This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To investigate the coexistence rate and related factors of developmental dysplasia of the hip (DDH) and congenital muscular torticollis (CMT), and to determine whether ultrasonography (US) gives good value for screening of DDH in CMT.
Method
We prospectively examined 121 infants (73 males and 48 females) diagnosed with CMT to determine the incidence of DDH by US. We also assessed the relationship between neck US findings and DDH occurrence, and investigated the clinical features of CMT related to DDH.
Results
18 patients (14.9%) were diagnosed as having DDH by US. However, most DDH was subclinical and spontaneously resolved. Only 2 patients (1.7%) needed to be treated with a harness. The positive predictive value of clinical examinations for DDH was 52.6% and patients treated by harness were all clinically positive. DDH was more common in the left side (13 left, 4 right, 1 both), but 6 out of 18 DDH (33.3%) cases presented on the contralateral side of CMT. Sex difference was not observed. Breech presentation and oligohydramnios were not related to DDH occurrence. Neck US findings did not correlate with DDH occurrence.
Conclusion
The coexistence rate of CMT and DDH was concluded to be 14.9%. If only DDH cases that required treatment were included, the coexistence rate of these two disorders would be lowered to 1.7%. All of these patients showed positive findings in clinical examination. Therefore, hip US should not be recommended routinely for patients with CMT.
Go to :

Keywords: Congenital muscular torticollis, Developmental dysplasia of the hip, Ultrasonography
INTRODUCTION
Congenital muscular torticollis (CMT) and developmental dysplasia of hip (DDH) are relatively common disorders in the new born population. The incidence of CMT in the new born population has been estimated at 0.017 to 1.9%.
1-
3 The incidence of DDH with evidence of instability is reported to be 1.0% in new borns, and for infants with evidence of dislocation of hip, the incidence is reported to be 0.1 to 0.15%.
4
Since Iwahara and Ikeda discovered the 14.8% incidence rate of DDH in their patients with CMT in 1962, many reports in the literature have confirmed a consistent relationship between CMT and DDH. Now, the consistent relationship of these two childhood disorders is widely accepted, although the reported concurrence rate varies between 0 and 29%.
1,
5-
9
CMT is apparent on the general physical examination and therefore should not escape notice by the primary care physician or the parents. On the other hand, DDH, whether it be complete dislocation or mild capsular laxity leading to subluxation, may not be so easy to detect.
Ultrasonography (US) is considered one of the most sensitive tools for the diagnosis of CMT
10,
11 and DDH.
12,
13 However, caregivers and the medical system may spend unnecessary cost to screen hip abnormalities with US. This prompted us to search for the coexistence rate of DDH in children with CMT. If the concurrence is high, it may be appropriate to use relatively expensive methods to screen for DDH in all children with CMT. However, if the concurrence is low, it seems less reasonable to use expensive routine screening examinations. In addition, it is important to know how many of these cases of DDH in children with CMT are not apparent on routine physical examination.
This study was conducted to investigate the coexistence rate of CMT and DDH and the related factors of these two disorders, positive predictive value of clinical examination for DDH, and whether US gave good value for screening of DDH in CMT patients.
Go to :

MATERIALS AND METHODS
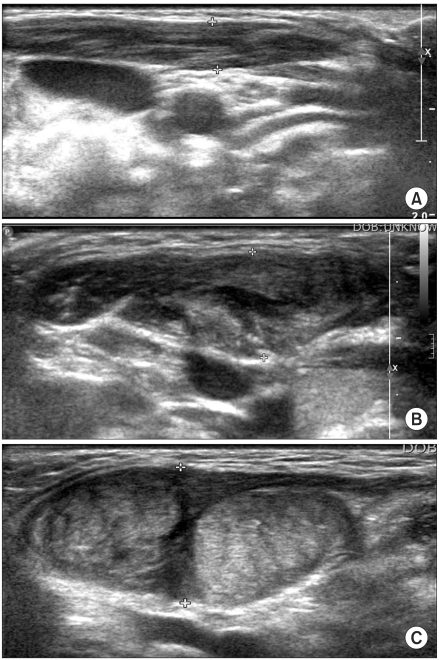
We prospectively examined 121 infants (73 males and 48 females) diagnosed with CMT in our clinic between January 2009 and July 2010. Patients with non-muscular causes of torticollis were excluded by ocular, neurologic, or radiologic examination and neck US. The total number of patients with non-muscular causes of torticollis was eight. Six of them suffered from ocular torticollis, whereas two had torticollis from other neurological causes. Diagnosis of CMT was based on clinical criteria including decreased neck rotation or lateral bending, the characteristic chin-occiput positioning with palpable sternocleidomastoid (SCM) mass and normal ocular or neurologic examination. We confirmed CMT with US in an indefinite case of physical examination without palpable mass on the SCM muscle. The US findings of the SCM muscles were divided into 3 grades according to severity (
Fig. 1). Grade 1 was when the thickness of involved SCM muscle increased compared to the normal side. Grade 2 was when a well-demarcated heteroechoic region was observed. Grade 3 was when diffuse hyperechoic fibrous mass was observed.
14,
15 We also acquired the muscle thickness ratio (involved side/normal side).
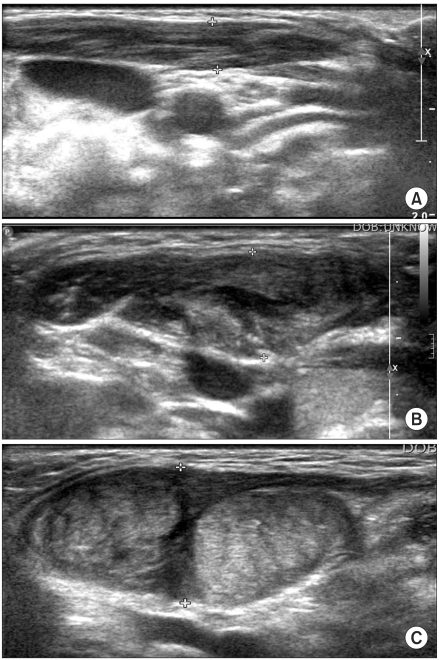 | Fig. 1Ultrasonographic grading of congenital muscular torticollis. (A) Grade 1 was defined when the thickness of involved SCM muscle was increased compared to the normal side. (B) Grade 2 was defined when well-demarcated heteroechoic region was observed. (C) Grade 3 was defined when diffuse hyperechoic fibrous mass was observed. 
|
DDH diagnosis and classification were based on hip US and physical examination findings. When performing the examination, we looked for limitation of abduction in the hip joint. The Ortolani and Barlow test was used for physical examination of the hip. All patients were screened for DDH with hip US. When hip US was performed, α angle and Graf classification were documented.
16 Graf classification type 1 was defined when US finding showed a normal form and structure; type 2, a dysplasia of the acetabulum; type 3, decentration of femoral head; and type 4, complete luxation of femoral head.
All patients with DDH were followed up by serial hip US after six months from initial US evaluation. All ultrasound scanning for neck and hip was performed by the same experienced sonographer. Birth history (breech presentation and oligohydramnios), sex and side of CMT or DDH were examined as potential risk factors to determine the coexistence rate of DDH and CMT.
Statistical analysis was performed using MedCal software (Mariakerke, Belgium). Logistic regression test was used and p-values of 0.05 or less were considered statistically significant.
Go to :

RESULTS
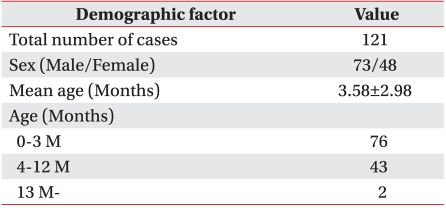
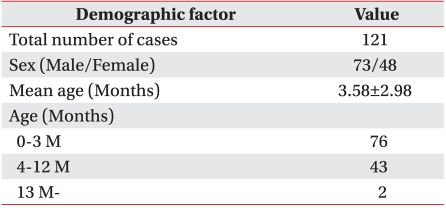
One hundred and twenty-one patients were identified as having CMT. Out of 73 male (60.3%) and 48 female (39.7%), 76 patients were seen within 3 months of life, 43 were between 4 and 12 months, and 2 were older than 12 months at presentation (mean age: 3.58 months, SD: 2.98 months). Eighteen patients (14.9%) were noted to have DDH on hip US including 9 males and 9 females. A sex difference was not observed (
Table 1).
Table 1
Demographic Factors of Patients Enrolled in This Study

Most DDH cases were spontaneously resolved at follow-up examination, and only 2 patients (1.7%) needed to be treated with Pavlik harness. Graf classification of patients treated with Pavlik harness was IIb. Positive predictive value (numbers of positive in physical examination and hip US/numbers of positive in physical examination×100) of clinical examination for DDH was 52.6% and patients treated by harness were all clinically positive. No false negative cases were observed in the negative physical examination (
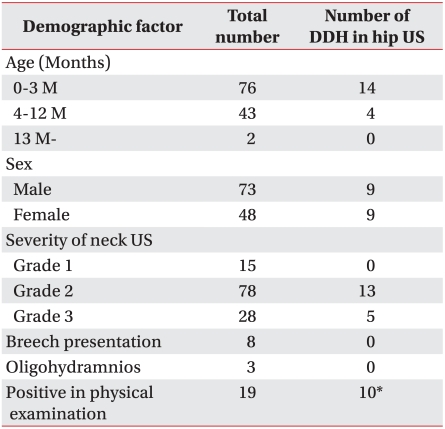
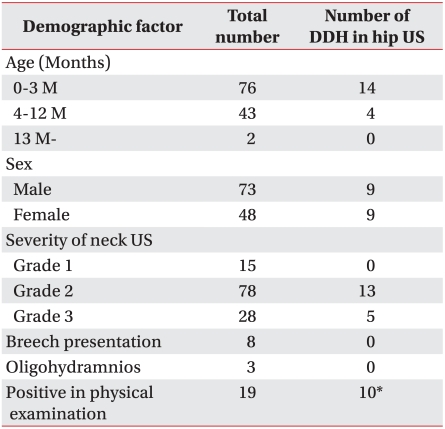
Table 2).
Table 2
Comparison of Clinical Characteristics in Total Case and Case of Positive Hip US

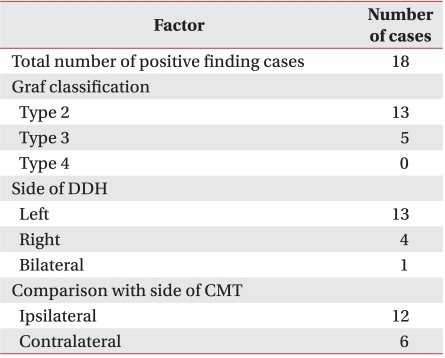
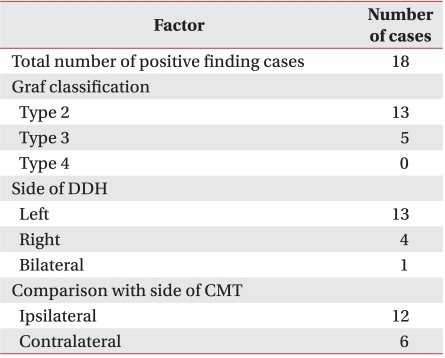
Of the 18 patients who were diagnosed with DDH in the hip US, 13 (72.2%) was identified as type 2 by Graf classification, and 5 (27.8%) as type 3. Five patients whose Graf classification was type 3 were all clinically positive, and 2 of them were treated by harness. DDH was more common in the left side (13 left, 4 right, 1 bilateral), and 6 out of 18 DDH (33.3%) presented on the contralateral side of CMT. No correlation was observed between the side of CMT and DDH (
Table 3).
Table 3
Hip US Data Obtained from Patients in This Study

Of the 121 patients, 8 (6.6%) had breech presentation listed, and 3 (2.4%) had oligohydramnios. Of the 18 patients who were diagnosed with DDH in the hip US, none had a history of breech presentation or oligohydramnios. Therefore, breech presentation and oligohydramnios were not related to DDH occurrence (
Table 2).
Of the 18 patients who were diagnosed with DDH in the hip US, the mean thickness ratio was 2.26. In the group of the other patients, the mean thickness ratio was 2.14. Out of 121 patients, 15 (12.4%) was identified as grade 1 on neck US, 78 (64.5%) as grade 2, and 28 (23.1%) as grade 3. Of the 18 patients who were diagnosed with DDH in the hip US, 13 (72.2%) were identified as grade 2 on neck US, and 5 (27.8%) as grade 3. The thickness ratio of neck muscle and grade of neck US did not correlate with DDH occurrence (
Table 3).
Go to :

DISCUSSION
The association of CMT and DDH has been established through many studies
1,
5-
9 and is widely accepted. Given this association, diagnosis of one of the disorders initiates an investigation for the other. Because CMT is clinically apparent, it most often leads to the evaluation of DDH. DDH is an important term because it accurately reflects the biologic features of the disorder and the susceptibility of the hip to become dislocated at various times. Early detection of DDH enables more effective treatment. Therefore, a screening test for the detection of DDH was attempted with various methods. In recent years, hip US has been recommended as a tool in early diagnosis of DDH in infants. However, it is inevitable that the families and medical establishment have to incur an unnecessary expense, while hip US is oversensitive to diagnose hip abnormalities that have been resolved spontaneously and need no medical treatment. Therefore, we evaluated how many patients diagnosed with DDH in the hip US had to be medically treated, and considered whether physical examination could be the diagnostic tool instead of the hip US.
Factors associated with DDH include ligamentous laxity, pre- and post-natal positioning, as well as genetic and environmental factors. In particular, conditions such as CMT, oligohydramnios or breech presentation predispose to DDH.
4,
17-
19 Therefore, current clinical guidelines
4 recommend conducting routine hip imaging screening tests in the case of female infants
20 with either positive familial history of DDH or history of breech presentation because of the significant risk for DDH. However, there is no consensus on routine hip imaging screening for patients with CMT.
The most important result from our study is that most of the 18 patients who were diagnosed with DDH in the hip US were spontaneously resolved at follow-up examination, and only 2 patients needed to be treated with Pavlik harness, and were all clinically positive on physical examination. The results of our study show that US of the hip should not be recommended routinely as a screening tool for those patients with CMT.
In 2001, a similar study was reported by Y.C. Tien at al.
21 From the results of their ultrasonographic study, the coexistence rate between CMT and DDH was concluded to be 17%, and if only those hip dysplasias that required treatment were included, the coexistence rate of these two disorders would be lowered to 8.5%. Owing to these results, hip US was recommended routinely for those patients with CMT. However, they only investigated the value of hip US as a screening test in DDH without consideration of whether the physical examination of the hip was enough as a screening test in DDH. Therefore, in spite of a similar coexistence rate between CMT and DDH to the rate observed by us, they adopted a completely opposite stance about the values of US hip as screening tool.
Another study showed that an 8% incidence rate of DDH in a group of 70 patients with CMT was found, and they decided that routine history and physical examination are sufficient for the identification of DDH in children with CMT.
22 However, they did not examine the rate at which hip US proven cases of DDH go on to develop CMT, while they performed hip physical examination in all patients with CMT clinically. Therefore, their results can be distinguished from our study.
We concluded that hip US should not be recommended as a routine test for patients with CMT. In addition, we investigated the indication for hip US as a screening test in infants with CMT, such as female sex, breech presentation, history of oligohydramnios and severity of CMT. However, this study provides no evidence that these risk factors significantly increase the rate of DDH in patients with CMT.
A number of reports have mentioned that well-known risk factors for DDH include female sex, breech presentation, history of oligohydramnios, side of CMT or DDH and other associated factors. However, the assessment for these risk factors was limited in our study, because we evaluated risk factors that were only recorded precisely enough to be comparable.
Our study also has limitations because the clinical examination of hip and interpretation of US findings were described subjectively and the results can be different depending on experience of the examiner.
Compared with previous studies that reviewed charts and records of patients with CMT retrospectively, this study was meaningful because we investigated the coexistence rate of two disorders prospectively by performing hip US in all patients with CMT for the first time.
Go to :

CONCLUSION
We concluded that, despite the association of CMT and DDH, a patient presenting with CMT does not require routine hip US screening test, excluding the case of abnormal clinical hip examination. In other words, hip US should be checked after confirming abnormal clinical findings of the hip in CMT patients.
Go to :

ACKNOWLEDGEMENTS
This work was supported by clinical research grant from Pusan National University Hospital (2009).
Go to :

References
1. Cheng JC, Au AW. Infantile torticollis: a review of 624 cases. J Pediatr Orthop. 1994; 14:802–808. PMID:
7814599.
2. Coventry MB, Harris LE. Congenital muscular torticollis in infancy; some observations regarding treatment. J Bone Joint Surg Am. 1959; 41-A:815–822. PMID:
13664717.
3. Suzuki S, Yamamuro T, Fujita A. The aetiological relationship between congenital torticollis and obstetrical paralysis. Int Orthop. 1984; 8:175–181. PMID:
6530313.

4. American Academy of Pediatrics. Clinical practice guideline: early detection of development dysplasia of the hip. Pediatrics. 2000; 105:896–905. PMID:
10742345.
5. Canale ST, Griffin DW, Hubbard CN. Congenital muscular torticollis. A long-term follow-up. J Bone Joint Surg Am. 1982; 64:810–816. PMID:
7085709.

6. Iwahara T, Ikeda A. On the ipsilateral involvement of congenital muscular torticollis and congenital dysplasia of the hip. J Jpn Orthop Assoc. 1962; 35:23–28.
7. Hummer CD, MacEwen GD. The coexistence of torticollis and congenital dysplasia of the hip. J Bone Joint Surg Am. 1972; 54:1255–1256. PMID:
4652057.

8. Ippolito E, Tudisco C, Massobrio M. Long-term results of open sternocleidomastoid tenotomy for idiopathic muscular torticollis. J Bone Joint Surg Am. 1985; 67:30–38. PMID:
3968102.

9. Binder H, Eng GD, Gaiser JF, Koch B. Congenital muscular torticollis: results of conservative management with long-term follow-up in 85 cases. Arch Phys Med Rehabil. 1987; 68:222–225. PMID:
3566514.
10. Chan YL, Cheng JC, Metreweli C. Ultrasonography of congenital muscular torticollis. Pediatr Radiol. 1992; 22:356–360. PMID:
1408445.

11. Lin JN, Chou ML. Ul t rasonographic study of thesternocleidomastoid muscle in the management of congenital muscular torticollis. J Pediatr Surg. 1997; 32:1648–1651. PMID:
9396548.
12. Graf R. Fundamentals of sonographic diagnosis of infant hip dysplasia. J Pediatr Orthop. 1984; 4:735–740. PMID:
6392336.

13. Harcke HT. Imaging in congenital dislocation and dysplasia of the hip. Clin Orthop Relat Res. 1992; 281:22–28. PMID:
1499216.

14. Kim SJ, Park EM, Choi WK, Seo KS, Yoon JS, Lee EH. The correlation between outcome and ultrasonographic findings in congenital muscular torticollis. J Korean Acad Rehabil Med. 2001; 25:601–608.
15. Hsu TC, Wang CL, Wong MK, Hsu KH, Tang FT, Chen HT. Correlation of clinical and ultrasonographic features in congenital muscular torticollis. Arch Phys Med Rehabil. 1999; 80:637–641. PMID:
10378488.

16. Graf R. Classification of hip joint dysplasia by means of sonography. Arch Orthop Trauma Surg. 1984; 102:248–255. PMID:
6712426.

17. Dunn PM. Perinatal observations on the etiology of congenital dislocations of the hip. Clin Orthop Relat Res. 1976; 119:11–22. PMID:
954299.
18. Davids JR, Wenger DR, Mubarak SJ. Congenital muscular torticolis: sequel of intrauterine or perinatal compartment syndrome. J Pediatr Orthop. 1993; 13:141–147. PMID:
8459000.
19. Sherer DM. Spontaneous torticollis in a breech-presenting fetus delivered by an atraumatic elective cesarean section: a case and review of the literature. Am J Perinatol. 1996; 13:305–307. PMID:
8863951.

20. Lehmann HP, Hinton R, Morello P, Santoli J. Developmental dysplasia of the hip practice guideline: technical report. Committee on Quality Improvement, and Subcommettee on Developmental Dysplasia of the Hip. Pediatrics. 2000; 105:E57. PMID:
10742378.
21. Tien YC, Su JY, Lin GT, Lin SY. Ultrasonographic study of the coexistence of muscular torticollis and dysplasia of the hip. J Pediatr Orthop. 2001; 21:343–347. PMID:
11371818.

22. Walsh JJ, Morrissy RT. Torticollis and hip dislocation. J Pediatr Orthop. 1998; 18:219–221. PMID:
9531405.

Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download