general anesthesia would be necessary for stoma repair. Moreover, performing DS is more time-consuming and DS itself can lead to several morbidities such as skin irritation, parastomal hernia, acute renal failure, and ileus [1011]. In this study, the time to resuming soft diet in the TAT group was significantly later than in the DS group (Table 2). It was because the surgeons started diet much conservatively for the TAT group concerning for the newly adopted TAT. Nevertheless, postoperative length of hospital stay was longer for the DS group. It seems related to more frequent postoperative ileus in the DS group, although it was not statistical (12 [12.2%] vs. 4 [6.0%], P = 0.284). According to a previous study of Snijders et al. [12], who compared the proportion of DS and AL among several hospitals, the adjusted proportion of DS and AL demonstrated no significant association, and the proportion of severe AL demonstrated no difference among hospitals, regardless of whether they created more DS. These data suggest that DS does not lower AL itself but mitigates the after-effects of AL. Therefore, research investigating novel protective methods with a similar effect is warranted.
Indwelling of rectal tubes was first described in the 1960s [13], and TAT has frequently been studied recently after the introduction of total mesorectal excision had become more concerned about AL [8]. The presumed mechanism of the protective effect of TAT is that it lowers intraluminal pressure, which is an important factor related to AL [14]. Recently, many systematic reviews and meta-analyses have consistently reported that TAT significantly lowers AL compared with not using it [7815]. It was also reported that TAT could be effective in treatment when AL occurred [16]. However, there have been few studies addressing whether TAT has protective effect similar to DS by direct comparison.
Recently, Wang et al. [17] recommended the use of TAT because it has effect similar to DS in their meta-analysis. However, they drew conclusions by comparing the incidence of AL from studies that compared DS with no-protection and other studies that compared TAT with no-protection. Unless those studies were investigated under similar clinical conditions including possible risk factors such as tumor location, preoperative RT, or operative time, they are considered to contain some logical errors.
In this study, the DS group exhibited lower tumor location, higher rates of neoadjuvant CCRT, and longer operative time. Also, the DS group patients without neoadjuvant CCRT presented significantly lower tumor location, shorter distal resection margin length, lower serum albumin level, longer operative time, and larger amount of intraoperative transfusion than the TAT group patients without neoadjuvant CCRT (data not shown). This suggests that surgeons who contributed to this study also preferred DS as protective method for AL in difficult and/or risky cases. However, in order for the use of DS to be justified, it is necessary to make sure that these factors have really increased the risk of AL.
The tumor location was about 1.4-cm difference in median. However, the anastomosis level, which is believed to have a greater effect than the tumor location on AL, did not differ statistically, and the difference was only 0.3 cm. It is questionable whether this difference was significant enough to affect the AL rate.
For longer operative time in the DS group, it is a factor that reflects the difficulty of surgery and is actually considered a risk factor for AL [18]. However, the 40-minute surgical time difference also includes the time to make stoma. In addition, even if the difficulty of surgery was higher in the DS group, it seems unlikely that the difficulty itself affected the anastomosis, given that there is no difference in complications during or after surgery as seen in Table 5.
The effect of RT on AL still remains controversial. According to a meta-analysis [19] that analyzed studies investigating AL rates and rectal cancer surgeries from 2000 to 2015, although short course RT was significant risk factor for AL, long course RT was not. In addition, a large randomized controlled trial conducted by The Medical Research Council CR07 [20] or Dutch total mesorectal excision trial [21] demonstrated no difference in AL rate in comparison of preoperative RT received group with postoperative RT received group and preoperative RT received group with not received group. A recent post hoc analysis study [22] using patient data from their own randomized controlled trial reported that exposure to RT did not increase AL; however, AL occurred significantly more often in patients with radiation proctitis after RT. Therefore, the influence of RT on AL should be studied further; moreover, studies comparing TAT with DS may be designed to compare patients who are not suspected to have radiation proctitis.
In the present study, it appears that surgeons chose DS conservatively without any particular concern for patients with neoadjuvant CCRT. There was a limit to having sufficient verification power because TAT was applied to only 7 patients who performed neoadjuvant CCRT (7 of 59, 11.9%). However, in the DS group, there was no difference in AL rate when subgroup analysis was performed on patients who received neoadjuvant CCRT and those who did not (4 [7.7%] vs. 6 [13.0%], P = 0.508). In the patient group who performed CCRT and DS, there were fewer patients with a tumor size greater than 3 cm (CCRT: 12 [23.1%] vs. non-CCRT: 29 [63.0%], P < 0.001), and estimated blood loss was less (CCRT: 100 mL [20–1,000 mL] vs. non-CCRT: 200 mL [20–1,000 mL], P = 0.031). There was no significant difference in other variables. Considering that DS does not reduce AL rate itself, but lowers the consequences of leak, at least in our data neoadjuvant CCRT did not affect AL rate.
All 3 factors above were not significant in the multivariate analysis that identified risk factors of AL (Table 4). The DS and TAT showed no difference in performance in the protection of the anastomosis regardless of CCRT as seen in our study presents by analyzing mid rectal cancer cohort of 5 years. Because the AL rate of the DS group was 10.2% in the present study and DS could not lower the rate of AL, it must be reconsidered that many of the 98 patients in the DS group had to endure disadvantages of DS owing to surgeon fears and apprehensions.
Tobacco use and lower BMI were significant risk factors for increasing AL rate in our multivariate analysis. Smoking is known to cause adverse impact on wound healing through various toxic effects and oxidative stress, so it has been reported in various studies as a risk factor for increasing AL after colorectal surgery [182324]. Four weeks of smoking cessation is encouraged before surgery. However, optimal length of cessation is still in study and toxic effect of smoking is known to be dose-dependent [24]. Thus it is recommended that cessation of smoking should be encouraged for patients who need surgery after explanation about increasing possibility of complications such as AL.
The effect of BMI on AL after colorectal surgery is debatable [181925]. However, high BMI seems to be related to surgical difficulty and this could be overcome by an experienced surgeon in high volume center. There are limits to studies that have reported high BMI negatively affect AL, because they classified BMI into simply normal and high. Recent studies which classified BMI into low, normal, and high have reported different results that low BMI increases early complications after colorectal surgery compared to normal or high BMI [2627]. There should be additional studies because effect of BMI on surgical outcome seems to have complex correlation with some metabolism-associated variables such as nutrition [27] or sarcopenia [28].
Meanwhile, the conventional preference of DS may be reasonable in one sense because when AL occurred in the present study, 30% of the DS group underwent reoperation and 30% were improved by antibiotics only. In contrast, all patients in the TAT group required reoperation (Fig. 1). This is probably because although both methods are based on the principle of lowering intraluminal pressure, there is a difference in that fecal material does pass through the anastomotic site in TAT. DS seems superior to minimize the adverse effect(s) when AL occurs.
Therefore, according to our study, it is suggested that the decision on which protection method to use should be made based on sufficient preoperative and intraoperative examination, not empirically. DS should be preferentially considered when a patient has many known risk factors for AL, a patient is considered to be at high risk in reported scoring systems of predicting AL [192329], or a patient whose postoperative complications are expected to be high [30].
Due to the retrospective design of the present study, it may have been limited by selection bias given that the decision for protective method was made by each surgeon intraoperatively. In addition, the statistical power of study may have been low due to the relatively small sample size of the patients who experienced AL. However, considering the severe adverse effects of AL, designing prospective studies would be difficult, if not unethical. Based on data from previous investigations, we believe that well-designed studies should aim to accumulate further data to determine circumstances in which TAT can be used as a replacement for DS.
References
1. Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery. 2010; 147:339–351. PMID: 20004450.

2. Paun BC, Cassie S, MacLean AR, Dixon E, Buie WD. Postoperative complications following surgery for rectal cancer. Ann Surg. 2010; 251:807–818. PMID: 20395841.

3. McArdle CS, McMillan DC, Hole DJ. Impact of anastomotic leakage on long-term survival of patients undergoing curative resection for colorectal cancer. Br J Surg. 2005; 92:1150–1154. PMID: 16035134.

4. Ha GW, Kim JH, Lee MR. Oncologic impact of anastomotic leakage following colorectal cancer surgery: a systematic review and meta-analysis. Ann Surg Oncol. 2017; 24:3289–3299. PMID: 28608118.

5. Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg. 2011; 253:890–899. PMID: 21394013.
6. Shogan BD, Carlisle EM, Alverdy JC, Umanskiy K. Do we really know why colorectal anastomoses leak? J Gastrointest Surg. 2013; 17:1698–1707. PMID: 23690209.

7. Goto S, Hida K, Kawada K, Okamura R, Hasegawa S, Kyogoku T, et al. Multicenter analysis of transanal tube placement for prevention of anastomotic leak after low anterior resection. J Surg Oncol. 2017; 116:989–995. PMID: 28743178.

8. Zhao WT, Li NN, He D, Feng JY. Transanal tube for the prevention of anastomotic leakage after rectal cancer surgery: a systematic review and meta-analysis. World J Surg. 2017; 41:267–276. PMID: 27734078.

9. Kim MK, Won DY, Lee JK, Kang WK, Kim JG, Oh ST. Comparative study between transanal tube and loop ileostomy in low anterior resection for mid rectal cancer: a retrospective single center trial. Ann Surg Treat Res. 2015; 88:260–268. PMID: 25960989.

10. Floodeen H, Hallböök O, Hagberg LA, Matthiessen P. Costs and resource use following defunctioning stoma in low anterior resection for cancer: a long-term analysis of a randomized multicenter trial. Eur J Surg Oncol. 2017; 43:330–336. PMID: 28069399.
11. Rullier E, Le Toux N, Laurent C, Garrelon JL, Parneix M, Saric J. Loop ileostomy versus loop colostomy for defunctioning low anastomoses during rectal cancer surgery. World J Surg. 2001; 25:274–278. PMID: 11343175.

12. Snijders HS, van Leersum NJ, Henneman D, de Vries AC, Tollenaar RA, Stiggelbout AM, et al. Optimal treatment strategy in rectal cancer surgery: should we be cowboys or chickens? Ann Surg Oncol. 2015; 22:3582–3589. PMID: 25691277.

13. Rack RJ. Advantages of an indwelling rectal tube in anterior resection and anastomosis for lesions involving the terminal portion of the colon. Dis Colon Rectum. 1966; 9:42–48. PMID: 5904614.

14. Lee SY, Kim CH, Kim YJ, Kim HR. Impact of anal decompression on anastomotic leakage after low anterior resection for rectal cancer: a propensity score matching analysis. Langenbecks Arch Surg. 2015; 400:791–796. PMID: 26318026.

15. Shigeta K, Okabayashi K, Baba H, Hasegawa H, Tsuruta M, Yamafuji K, et al. A meta-analysis of the use of a transanal drainage tube to prevent anastomotic leakage after anterior resection by doublestapling technique for rectal cancer. Surg Endosc. 2016; 30:543–550. PMID: 26091985.

16. Shalaby M, Thabet W, Buonomo O, Lorenzo ND, Morshed M, Petrella G, et al. Transanal tube drainage as a conservative treatment for anastomotic leakage following a rectal resection. Ann Coloproctol. 2018; 34:317–321. PMID: 30572421.

17. Wang FG, Yan WM, Yan M, Song MM. Comparison of anastomotic leakage rate and reoperation rate between transanal tube placement and defunctioning stoma after anterior resection: a network meta-analysis of clinical data. Eur J Surg Oncol. 2019; 45:1301–1309. PMID: 30738589.

18. McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg. 2015; 102:462–479. PMID: 25703524.

19. Arezzo A, Migliore M, Chiaro P, Arolfo S, Filippini C, Di Cuonzo D, et al. The REAL (REctal Anastomotic Leak) score for prediction of anastomotic leak after rectal cancer surgery. Tech Coloproctol. 2019; 23:649–663. PMID: 31240416.

20. Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S, et al. Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet. 2009; 373:811–820. PMID: 19269519.

21. Marijnen CA, Kapiteijn E, van de Velde CJ, Martijn H, Steup WH, Wiggers T, et al. Acute side effects and complications after short-term preoperative radiotherapy combined with total mesorectal excision in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol. 2002; 20:817–825. PMID: 11821466.

22. Ma T, Zhong Q, Cao W, Qin Q, Meng X, Wang H, et al. Clinical anastomotic leakage after rectal cancer resection can be predicted by pelvic anatomic features on preoperative MRI scans: a secondary analysis of a randomized controlled trial. Dis Colon Rectum. 2019; 62:1326–1335. PMID: 31567929.

23. Dekker JW, Liefers GJ, de Mol, Putter H, Tollenaar RA. Predicting the risk of anastomotic leakage in left-sided colorectal surgery using a colon leakage score. J Surg Res. 2011; 166:e27–e34. PMID: 21195424.

24. Baucom RB, Poulose BK, Herline AJ, Muldoon RL, Cone MM, Geiger TM. Smoking as dominant r isk factor for anastomotic leak after left colon resection. Am J Surg. 2015; 210:1–5. PMID: 25910885.
25. Qu H, Liu Y, Bi DS. Clinical risk factors for anastomotic leakage after laparoscopic anterior resection for rectal cancer: a systematic review and meta-analysis. Surg Endosc. 2015; 29:3608–3617. PMID: 25743996.

26. Arkenbosch JH, van Erning FN, Rutten HJ, Zimmerman D, de Wilt JH, Beijer S. The association between body mass index and postoperative complications, 30-day mortality and long-term survival in Dutch patients with colorectal cancer. Eur J Surg Oncol. 2019; 45:160–166. PMID: 30712552.

27. Gebauer B, Meyer F, Ptok H, Steinert R, Otto R, Lippert H, et al. Impact of body mass index on early postoperative and long-term outcome after rectal cancer surgery. Visc Med. 2017; 33:373–382. PMID: 29177167.

28. Simonsen C, de Heer P, Bjerre ED, Suetta C, Hojman P, Pedersen BK, et al. Sarcopenia and postoperative complication risk in gastrointestinal surgical oncology: a meta-analysis. Ann Surg. 2018; 268:58–69. PMID: 29373365.
29. Liu Y, Wan X, Wang G, Ren Y, Cheng Y, Zhao Y, et al. A scoring system to predict the risk of anastomotic leakage after anterior resection for rectal cancer. J Surg Oncol. 2014; 109:122–125. PMID: 24318774.

30. Golden DL, Ata A, Kusupati V, Jenkel T, Khakoo NS, Taguma K, et al. Predicting postoperative complications after acute care surgery: how accurate is the ACS NSQIP surgical risk calculator? Am Surg. 2019; 85:335–341. PMID: 31043191.

Fig. 1
Applied treatment after a diagnosis of anastomotic leak. DS, diverting stoma; TAT, transanal tube.

Table 2
Perioperative outcomes and pathologic results of the diverting stoma (DS) and transanal tube (TAT) group
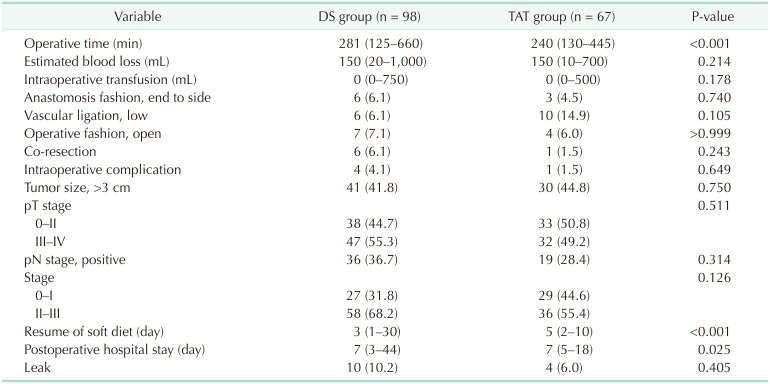
Table 3
Clinical characteristics of patients who presented anastomotic leak (AL) and those who did not




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download