1. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Sanelli JT, Freeman ED, Slaten WK, Rao S. Fluoroscopically guided lumbar transforaminal epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehabil. 2002; 81:898–905. PMID:
12447088.
2. Slipman CW, Chow DW. Therapeutic spinal corticosteroid injections for the management of radicu lopathies. Phys Med Rehabil Clin N Am. 2002; 13:697–711. PMID:
12380554.
3. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine. 2002; 27:11–16. PMID:
11805628.
4. Bogduk N. Clinical anatomy of the lumbar spine and sacrum. 2005. 4th ed. New York: Churchill Living stone;p. 123–124.
5. Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: report of three cases. Spine J. 2002; 2:70–75. PMID:
14588291.
6. Somayaji HS, Saifuddin A, Casey AT, Briggs TW. Spinal cord infarction following therapeutic computed tomography-guided left L2 nerve root injection. Spine (Phila Pa 1976). 2005; 30:E106–E108. PMID:
15706327.

7. Stretanski MF, Chopko B. Unintentional vascular uptake in fluoroscopically guided, contrast confirmed spinal injections: a 1-yr clinical experience and discussion of findings. Am J Phys Med Rehabil. 2005; 84:30–35. PMID:
15632486.
8. Jasper JF. Lumbar retrodiscal transforaminal injection. Pain Physician. 2007; 10:501–510. PMID:
17525785.

9. Lee IS, Kim SH, Lee JW, Hong SH, Choi JY, Kang HS, Song JW, Kwon AK. Comparison of the temporary diagnostic relief of transforaminal epidural ste roid injection approaches: conventional versus posterolateral technique. AJNR Am J Neuroradiol. 2007; 28:204–208. PMID:
17296980.
10. Lew HL, Coelho P, Chou LH. Preganglionic approach to transforaminal epidural steroid injections. Am J Phys Med Rehabil. 2004; 83:378. PMID:
15100628.

11. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Freeman TL, Slaten WK. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil. 2000; 81:1045–1050. PMID:
10943753.

12. Sullivan WJ, Willick SE, Chira-Adisai W, Zuhosky J, Tyburski M, Dreyfuss P, Prather H, Press JM. Incidence of intravascular uptake in lumbar spinal injec tion procedures. Spine. 2000; 25:481–486. PMID:
10707395.
13. Furman MB, O'Brien EM, Zgleszewski TM. Incidence of intravascular penetrati on in transforaminal lumbosacral epidural steroid injections. Spine. 2000; 25:2628–2632. PMID:
11034648.
14. Furman MB, Giovanniello MT, O'Brien EM. Incidence of intravascular penet ration in transforaminal cervical epidural steroid injections. Spine. 2003; 28:21–25. PMID:
12544950.
15. Smuck M, Fuller BJ, Yoder B, Huerta J. Incidence of simultaneous epidural and vascular injection during lumbosacral transforaminal epidural injections. Spine J. 2007; 7:79–82. PMID:
17197337.

16. Derby R, Lee SH, Kim BJ, Chen Y, Seo KS. Complications following cervical epidural steroid injections by expert interventionalists in 2003. Pain Physician. 2004; 7:445–449. PMID:
16858486.
17. Alleyne CH Jr, Cawley CM, Shengelaia GG, Barrow DL. Microsurgical anatomy of the artery of Adamkiewicz and its segmental artery. J Neurosurg. 1998; 89:791–795. PMID:
9817417.

18. Burn JM, Langdon L. Lumbar epidural injection for the treatment of chronic sciatica. Rheumatol Phys Med. 1970; 10:368–374. PMID:
5458848.

19. Snoek W, Weber H, Jorgensen B. Double blind evaluation of extradural methyl prednisolone for herniated lumbar discs. Acta Orthop Scand. 1977; 48:635–641. PMID:
343479.

20. Cohen SP, Maine DN, Shockey SM, Kudchadkar S, Griffith S. Inadvertent disk injection during transforaminal epidural steroid injection: steps for prevention and management. Pain Med. 2008; 9:688–694. PMID:
18657222.

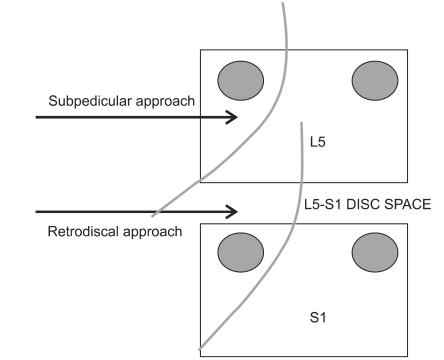
21. In : Kim C, Choi HE, Kang SH, Lim MH, editors. The contrast spreading pattern in the retrodiscal approach for transforaminal epidural block. 2010. The 38th Annual Conference of the Korean Academy of Rehabilitation Medicine; 2010 Oct 21-23; Seoul, Korea. Seoul: Medrang.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download