1. Dimopoulos IS, Radziwon A, St Laurent CD, MacDonald IM. Choroideremia. Curr Opin Ophthalmol. 2017; 28(5):410–415. PMID:
28520608.

2. Coussa RG, Traboulsi EI. Choroideremia: a review of general findings and pathogenesis. Ophthalmic Genet. 2012; 33(2):57–65. PMID:
22017263.

3. MacDonald IM, Binczyk N, Radziwon A, Dimopoulos I. Choroideremia. Cheung G, editor. Hereditary Chorioretinal Disorders. Singapore: Springer Nature Singapore Pte Ltd;2020. p. 99–106.
4. Jacobson SG, Cideciyan AV, Sumaroka A, Aleman TS, Schwartz SB, Windsor EA, et al. Remodeling of the human retina in choroideremia: Rab escort protein 1 (
REP-1) mutations. Invest Ophthalmol Vis Sci. 2006; 47(9):4113–4120. PMID:
16936131.
5. MacDonald IM, Sereda C, McTaggart K, Mah D. Choroideremia gene testing. Expert Rev Mol Diagn. 2004; 4(4):478–484. PMID:
15225095.

6. Goody RS, Rak A, Alexandrov K. The structural and mechanistic basis for recycling of Rab proteins between membrane compartments. Cell Mol Life Sci. 2005; 62(15):1657–1670. PMID:
15924270.

7. Pereira-Leal JB, Hume AN, Seabra MC. Prenylation of Rab GTPases: molecular mechanisms and involvement in genetic disease. FEBS Lett. 2001; 498(2-3):197–200. PMID:
11412856.

8. Battu R, Jeyabalan N, Murthy P, Reddy KS, Schouten JS, Webers CA. Genetic analysis and clinical phenotype of two Indian families with X-linked choroideremia. Indian J Ophthalmol. 2016; 64(12):924–929. PMID:
28112135.

9. Wu AL, Wang JP, Tseng YJ, Liu L, Kang YC, Chen KJ, et al. Multimodal imaging of mosaic retinopathy in carriers of hereditary X-linked recessive diseases. Retina. 2018; 38(5):1047–1057. PMID:
28376043.

10. Rodrigues MM, Ballintine EJ, Wiggert BN, Lee L, Fletcher RT, Chader GJ. Choroideremia: a clinical, electron microscopic, and biochemical report. Ophthalmology. 1984; 91(7):873–883. PMID:
6089068.
11. Mitsios A, Dubis AM, Moosajee M. Choroideremia: from genetic and clinical phenotyping to gene therapy and future treatments. Ther Adv Ophthalmol. 2018; 10:2515841418817490. PMID:
30627697.

12. Krill AE, Archer D. Classification of the choroidal atrophies. Am J Ophthalmol. 1971; 72(3):562–585. PMID:
5315093.

13. Lee TK, McTaggart KE, Sieving PA, Heckenlively JR, Levin AV, Greenberg J, et al. Clinical diagnoses that overlap with choroideremia. Can J Ophthalmol. 2003; 38(5):364–372. PMID:
12956277.

14. Gao FJ, Tian GH, Hu FY, Wang DD, Li JK, Chang Q, et al. Next-generation sequencing-based clinical diagnosis of choroideremia and comprehensive mutational and clinical analyses. BMC Ophthalmol. 2020; 20(1):212. PMID:
32487042.

15. Kim MS, Joo K, Seong MW, Kim MJ, Park KH, Park SS, et al. Genetic mutation profiles in Korean patients with inherited retinal diseases. J Korean Med Sci. 2019; 34(21):e161. PMID:
31144483.

16. Ma DJ, Lee HS, Kim K, Choi S, Jang I, Cho SH, et al. Whole-exome sequencing in 168 Korean patients with inherited retinal degeneration. BMC Med Genomics. 2021; 14(1):74. PMID:
33691693.

17. Guo H, Li J, Gao F, Li J, Wu X, Liu Q. Whole-exome sequencing reveals a novel
CHM gene mutation in a family with choroideremia initially diagnosed as retinitis pigmentosa. BMC Ophthalmol. 2015; 15(1):85. PMID:
26216097.

18. MacDonald IM, Russell L, Chan CC. Choroideremia: new findings from ocular pathology and review of recent literature. Surv Ophthalmol. 2009; 54(3):401–407. PMID:
19422966.

19. MacDonald IM, Mah DY, Ho YK, Lewis RA, Seabra MC. A practical diagnostic test for choroideremia. Ophthalmology. 1998; 105(9):1637–1640. PMID:
9754170.

20. Di Iorio V, Esposito G, De Falco F, Boccia R, Fioretti T, Colucci R, et al.
CHM/
REP1 transcript expression and loss of visual function in patients affected by choroideremia. Invest Ophthalmol Vis Sci. 2019; 60(5):1547–1555. PMID:
30995293.
21. Li S, Guan L, Fang S, Jiang H, Xiao X, Yang J, et al. Exome sequencing reveals
CHM mutations in six families with atypical choroideremia initially diagnosed as retinitis pigmentosa. Int J Mol Med. 2014; 34(2):573–577. PMID:
24913019.
22. Bae K, Song JS, Lee C, Kim NK, Park WY, Kim BJ, et al. Identification of pathogenic variants in the
CHM gene in two Korean patients with choroideremia. Ann Lab Med. 2017; 37(5):438–442. PMID:
28643494.
23. Khan KN, Islam F, Moore AT, Michaelides M. Clinical and genetic features of choroideremia in childhood. Ophthalmology. 2016; 123(10):2158–2165. PMID:
27506488.

24. Xue K, Oldani M, Jolly JK, Edwards TL, Groppe M, Downes SM, et al. Correlation of optical coherence tomography and autofluorescence in the outer retina and choroid of patients with choroideremia. Invest Ophthalmol Vis Sci. 2016; 57(8):3674–3684. PMID:
27403996.

25. Heon E, Alabduljalil T, McGuigan DB 3rd, Cideciyan AV, Li S, Chen S, et al. Visual function and central retinal structure in choroideremia. Invest Ophthalmol Vis Sci. 2016; 57(9):OCT377–OCT387. PMID:
27409497.

26. Lazow MA, Hood DC, Ramachandran R, Burke TR, Wang YZ, Greenstein VC, et al. Transition zones between healthy and diseased retina in choroideremia (CHM) and Stargardt disease (STGD) as compared to retinitis pigmentosa (RP). Invest Ophthalmol Vis Sci. 2011; 52(13):9581–9590. PMID:
22076985.

27. Sun LW, Johnson RD, Williams V, Summerfelt P, Dubra A, Weinberg DV, et al. Multimodal imaging of photoreceptor structure in choroideremia. PLoS One. 2016; 11(12):e0167526. PMID:
27936069.

28. Syed R, Sundquist SM, Ratnam K, Zayit-Soudry S, Zhang Y, Crawford JB, et al. High-resolution images of retinal structure in patients with choroideremia. Invest Ophthalmol Vis Sci. 2013; 54(2):950–961. PMID:
23299470.

29. Popović P, Jarc-Vidmar M, Hawlina M. Abnormal fundus autofluorescence in relation to retinal function in patients with retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol. 2005; 243(10):1018–1027. PMID:
15906064.

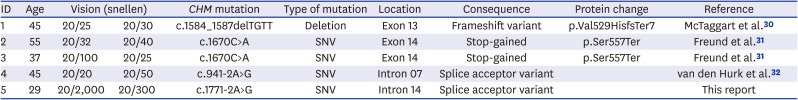
30. McTaggart KE, Tran M, Mah DY, Lai SW, Nesslinger NJ, MacDonald IM. Mutational analysis of patients with the diagnosis of choroideremia. Hum Mutat. 2002; 20(3):189–196. PMID:
12203991.

31. Freund PR, Sergeev YV, MacDonald IM. Analysis of a large choroideremia dataset does not suggest a preference for inclusion of certain genotypes in future trials of gene therapy. Mol Genet Genomic Med. 2016; 4(3):344–358. PMID:
27247961.

32. van den Hurk JA, van de Pol DJ, Wissinger B, van Driel MA, Hoefsloot LH, de Wijs IJ, et al. Novel types of mutation in the choroideremia (
CHM) gene: a full-length L1 insertion and an intronic mutation activating a cryptic exon. Hum Genet. 2003; 113(3):268–275. PMID:
12827496.






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download