A 30-year-old woman visited the hospital for gradually progressing tingling sensation in her right 5
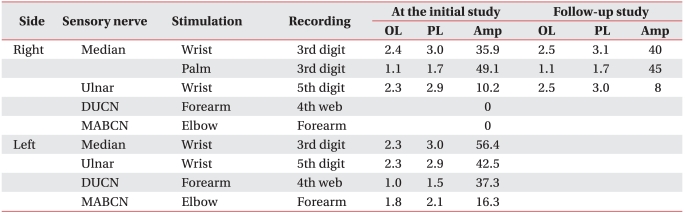
th finger and right shoulder pain, which developed after receiving a cesarean section procedure one year previously. She experienced intermittent pain on her right shoulder and wrist area for 10 years and atrophy of her right hand intrinsic muscles appeared 2 years ago. There was no history of trauma or systemic disease. After recording a detailed history, a chronic sleep habit of abnormal posture with hyperabduction of the right shoulder was revealed. With severe atrophy of the right hand intrinsic muscle (
Fig. 1-A), manual muscle testing based on the Medical Research Council grade of right abductor pollicis brevis muscle was decreased to grade 1, abductor digiti minimi muscle and 1
st dorsal interosseous muscle, grade 4. Hypesthesia on the right medial arm and forearm, and dorsal and palmar aspect of the ulnar side of the hand and the 4
th and 5
th fingers was observed (
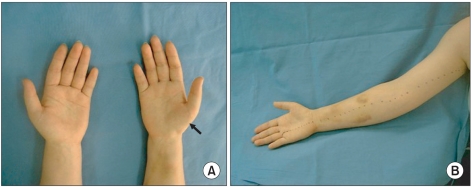
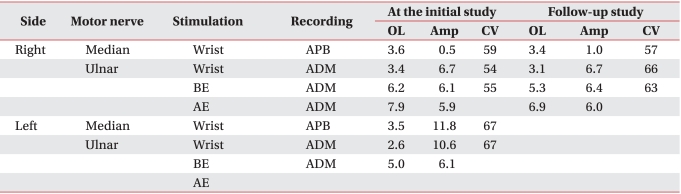
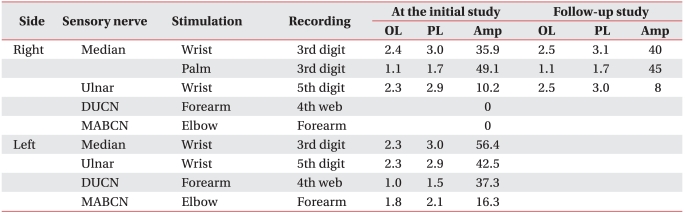
Fig. 1-B). Temperature decrease or edematous change of the right hand was not observed. Provoked test for carpal tunnel syndrome or ulnar neuropathy at the elbow including Phalen test, Froment sign, and Tinel signs of median nerve at the wrist and ulnar nerve at the wrist and elbow were all negative. Loss of radial artery pulse was noticed in Adson's and Wright's test. Roos stress test showed positive findings. Under impression of TOS, nerve conduction studies and needle electromyographic examination were conducted. In a conduction study, decreased amplitude and prolonged latency of compound muscle action potential (CMAP) of median nerve and sensory nerve action potential (SNAP) of ulnar nerve was observed (
Fig. 2-A, D). Right ulnar CMAP was within normal range, yet was decreased compared to the left side (
Fig. 2-B, C). Dorsal ulnar cutaneous and medial antebrachial cutaneous SNAPs were unobtainable. In needle electromyography, abnormal spontaneous activities and/or large motor unit potentials were observed in C8 and T1 segment innervated muscles including abductor pollicis brevis, abductor digiti minimi, 1
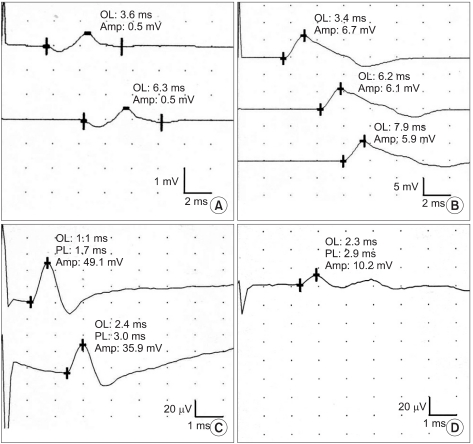
st dorsal interosseous, and extensor indicis muscles. Abnormal spontaneous activity was not observed in cervical paravertebral muscles. Additional studies were performed to evaluate the causes of neurogenic TOS and presence of vascular TOS. Cervical rib was not found in plain radiography and abnormal findings were not observed in the neck MRI and arteriogram (
Fig. 3-A, B). However, a venogram showed mild compression of the right subcalvian vein around the thoracic outlet during shoulder abduction (
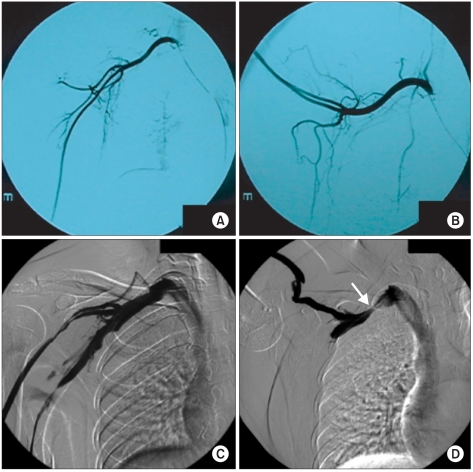
Fig. 3-C, D). Due to absence of edema, color change or cold sensation of upper extremity, venous TOS was excluded. She was diagnosed as true neurogenic TOS due to repetitive abnormal sleeping posture with hyperabducted shoulder. Posture correction education and conservative treatment including physical therapy and trigger point injection was performed. She did not complain of any symptom aggravation, and there was no interval change on the follow-up electrophysiologic study after 4 years (
Table 1,
2).
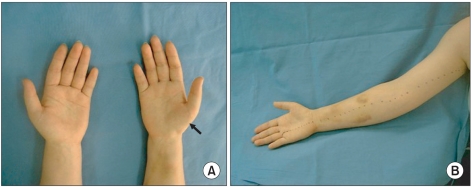 | Fig. 1(A) The right hand thenar muscle was atrophied (arrow). (B) Sensation on the medial side of the arm and forearm and little finger (medial to the dot line) was decreased. 
|
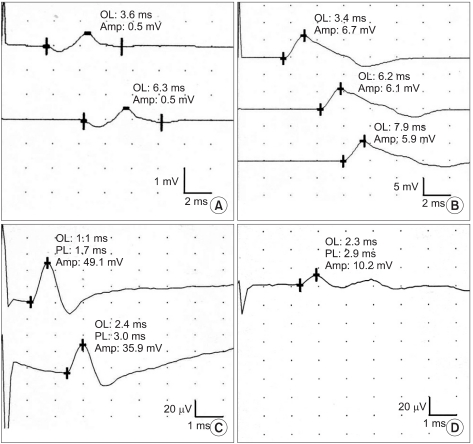 | Fig. 2(A) The right median motor response was of low amplitude. (B) The right ulnar motor response was normal. (C) The right median sensory response was normal. (D) The right ulnar sensory response was of low amplitude. 
|
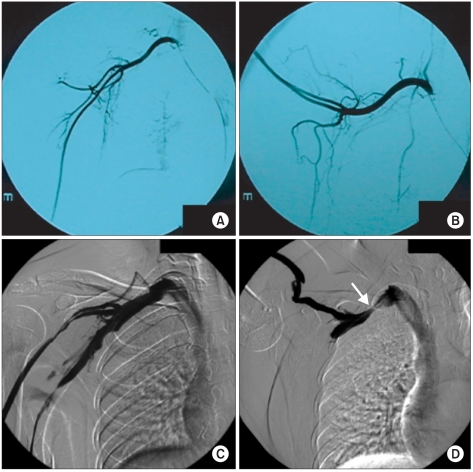 | Fig. 3Arteriogram demonstrated no compression of subclavian artery during shoulder abduction (A, B), but venogram showed compression of the right subcalvian vein around the thoracic out during shoulder abduction (arrow) (C, D). 
|
Table 1
Motor Nerve Conduction Studies
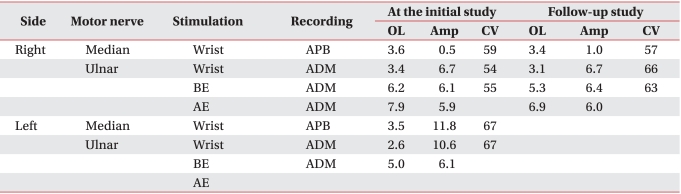

Table 2
Sensory Nerve Conduction Studies





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download