This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To investigate the reliability of inspection-based classification of sagittal gait patterns in children with bilateral spastic cerebral palsy (CP).
Method
Video clip recordings of gait patterns and sagittal kinematic data obtained by a computerized motion analysis system from 91 patients with bilateral spastic CP were reviewed. The abnormal gait patterns were classified into 4 groups using the method described by Rodda et al. Visual observation-based classification (visual classification) was compared with classification by 3D analysis-based methods (3D classification). The reliabilities of visual classifications made by an experienced physician and a trainee physician were analyzed.
Results
The consistency of inspection-based gait classification using kinematic data analysis was demonstrated by an experienced physician (Kappa coefficient (k)=0.67, p<0.001). However, the consistency was low for the trainee physician (k=0.37, p<0.001). Group III (apparent equinus) was commonly confused with group IV (crouch gait) by the trainee physician, resulting in lower agreement for those two evaluation groups than for other patterns. Video observation showed low reliability in comparisons made between the experienced and the trainee physician (k=0.37, p<0.001).
Conclusion
There was substantial agreement of gait classification between video observation and kinematic data analysis by the experienced physician, but not by the trainee physician. Low reliability was also demonstrated for inspection-based gait classification.
Go to :

Keywords: Spastic diplegia, Gait, Observation, Reliability
INTRODUCTION
Patients with bilateral spastic cerebral palsy (CP) tend to show abnormal gait due to spasticity, muscle weakness, abnormal muscle coordination, and the ensuing muscle shortening and bone deformity. The abnormal gait is observed in a wide variety of patterns depending on the severity of such disorders.
1,
2
Using computerized three-dimensional (3D) motion analysis, it has been possible to identify the similarities and differences of abnormal gait patterns in patients with CP. There have been many efforts to categorize their abnormal gait patterns. O'Byrne et al.
3 and Kienast et al.,
4 who conducted cluster analyses, suggested 8 and 3 categories, respectively. Rodda et al.
5 suggested 4 categories of sagittal gait patterns based on the 3D gait analysis in patients with bilateral spastic CP.
It is clinically crucial to classify gait patterns into several categories, because the classification makes it possible to explain the causes of gait abnormality in each category. This elucidates the muscles whose spasticity should be managed, which should be lengthened, and which should be braced for improving gait patterns, and this permits standardization of the therapeutic process.
6,
7 In addition, healthcare providers such as doctors and therapists do not need to explain the gait patterns in detail, but have only to categorize the abnormal gait patterns, which permits them to communicate accurately and objectively analyze the outcome of treatment.
8,
9 In particular, categorization has the merit of enabling healthcare providers to observe patients' gaits or to easily video-record gaits without using a high-priced computer-aided analyzer, which is helpful for making clinical decisions.
10
Given such advantages however, not much is known about whether visual analyses have been consistent with 3D gait analyses in regarding categorization, and whether different raters reach the same conclusions. For this reason, this study was conducted to analyze the consistency between visual observation-based classification (visual classification) and 3D analysis-based classification (3D classification) when using the classification suggested by Rodda et al.,
5,
11 as well as to analyze the reliability between different raters in visual classifications.
Go to :

MATERIALS AND METHODS
Subjects
The subjects included 91 patients with bilateral spastic CP who underwent gait analysis in the motion analysis laboratory of the present hospital between September 2008 and May 2009.
Methods
Gait analysis was performed using a computerized gait analysis system (VICON 370 Motion Analysis System with 6 infrared cameras, Oxford Metrics Inc., Oxford, UK) to measure the kinematic data (angle of each joint) during the gait cycle. A trained investigator placed 13 reflective markers on the first sacrum, the anterior superior iliac spine, the mid points of the lateral femur, the lateral knee joint axis, the midpoints of the lateral tibia, the lateral malleolus, and the dorsal foot between metatarsal heads 2 and 3. All subjects walked barefoot at a self-determined speed along an 8-meter path with the markers in place. Force-plates (AMTI OR 6-5, Advanced Mechanical Technology, Newton, MA, USA) under the path recorded ground reaction forces during the walking trials with a 480-Hz sampling frequency, and joint moments were expressed as internal moments to counter the ground reaction force. Data collection continued until the subject achieved at least 3 'clean' force-plate strikes. Kinematic data from successful trials were averaged and the averaged data were used for statistical analysis.
8 Video recording was done simultaneously from the front, rear, and side, with the 3D gait analysis.
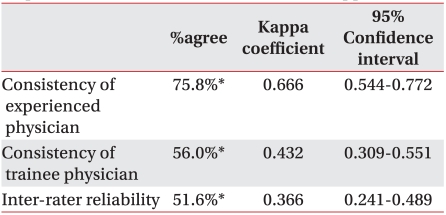
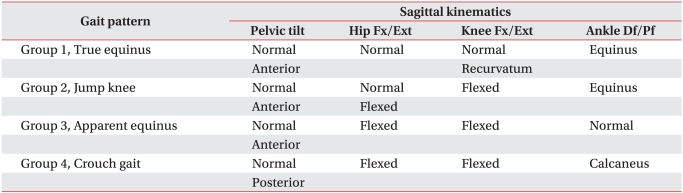
Sagittal gait abnormalities in patients with bilateral spastic CP were categorized using Rodda's classification
5 described as follows: The 1st group was defined as true equinus. The ankle is in equinus. The knee extends fully or goes into mild recurvatum. The hip extends fully and the pelvis is within the normal range or tilted anterior. The 2nd group was defined as jump gait. The ankle is in equinus, particularly in late stance. The knee and hip are excessively flexed in early stance and then extend to a variable degree in late stance, but never reach full extension. The pelvis is either within the normal range or tilted anterior. In this group, equinus is caused by the contracture or spasticity of the triceps surae muscle, the flexion of the knee joint and the hip joint caused by the contracture or spasticity of the hamstring and the hip joint flexor muscle, and the increased anterior tilt of the pelvis. Also, in cases where the rectus femoris muscle becomes spastic or shortened, it is accompanied by stiff knee gait during the swing phase. The 3rd group was defined as apparent equinus. The ankle has a normal range, but the knee and hip are excessively flexed throughout stance. The pelvis is normal or tilted anterior. In this group, the proximal knee joint shows much more exion during the stance phase and thus subjects tend to walk on tiptoe, but in the gait analysis, the dorsiflexion of the ankle joint is comparatively normal. In the gait analysis, the ankle joint shows comparatively normal dorsiflexion. The 4th group was defined as crouch gait. The ankle is excessively dorsiflexed throughout stance, and the knee and hip are excessively flexed. The pelvis is in the normal range or tilted posterior. This case is easily observed in patients with severe bilateral spastic CP (
Fig. 1,
Table 1).
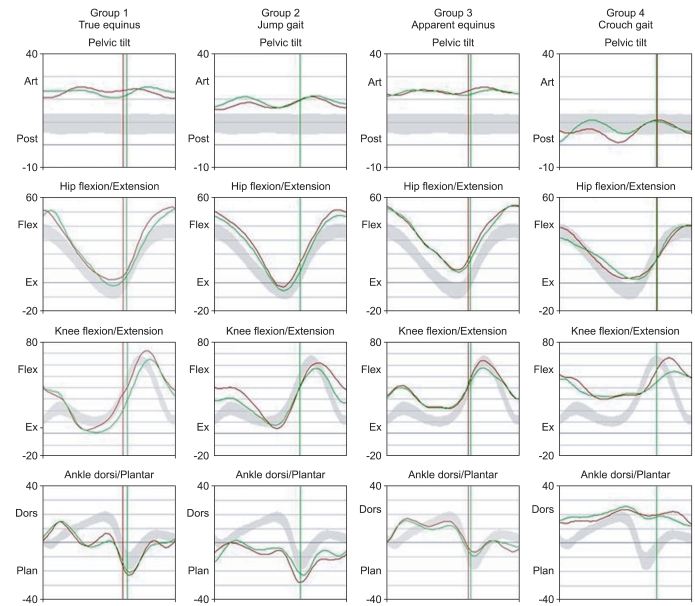 | Fig. 1Saggital plane kinematic data for gait patterns. Examples of sagittal plane kinematic data for each gait pattern (Green line for right leg and red line for left leg). Light gray band represents the mean±1 standard deviation of kinematic data from our laboratory's normal database. Vertical axis represents angular displacement of joint and the horizontal axis represents the timeline of single gait cycle. Group 1 (True equinus): The ankle is in equinus. The knee extends fully or goes into mild recurvatum. The hip extends fully and the pelvis is within the normal range or tilted anterior. Group 2 (Jump gait): The ankle is in equinus, particularly in late stance. The knee and hip are excessively flexed in early stance and then extend to a variable degree in late stance, but never reach full extension. The pelvis is either within the normal range or tilted anterior. Group 3 (Apparent equinus): The ankle has a normal range but the knee and hip are excessively flexed throughout stance. The pelvis is normal or tilted anterior. Group 4 (Crouch gait): The ankle is excessively dorsiflexed throughout stance and the knee and hip are excessively flexed. The pelvis is in the normal range or tilted posterior. 5

|
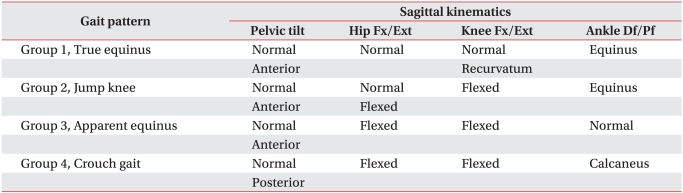
Table 1
The Definition of the Gait Classification at Each Level

Kinematic data and video-recordings of gait pattern were retrospectively analyzed by 2 raters. One of the raters was a specialist in pediatric rehabilitation who had 5-years of clinical experience (an experienced rater), and was accustomed to applying the Rodda's classification and the computerized 3D motion analysis. The other rater was a resident in pediatric rehabilitation (a trainee rater), who had little experience in using Rodda's classification, but was fully trained for it prior to data analysis. The results of computerized 3D motion analysis were analyzed by the experienced rater in accordance with Rodda's classification. For visual classification, the experienced rater and the trainee rater watched the videos of subjects' gait patterns and individually categorized them in accordance with Rodda's classification.
Analytical methods
The 'Statistical Package for the Social Sciences (SPSS; version 18.0)' was used to analyze data. The validity of classification and the inter-rater reliability were analyzed using Kappa coefficients (k). A high consistency was defined as a Kappa coefficient ≥0.8 and a moderate consistency when it was ≥0.6 but <0.8. A low consistency was defined as a Kappa coefficient <0.6.
12
Go to :

RESULTS
The 91 subjects consisted of 61 men and 30 women. Twenty-one (23%), 52 (58%), and 18 (19%) of the subjects were classified as level 1, level 2, and level 3, respectively on the basis of the Gross Motor Function Classification System (GMFCS). Their average age was 10.4±6.3 years (range, 4-34 years). The experienced rater classified subjects into 4 groups using the computerized 3D gait analysis; the average age of the 1st group was 7.6±2.5; the 2nd group, 3rd group and 4th group were 11.1±8.8, 10.4±6.3, and 14.2±4.3, respectively.
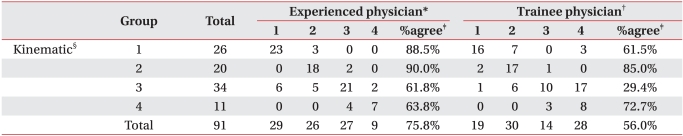
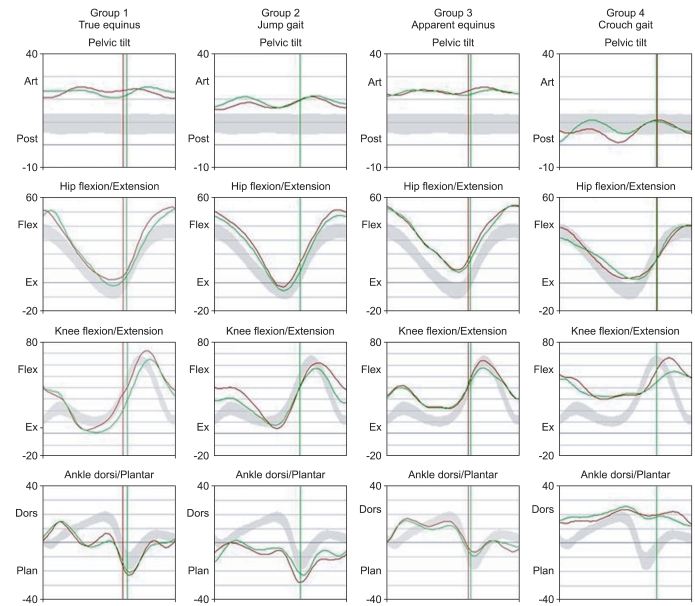
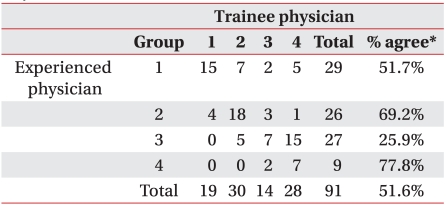
A comparative analysis was made of the consistency between the visual classification, given by the experienced rater and the trainee rater individually, and the experienced rater's 3D gait analysis. The mean consistency of the experienced rater's visual classification reached 75.8%. The consistencies of the 4 groups were 88.5%, 90.0%, 61.8%, and 63.6% respectively; the 1st group and the 2nd group showed high consistencies, but the other 2 groups showed moderate consistencies. The mean consistency of the trainee rater's visual classification reached 56.0%. The 4 groups indicated 61.5%, 85.0%, 29.4%, and 72.7% respectively; the 2nd group and the 4th group showed high consistencies, but the 1st group and the 3rd group showed a moderate consistency and a low consistency, respectively. In both testers' results, the 2nd group showed a high consistency, but the 3rd group showed a comparatively low consistency (
Table 2).
Table 2
Consistency of Inspection-based Gait Classification by Experienced and Trainee Physicians

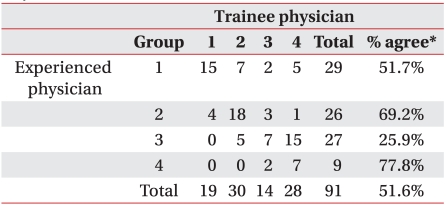
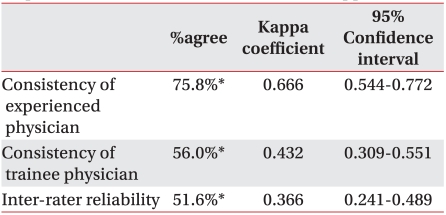
The inter-rater consistency of visual classification averaged 51.6%. The 4 groups indicated 51.7%, 69.2%, 25.9%, and 77.8% respectively; the 4th group showed a high consistency, but the 1st group and the 2nd group showed moderate consistencies. The 3rd group showed a low consistency (
Table 3).
Table 3
Reliability of Inspection-based Gait Classification Compared between Experienced and Trainee Physicians

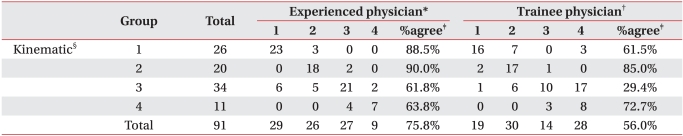
As mentioned above, Kappa coefficients were used to analyze the consistency between 3D classification and visual classification. The experienced rater demonstrated a moderate consistency (k=0.667), but the trainee rater demonstrated a low consistency (k=0.432). The inter-rater consistency was low for visual classification (k=0.366) (
Table 4).
Table 4
Consistency and Inter-observer Reliability for Inspection-based Gait Classification with Kappa Statistics

Go to :

DISCUSSION
In patients with bilateral spastic CP, sagittal gait abnormalities are observed which vary depending on joint and bone deformities and the degree of spasticity.
5 In 1986, Rang et al.
13 classified the gait patterns of patients with bilateral spastic CP, based on sagittal observations. They explained the interconnection between the psoas muscle and lumbar lordosis; the hip joint adductor muscle and scissoring gait; the hamstring muscle and the flexion of the knee joint; the rectus femoris muscle and stiff-legged gait; the triceps surae muscle and equinus gait, and suggested therapeutic guidelines based on the contracture of specific muscles. Rodda et al.
5 classified the gait patterns of patients with bilateral spastic CP into 4 categories, referring to the sagittal location of the ankle joint, the knee joint and the hip joint, and suggested cases where assist devices should be applied, where botulinum toxin should be injected, and where muscles should be lengthened. For reference, this study adopted their classification.
The classification of gait patterns has the merit of standardizing treatments, and also enabling healthcare providers to classify gait patterns without high-priced computer-aided analyzers. Therefore, the first consideration is to prove whether visual observation is consistent with 3D gait analysis for classification. By using the classification, healthcare providers do not need explain gait patterns in detail, but have only to categorize them, which makes it possible for them to have accurate communications with each other; but this system requires consistency between raters. In addition, such a classification provides simple and clear definitions of abnormal gait patterns, which enables even inexperienced raters to provide a comparatively accurate classification. Thus, the second consideration is to confirm the reliability between experienced raters and inexperienced raters.
In this study, the consistency between visual classification and 3D classification given by an experienced rater was analyzed (
Table 2). In the case of the experienced rater, the consistency was lower in the 3rd group and the 4th group than in the 1st group and the 2nd group. In the 3rd group, equinus gait was observed due to the excessive flexion of the hip joint and the knee joint, though the ankle showed the comparatively normal dorsiflexion. However, it is not easy for the visual observation to check whether plantar flexion has increased in the ankle. Actually, in this study, subjects to be classified as the 3rd group were wrongly classified as the 1st or 2nd group. Moreover, valgus deformity tends to increase, and the ankle tends to be dorsiflexed as patients grow older. Such being the case, it is easy to classify those subjects as the 4th group when their equinus gaits are not clearly observed, and an inexperienced rater is especially apt to make such mistakes. A previous study
5 reported that subjects in the 1st group and the 2nd group were on average younger than those in the 3rd group and the 4th group. Also, the 1st group had the youngest subjects (average, 7.6 years), followed by the 2nd group (11.1 years), the 3rd group (10.8 years), and the 4th group (14.1 years), which implies that gait abnormalities may change as patients grow older. This also presents the possibility of a transition phase that makes it difficult to accurately classify gait abnormalities.
14 In a previous study that conducted a cluster analysis with the results of 3D gait analyses.
9 the 1st group and the 4th group showed clearly different gait patterns and distinct characteristics, but the 2nd group and the 3rd group were not significantly distinguished from other groups.
For verifying inter-rater reliability of visual classification, an analysis was made of the consistency between visual classifications given by the experienced rater and the trainee rater individually (
Table 2). The result showed that the inter-rater consistency was lower in the 3rd group in comparison with other groups; especially, there were many cases where subjects classified as the 3rd group by the experienced rater, were reclassified as the 4th group by the trainee rater. Likewise, Rodda et al.
5 evaluated intra-rater and inter-rater reliabilities by referring to visual observations and 3D gait analyses simultaneously; generally, the groups showed high intra-rater reliabilities, but the 3rd group showed a low reliability.
In summary, the experienced rater demonstrated a moderate consistency between visual classification and 3D classification. On the other hand, the trainee rater demonstrated low values not only for consistency but also for inter-rater reliability (
Table 4). Therefore, though visual observation-based classification has many merits, the results of this study cast a doubt on its accuracy. However, such errors can be corrected by physical examinations; to be specific, physical examinations make it possible to check how much the ankle plantarflexor muscle, the hamstring, and the psoas muscle have been shortened and thus reduce errors where subjects to be classified as the 3rd group are wrongly classified as the 1st or 2nd or 4th group. Therefore, a further study needs to be conducted to ascertain whether a combination of visual observations and physical examinations can improve the reliability of classification.
Go to :

CONCLUSION
In conjunction with the gait patterns of 91 patients with bilateral spastic CP, a comparison was made between visual observation-based classification and 3D gait analysis-based classification. In addition, analyses were made of the consistency between the two classifications and reliability between an experienced rater and a trainee rater. As for the consistency, the experienced rater demonstrated high consistencies in the 1st group and the 2nd group, but moderate consistencies in the 3rd group and the 4th group. The trainee rater demonstrated a particularly low consistency in the 3rd group. As for the inter-rater reliability, the consistency was low in the 3rd group. In particular, there were many cases where the trainee rater incorrectly classified subjects who should have been classified as the 3rd group, but rather were classified as the 4th group.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download