INTRODUCTION
The most important component of healthcare resources are the healthcare workers. Healthcare work is labor-intensive compared to other industries, and proper management of healthcare personnel is necessary to maintain and improve the quality of medical services. In particular, systematic management of the health conditions of healthcare workers and medical personnel is important because, in addition to benefiting the individual workers, it affects the safety of patients and the stability of the healthcare system. Recent public health crises, such as the coronavirus disease 2019 pandemic, have highlighted the importance of healthcare workers within the healthcare system.
12 Particularly, these events have demonstrated that good physical and mental health of medical personnel is essential for a well-functioning healthcare system. To address this, specific measures for managing the health of medical personnel are needed.
Despite the importance of good health in healthcare workers, many medical staff experience burnout syndrome in clinical settings. A meta-analysis of data from 45 countries collected between 1991 and 2018 showed that 67% of doctors experience exhaustion.
34 The prevalence of burnout syndrome in medical residents is 51%, and this is higher in Asia (57.2%) and North America (51.6%) than in Europe (27.7%). Further, 11.23% of nurses report exhaustion.
5 Burnout in healthcare providers may interfere with their ability to offer high-quality medical service to patients, and continuous exhaustion may increase the risk for diseases and overwork-related health problems in these workers.
Various studies have examined the occupational factors that influence the health of clinicians. For instance, one study found that the leading cause of death for male doctors in the USA is similar to that of the general population but that the likelihood of death from cerebrovascular disease, transportation accidents, and suicide is higher than that in the general population, so attention was requested to these causes.
6 In Taiwan, doctors report a higher risk for acute myocardial infarction due to the high prevalence of high blood pressure (23.6% vs. 19.1%) and hyperlipidemia (21.4% vs. 13.0%) compared to non-doctors, which requires management.
7 In addition to the USA and Taiwan, studies in Canada and Australia have also used survey tools or health insurance data to identify factors that could improve the welfare of healthcare workers, and correspondingly, the medical system.
8910
In Korea, several studies have examined health status in doctors and nurses. According to a 2005 mortality study of doctors in Korea, the overall mortality rate of doctors is lower than that of the general population but associated drug addiction and suicide are higher,
11 and doctors are more vulnerable to suicide than individuals with other occupations.
12 In a 2016 study of 382 doctors, the prevalence of cancer was more than three times that of the general population. Questions remain as to how doctors should interpret the high prevalence of cancer, as well as the reasons for the increase. The exact cause of this result has yet to be determined, and only a few hypotheses have been considered. This was attributed to specific characteristics of the work environment and routine such as a busy and irregular routine, such as working night shifts, and increased exposure to radioactive materials.
13 Since 2013, the Korean Nursing Health Study (KNHS) has been conducted yearly by the Korean Center for Disease Control and Prevention. The study aims to identify health conditions, lifestyle factors, and disease prevalence via a web-based online survey of nurses working in hospitals, with a focus on the impact of disease outbreaks. However, most of the completed or ongoing studies are cross-sectional, which can make it difficult to compare data between studies. Further, the information produced by these studies is often limited to working conditions and worker satisfaction. In order to evaluate the health status of healthcare workers, long-term and diverse follow-up surveys are required to utilize the appropriate sources of data for a wide range of health assessments.
In this study, we compared the health status of healthcare workers (doctors and nurses) to that of the general population by obtaining major causes of death, mortality, and disease prevalence based on the National Health Insurance Service data and cause-of-death statistics.
METHODS
This study obtained data from the Korea National Health Insurance customized research database. The study subjects were defined as those who underwent at least one general health examination among those who reported to work as doctors and nurses at healthcare institutions from 2002 to 2017. The study selected those registered as doctors and nurses using the Occupational Regulations (INDTP_CD) codes in the qualification database, and extracted workers in healthcare institutions using Occupational Regulations (JICYEK_DTL_CD). In addition, the general health examination was checked in the health examination database. Individuals who worked as both a doctor and nurse at the same time were excluded from the study. We collected the medical usage history of the study subjects included in the treatment database, general health examination results included in the health examination database, disease history, and health behavior data. In addition, the causes of death and mortality of healthcare workers were observed by combining cancer screening data and cause of death data from the National Statistical Office. The variables necessary to identify and track the health levels of healthcare workers were selected, and all variables included data from 2002 to 2017.
To analyze the main cause of death and mortality, data from subjects identified as deceased were extracted from a customized database based on the Korean Standard Classification of Diseases. To compare the mortality of healthcare workers with that of the general population, the number of deaths was extracted and compared according to the major causes of death in the Statistics Korea mortality statistics from 2002 to 2017. Malignant neoplasms were classified in more detail according to their location (C00–C99), and the details of injury, addiction, and death due to external causes were classified according to the impairment mechanism (V01–Y84). Mortality rates were calculated and analyzed using person-years from 2002 to 2017. We also calculated the proportional mortality ratio (PMR) using a log link function and Poisson regression analysis after correcting for gender and age to compare mortality rates between healthcare workers and the general population.
14 PMR refers to the proportion of deaths from a certain disease in the survey group and deaths from the same disease in the standard population when the effects of factors such as age, sex, and so forth are controlled for. Accordingly, PMR in this study was measured as the proportion of deaths due to specific causes in healthcare workers to the proportion of deaths due to the same specific cause in the general population. The 95% confidence interval (CI) was based on the Poisson distribution and Mantel-Haenszel χ
2.
6
We used the mutually exclusive disease classification system used in the Global Burden of Disease (GBD) study conducted by the Institute for Health Indicators to determine prevalence in healthcare workers.
15 The GBD study used 260 disease groups. Here, we used data from patients with diseases from 238 disease groups, excluding ‘other injury’ groups. Malignant neoplasms were classified and analyzed in detail according to the site of occurrence. To calculate prevalence rates, the major classification of disease codes in the 10th International Classification of Diseases was used, and the definitions of a study on disease burden measurement and future prediction in Koreans were used for the disease criteria.
16 In this study, a person who was hospitalized more than once in 2017 or satisfied the number of outpatient treatments for each disease according to criteria in previous studies was defined as a patient. The prevalence rate was calculated by dividing the number of people with a given condition by the population at mid-2017. Then, even if the prevalence of a disease is low, a disease with a high proportion of healthcare workers among the total number of patients can be considered a specific disease of healthcare personnel. Accordingly, the number of healthcare worker patients was compared with the number of patients in the general population. For 238 diseases, the prevalence proportion was calculated using the number of patients in the total population as the denominator and the number of healthcare worker patients as the numerator.
All statistical analyses were conducted using the statistical program SAS 9.4 (SAS Institute, Cary, NC, USA).
Ethics statement
The study was conducted after receiving an exemption from the Research Ethics Review Committee (SEUMC 2019-09-023) of Seoul Hospital, Ewha Womans University.
RESULTS
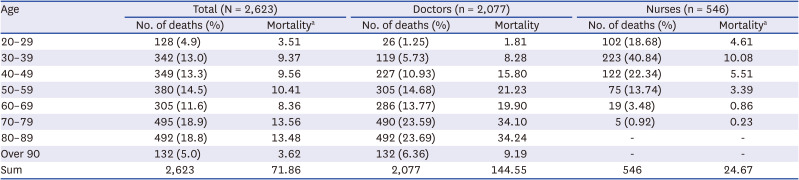
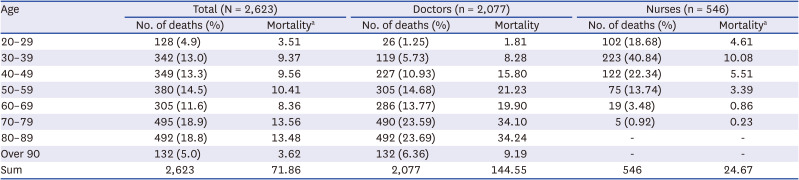
The study included 104,484 doctors and 220,310 nurses. Of these, 2,623 people died during the study period, 2,077 doctors and 546 nurses. Among the total number of healthcare workers who died, the mortality rate of those in their 70s was the highest at 13.56 per 100,000 person-years, and the death rate of those in their 20s was the lowest at 3.51 per 100,000 person-years. Among doctors, those in their 80s had the highest mortality rate, at 34.24 per 100,000 person-years. Among nurses, those in their 30s had the highest mortality rate, at 10.08 per 100,000 person-years (
Table 1).
Table 1
Number of deaths and mortality rate by age of healthcare workers
|
Age |
Total (N = 2,623) |
Doctors (n = 2,077) |
Nurses (n = 546) |
|
No. of deaths (%) |
Mortalitya
|
No. of deaths (%) |
Mortality |
No. of deaths (%) |
Mortalitya
|
|
20–29 |
128 (4.9) |
3.51 |
26 (1.25) |
1.81 |
102 (18.68) |
4.61 |
|
30–39 |
342 (13.0) |
9.37 |
119 (5.73) |
8.28 |
223 (40.84) |
10.08 |
|
40–49 |
349 (13.3) |
9.56 |
227 (10.93) |
15.80 |
122 (22.34) |
5.51 |
|
50–59 |
380 (14.5) |
10.41 |
305 (14.68) |
21.23 |
75 (13.74) |
3.39 |
|
60–69 |
305 (11.6) |
8.36 |
286 (13.77) |
19.90 |
19 (3.48) |
0.86 |
|
70–79 |
495 (18.9) |
13.56 |
490 (23.59) |
34.10 |
5 (0.92) |
0.23 |
|
80–89 |
492 (18.8) |
13.48 |
492 (23.69) |
34.24 |
- |
- |
|
Over 90 |
132 (5.0) |
3.62 |
132 (6.36) |
9.19 |
- |
- |
|
Sum |
2,623 |
71.86 |
2,077 |
144.55 |
546 |
24.67 |
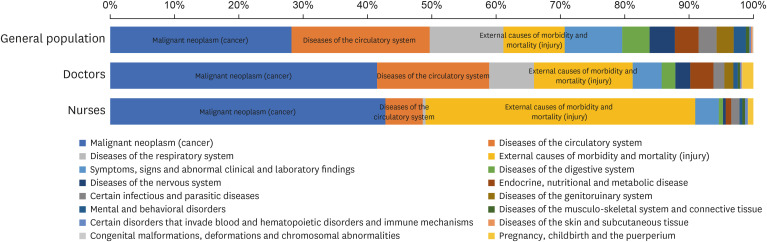
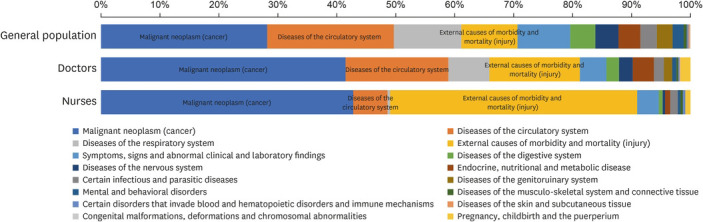
Compared to the general population, the proportion of mortality of doctors and nurses was equally high for those with malignant neoplasm, but the proportion of mortality from injury, addiction, and external causes was significantly higher in healthcare workers (
Fig. 1). In particular, nearly half of the nurses who died during the study period were found to have been killed by injury, addiction, and external causes.
Fig. 1
Causes of death in the general population versus healthcare workers.
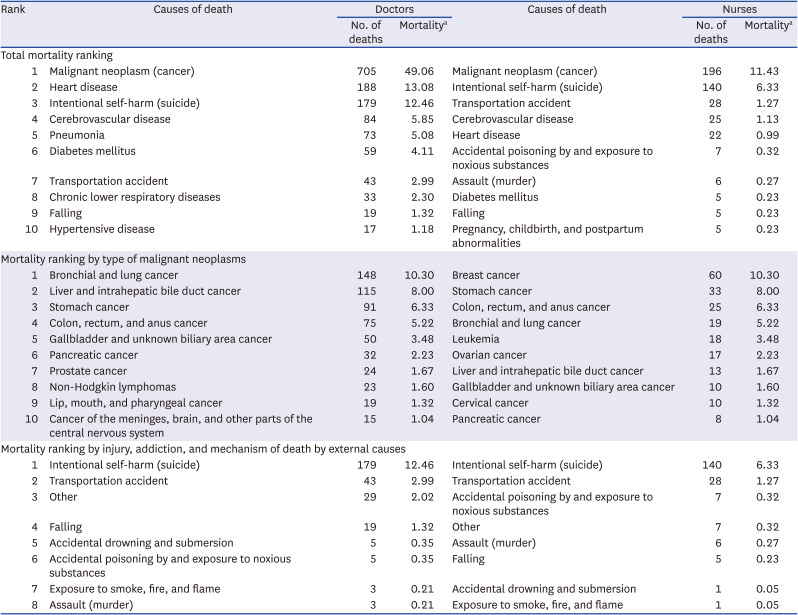
To analyze the cause of death in healthcare workers, we surveyed data from 1,834 doctors and 465 nurses except for 324 who were unknown causes of death (
Table 2). Doctors with malignant neoplasm had the highest mortality rate at 49.1 per 100,000 person-years, followed by those with heart disease (13.1 per 100,000 person-years), and intentional self-harm (12.5 per 100,000 person-years). For nurses, the death rate of those with malignant neoplasm was the highest at 11.4 per 100,000 person-years, followed by intentional self-harm (6.3 per 100,000 person-years), and transportation accidents (1.3 per 100,000 person-years).
Table 2
Ranked mortality by cause of death in healthcare workers
|
Rank |
Causes of death |
Doctors |
Causes of death |
Nurses |
|
No. of deaths |
Mortalitya
|
No. of deaths |
Mortalitya
|
|
Total mortality ranking |
|
1 |
Malignant neoplasm (cancer) |
705 |
49.06 |
Malignant neoplasm (cancer) |
196 |
11.43 |
|
2 |
Heart disease |
188 |
13.08 |
Intentional self-harm (suicide) |
140 |
6.33 |
|
3 |
Intentional self-harm (suicide) |
179 |
12.46 |
Transportation accident |
28 |
1.27 |
|
4 |
Cerebrovascular disease |
84 |
5.85 |
Cerebrovascular disease |
25 |
1.13 |
|
5 |
Pneumonia |
73 |
5.08 |
Heart disease |
22 |
0.99 |
|
6 |
Diabetes mellitus |
59 |
4.11 |
Accidental poisoning by and exposure to noxious substances |
7 |
0.32 |
|
7 |
Transportation accident |
43 |
2.99 |
Assault (murder) |
6 |
0.27 |
|
8 |
Chronic lower respiratory diseases |
33 |
2.30 |
Diabetes mellitus |
5 |
0.23 |
|
9 |
Falling |
19 |
1.32 |
Falling |
5 |
0.23 |
|
10 |
Hypertensive disease |
17 |
1.18 |
Pregnancy, childbirth, and postpartum abnormalities |
5 |
0.23 |
|
Mortality ranking by type of malignant neoplasms |
|
1 |
Bronchial and lung cancer |
148 |
10.30 |
Breast cancer |
60 |
10.30 |
|
2 |
Liver and intrahepatic bile duct cancer |
115 |
8.00 |
Stomach cancer |
33 |
8.00 |
|
3 |
Stomach cancer |
91 |
6.33 |
Colon, rectum, and anus cancer |
25 |
6.33 |
|
4 |
Colon, rectum, and anus cancer |
75 |
5.22 |
Bronchial and lung cancer |
19 |
5.22 |
|
5 |
Gallbladder and unknown biliary area cancer |
50 |
3.48 |
Leukemia |
18 |
3.48 |
|
6 |
Pancreatic cancer |
32 |
2.23 |
Ovarian cancer |
17 |
2.23 |
|
7 |
Prostate cancer |
24 |
1.67 |
Liver and intrahepatic bile duct cancer |
13 |
1.67 |
|
8 |
Non-Hodgkin lymphomas |
23 |
1.60 |
Gallbladder and unknown biliary area cancer |
10 |
1.60 |
|
9 |
Lip, mouth, and pharyngeal cancer |
19 |
1.32 |
Cervical cancer |
10 |
1.32 |
|
10 |
Cancer of the meninges, brain, and other parts of the central nervous system |
15 |
1.04 |
Pancreatic cancer |
8 |
1.04 |
|
Mortality ranking by injury, addiction, and mechanism of death by external causes |
|
1 |
Intentional self-harm (suicide) |
179 |
12.46 |
Intentional self-harm (suicide) |
140 |
6.33 |
|
2 |
Transportation accident |
43 |
2.99 |
Transportation accident |
28 |
1.27 |
|
3 |
Other |
29 |
2.02 |
Accidental poisoning by and exposure to noxious substances |
7 |
0.32 |
|
4 |
Falling |
19 |
1.32 |
Other |
7 |
0.32 |
|
5 |
Accidental drowning and submersion |
5 |
0.35 |
Assault (murder) |
6 |
0.27 |
|
6 |
Accidental poisoning by and exposure to noxious substances |
5 |
0.35 |
Falling |
5 |
0.23 |
|
7 |
Exposure to smoke, fire, and flame |
3 |
0.21 |
Accidental drowning and submersion |
1 |
0.05 |
|
8 |
Assault (murder) |
3 |
0.21 |
Exposure to smoke, fire, and flame |
1 |
0.05 |
We analyzed death by malignant neoplasm, injury, addiction, and external causes according to the type and mechanism. First, when we examined the mortality rate by the type of malignant neoplasm, doctors with bronchial and lung cancer had the highest mortality rate at 10.3 per 100,000 person-years, followed by liver and intrahepatic bile duct cancer (8.0 per 100,000 person-years), and stomach cancer (6.3 per 100,000 person-years). For nurses, those with breast cancer had the highest mortality rate at 2.7 per 100,000 person-years, followed by stomach cancer (1.5 per 100,000 person-years), and colon, rectum, and anus cancer (1.1 per 100,000 person-years).
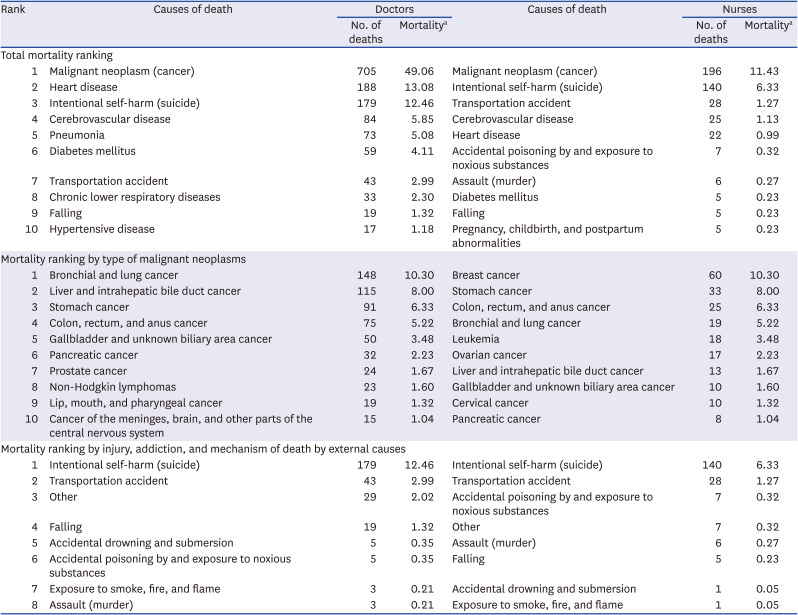
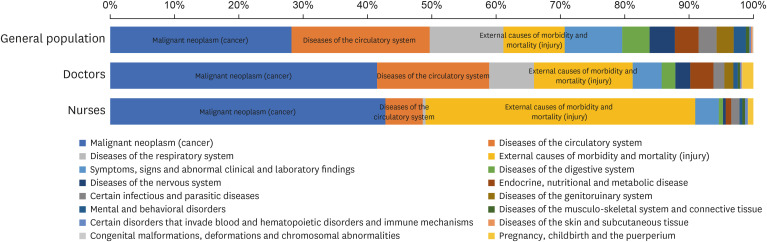
The rank of death from heart disease, intentional self-harm, pneumonia, and transportation accident were higher than those of the general public (
Fig. 2). In particular, nurses were more likely to die from injury than the general population, such that transportation accidents, addiction, exposure to toxic substances, assault (murder), and falling were among the top 10 causes of death.
Fig. 2
Comparison of mortality rankings between healthcare workers and the general population.
According to the ranking by the type of malignant neoplasm, colon, rectum and anus cancer, and non-Hodgkin lymphoma ranked high as causes of death in doctors. Further, unlike the general population, cancers of the gallbladder, biliary tract, prostate, lip, mouth, pharyngeal area, meninges, brain, and other parts of the central nervous system were among the top 10 causes of death in doctors. Nurses were significantly more likely to die from breast cancer than people in the general population, as well as from other cancers that specifically affect women, such as ovarian and cervical cancers. Nurses were also more likely to die from cancers of the stomach, colon, rectum, anus, leukemia, meninges, gallbladder, and biliary tract than people in the general population (
Fig. 2).
Our detailed ranking of the causes of death from injury showed that intentional self-harm was the number one cause of death in both healthcare workers and the general public, but this ratio was higher in healthcare personnel. In addition, deaths from unexpected poisoning and exposure to toxic substances were particularly high in healthcare personnel. In nurses, both the rank and proportion of unexpected poisoning and exposure to toxic substances were higher than that in doctors, as was the case with death by assault (murder) (
Fig. 2).
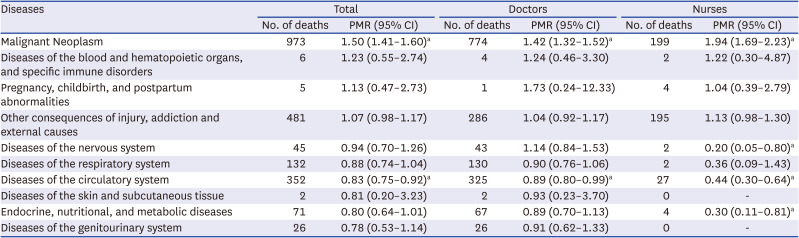
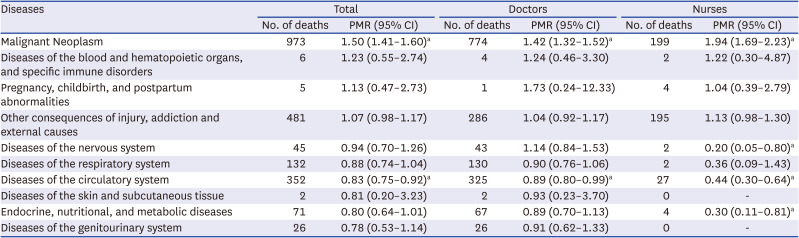
As shown in
Table 3, when analyzing the PMR values for cause of death among healthcare workers, the PMR value for malignant neoplasm was the highest at 1.50 and it was statistically significant (95% CI, 1.41–1.60). Diseases of the blood and hematopoietic organs, and specific immune disorders (1.23), pregnancy, childbirth, and postpartum abnormalities (1.13), and other consequences of injury, addiction, and external causes (1.82) all had PMR values greater than 1.0. However, the PMR value for diseases of the circulatory system was significant lower than the public (0.83; 95% CI, 0.75–0.92).
Table 3
Proportional mortality ratio by cause of death in healthcare workers
|
Diseases |
Total |
Doctors |
Nurses |
|
No. of deaths |
PMR (95% CI) |
No. of deaths |
PMR (95% CI) |
No. of deaths |
PMR (95% CI) |
|
Malignant Neoplasm |
973 |
1.50 (1.41–1.60)a
|
774 |
1.42 (1.32–1.52)a
|
199 |
1.94 (1.69–2.23)a
|
|
Diseases of the blood and hematopoietic organs, and specific immune disorders |
6 |
1.23 (0.55–2.74) |
4 |
1.24 (0.46–3.30) |
2 |
1.22 (0.30–4.87) |
|
Pregnancy, childbirth, and postpartum abnormalities |
5 |
1.13 (0.47–2.73) |
1 |
1.73 (0.24–12.33) |
4 |
1.04 (0.39–2.79) |
|
Other consequences of injury, addiction and external causes |
481 |
1.07 (0.98–1.17) |
286 |
1.04 (0.92–1.17) |
195 |
1.13 (0.98–1.30) |
|
Diseases of the nervous system |
45 |
0.94 (0.70–1.26) |
43 |
1.14 (0.84–1.53) |
2 |
0.20 (0.05–0.80)a
|
|
Diseases of the respiratory system |
132 |
0.88 (0.74–1.04) |
130 |
0.90 (0.76–1.06) |
2 |
0.36 (0.09–1.43) |
|
Diseases of the circulatory system |
352 |
0.83 (0.75–0.92)a
|
325 |
0.89 (0.80–0.99)a
|
27 |
0.44 (0.30–0.64)a
|
|
Diseases of the skin and subcutaneous tissue |
2 |
0.81 (0.20–3.23) |
2 |
0.93 (0.23–3.70) |
0 |
- |
|
Endocrine, nutritional, and metabolic diseases |
71 |
0.80 (0.64–1.01) |
67 |
0.89 (0.70–1.13) |
4 |
0.30 (0.11–0.81)a
|
|
Diseases of the genitourinary system |
26 |
0.78 (0.53–1.14) |
26 |
0.91 (0.62–1.33) |
0 |
- |
Doctors had PMR value over 1 for death associated with pregnancy, childbirth, and postpartum abnormalities (1.73), malignant neoplasm (1.42), diseases of the blood and hematopoietic organs, and specific immune disorders (1.24), diseases of the nervous system (1.14), and other consequences of injury, addiction, and external causes (1.04). The PMR value of malignant neoplasm (1.42; 95% CI, 1.32–1.52) was statistically significantly higher than that of the general public. And disease of the circulatory system (0.89; 95% CI, 0.80–0.99) was statistically significantly lower than that of the general public.
For nurses, the PMR was high (1.94; 95% CI, 1.69–2.23) for malignant neoplasm followed by diseases of the blood and hematopoietic organs, and specific immune disorders (1.22), other consequences of injury, addiction, and external causes (1.13), and pregnancy, childbirth, and postpartum abnormalities (1.04). The PMR value for diseases of the nervous system (0.20; 95% CI, 0.05–0.80) and the circulating system (0.44; 95% CI, 0.30–0.64) were significant lower than the general public.
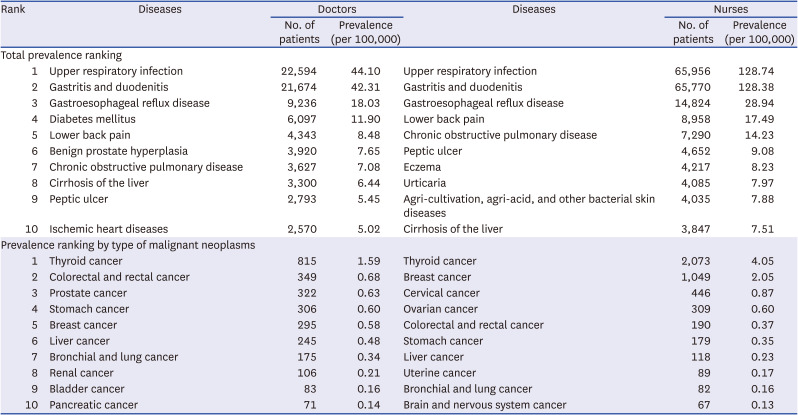
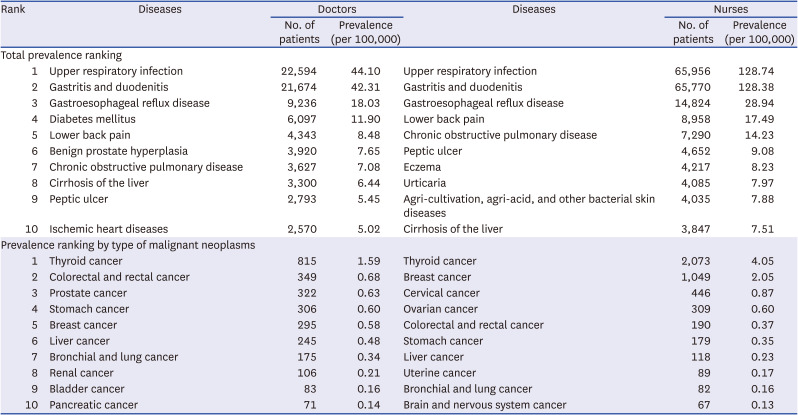
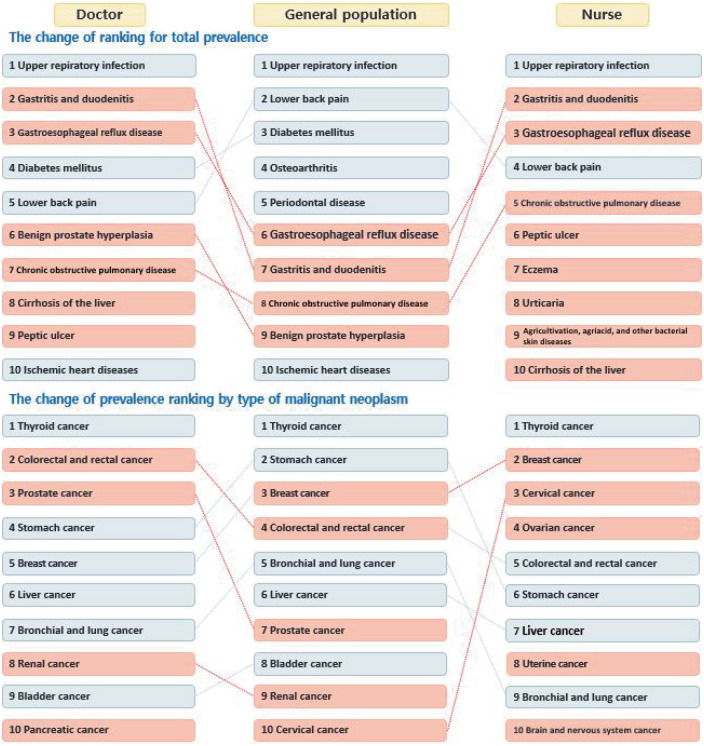
The following is a result of the prevalence of healthcare personnel, doctors had the highest prevalence of upper respiratory infections at 21,624 per 100,000 people, followed by gastritis and duodenitis (20,744 per 100,000 people), and gastroesophageal reflux disease (8,840 per 100,000 people). The prevalence of upper respiratory infections in nurses was highest at 29,938 per 100,000 people, followed by gastritis and duodenitis at 29,853 per 100,000 people. Nurses had a higher prevalence of disease than doctors, and women’s health issues were among the most prevalent diseases (
Table 4).
Table 4
Ranked disease prevalence in healthcare workers in 2017
|
Rank |
Diseases |
Doctors |
Diseases |
Nurses |
|
No. of patients |
Prevalence (per 100,000) |
No. of patients |
Prevalence (per 100,000) |
|
Total prevalence ranking |
|
1 |
Upper respiratory infection |
22,594 |
44.10 |
Upper respiratory infection |
65,956 |
128.74 |
|
2 |
Gastritis and duodenitis |
21,674 |
42.31 |
Gastritis and duodenitis |
65,770 |
128.38 |
|
3 |
Gastroesophageal reflux disease |
9,236 |
18.03 |
Gastroesophageal reflux disease |
14,824 |
28.94 |
|
4 |
Diabetes mellitus |
6,097 |
11.90 |
Lower back pain |
8,958 |
17.49 |
|
5 |
Lower back pain |
4,343 |
8.48 |
Chronic obstructive pulmonary disease |
7,290 |
14.23 |
|
6 |
Benign prostate hyperplasia |
3,920 |
7.65 |
Peptic ulcer |
4,652 |
9.08 |
|
7 |
Chronic obstructive pulmonary disease |
3,627 |
7.08 |
Eczema |
4,217 |
8.23 |
|
8 |
Cirrhosis of the liver |
3,300 |
6.44 |
Urticaria |
4,085 |
7.97 |
|
9 |
Peptic ulcer |
2,793 |
5.45 |
Agri-cultivation, agri-acid, and other bacterial skin diseases |
4,035 |
7.88 |
|
10 |
Ischemic heart diseases |
2,570 |
5.02 |
Cirrhosis of the liver |
3,847 |
7.51 |
|
Prevalence ranking by type of malignant neoplasms |
|
1 |
Thyroid cancer |
815 |
1.59 |
Thyroid cancer |
2,073 |
4.05 |
|
2 |
Colorectal and rectal cancer |
349 |
0.68 |
Breast cancer |
1,049 |
2.05 |
|
3 |
Prostate cancer |
322 |
0.63 |
Cervical cancer |
446 |
0.87 |
|
4 |
Stomach cancer |
306 |
0.60 |
Ovarian cancer |
309 |
0.60 |
|
5 |
Breast cancer |
295 |
0.58 |
Colorectal and rectal cancer |
190 |
0.37 |
|
6 |
Liver cancer |
245 |
0.48 |
Stomach cancer |
179 |
0.35 |
|
7 |
Bronchial and lung cancer |
175 |
0.34 |
Liver cancer |
118 |
0.23 |
|
8 |
Renal cancer |
106 |
0.21 |
Uterine cancer |
89 |
0.17 |
|
9 |
Bladder cancer |
83 |
0.16 |
Bronchial and lung cancer |
82 |
0.16 |
|
10 |
Pancreatic cancer |
71 |
0.14 |
Brain and nervous system cancer |
67 |
0.13 |
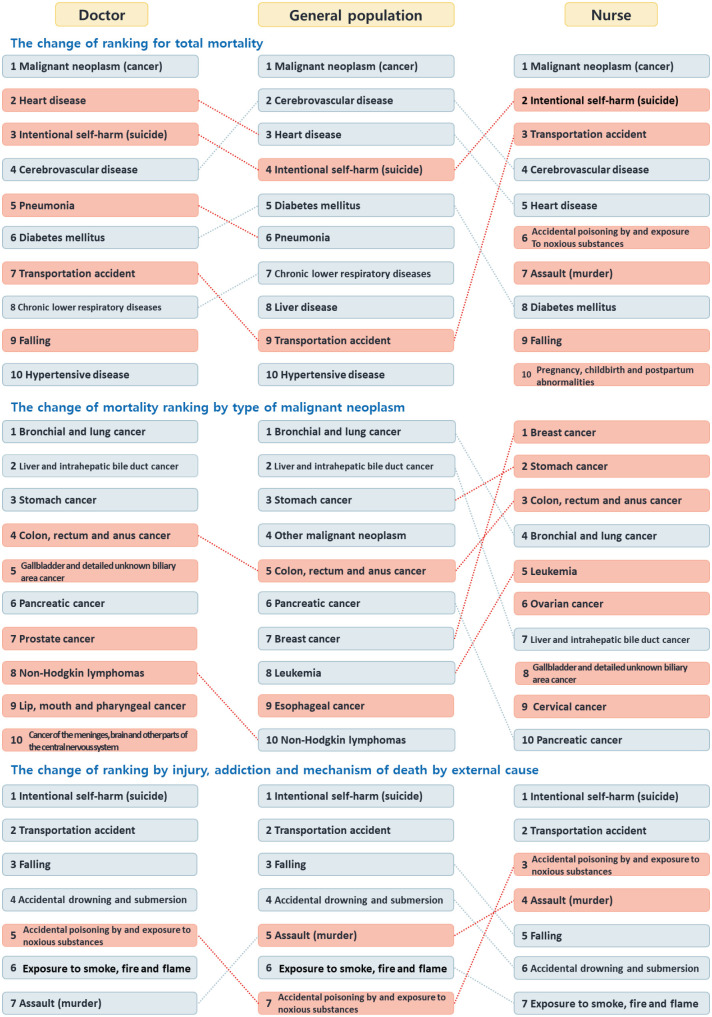
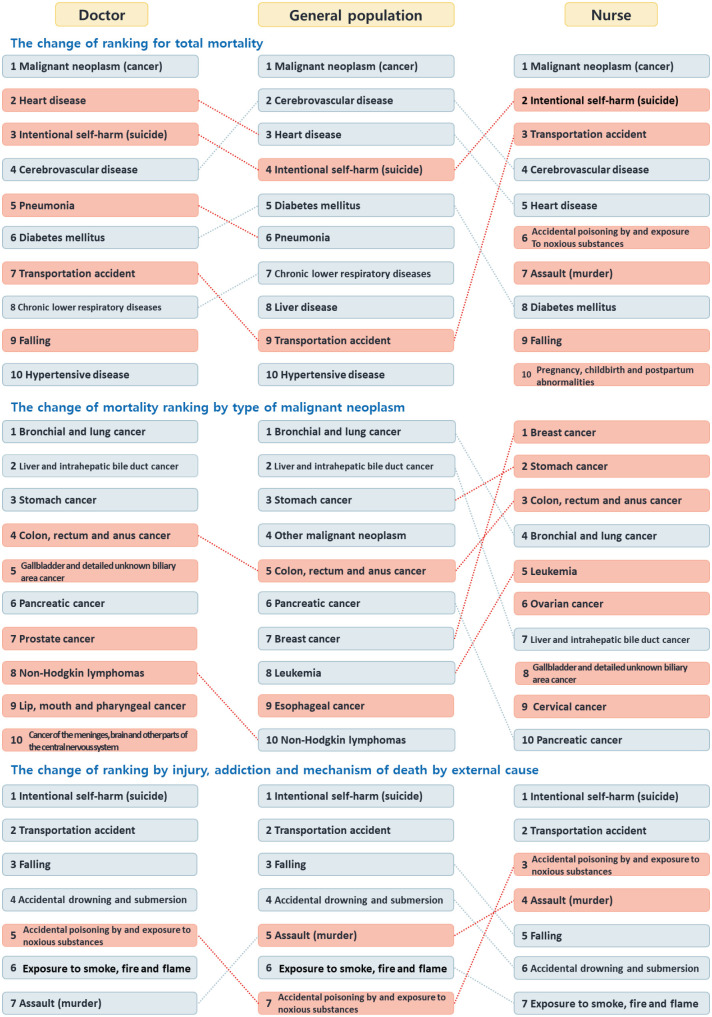
Next, we examined the prevalence by type of malignant neoplasm, which was the highest cause of death amongst healthcare workers. In both doctors and nurses, thyroid cancer had the highest prevalence, and it was the cause of death in 780 doctors and 941 nurses per 100,000 people. In doctors, colon and rectal cancers were the cause of death in 334 per 100,000 people, followed by prostate cancer (308 per 100,000 people), breast cancer (476 per 100,000 people), and cervical cancer (202 per 100,000 people) (
Table 4).
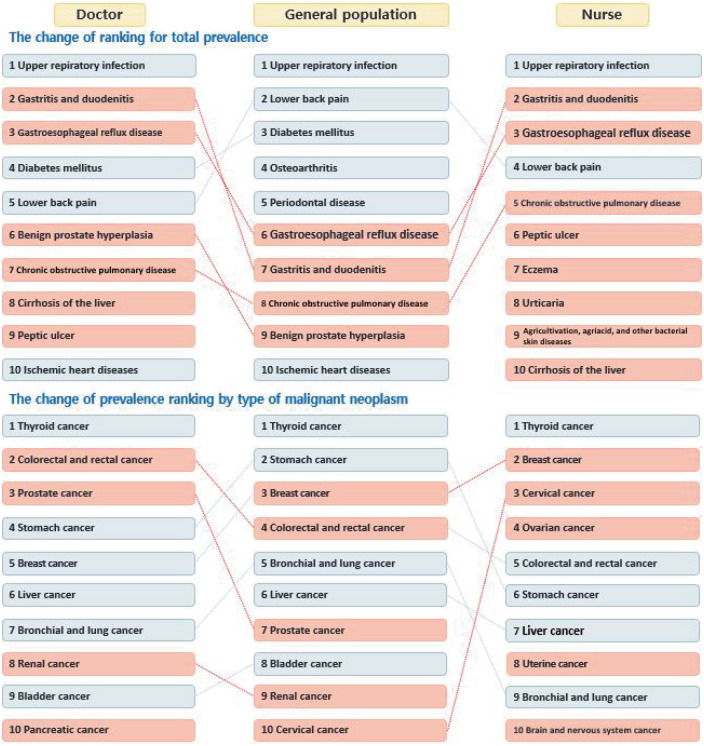
In particular, cancers of the colon, rectum, prostate, kidney, and pancreas were more frequent in doctors than in the general population, and cancers more likely to affect women, such as breast, cervical, ovarian, and uterine cancers, were more frequent in nurses than in the general population (
Fig. 3).
Fig. 3
Comparison of prevalence rankings between healthcare workers and the general population.
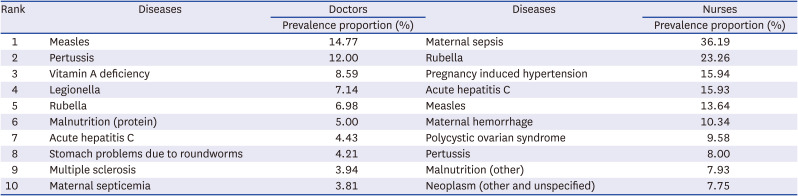
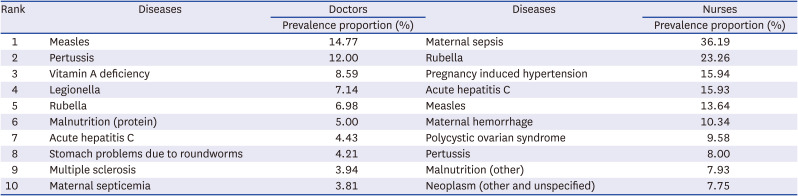
Calculating the proportion of healthcare worker among the total prevalence, the percentage was calculated by dividing the prevalence of certain diseases in the healthcare worker by the prevalence of total cases. We looked at the proportion of individuals who had diseases among healthcare personnel and the general population. Doctors were most likely to have measles (14.8%), followed by pertussis (12.0%), vitamin A deficiency (8.6%), legionella (7.1%), and rubella (7.0%). For nurses, maternal sepsis was most common (36.2%), followed by rubella (23.3%), pregnancy-induced hypertension (15.9%), acute hepatitis C (15.9%), and measles (13.6%). For both occupations, infectious diseases were among the most prevalent health concerns (
Table 5).
Table 5
Specific diseases in healthcare workers compared to the general population
|
Rank |
Diseases |
Doctors |
Diseases |
Nurses |
|
Prevalence proportion (%) |
Prevalence proportion (%) |
|
1 |
Measles |
14.77 |
Maternal sepsis |
36.19 |
|
2 |
Pertussis |
12.00 |
Rubella |
23.26 |
|
3 |
Vitamin A deficiency |
8.59 |
Pregnancy induced hypertension |
15.94 |
|
4 |
Legionella |
7.14 |
Acute hepatitis C |
15.93 |
|
5 |
Rubella |
6.98 |
Measles |
13.64 |
|
6 |
Malnutrition (protein) |
5.00 |
Maternal hemorrhage |
10.34 |
|
7 |
Acute hepatitis C |
4.43 |
Polycystic ovarian syndrome |
9.58 |
|
8 |
Stomach problems due to roundworms |
4.21 |
Pertussis |
8.00 |
|
9 |
Multiple sclerosis |
3.94 |
Malnutrition (other) |
7.93 |
|
10 |
Maternal septicemia |
3.81 |
Neoplasm (other and unspecified) |
7.75 |
DISCUSSION
We found that the main causes of death, mortality, and prevalence of disease in healthcare workers were different from those in the general population. Malignant neoplasm topped the list of causes of death for both the general population and healthcare workers. However, intentional self-harm and transportation accidents ranked higher in healthcare workers than in the general population. In particular, nurses ranked high in death from injury compared to the general population, and traffic accidents, unexpected addiction, exposure to toxic substances, assault, and falling also ranked high as causes of death. According to our findings regarding disease prevalence, both doctors and nurses had a higher prevalence of upper respiratory diseases compared to the general public, and also had a high rate of stress-related diseases such as gastrointestinal and respiratory disease. In addition, healthcare workers appeared to be particularly vulnerable to infectious diseases such as maternal sepsis, rubella, and measles.
Our data indicate that healthcare personnel had a high rate of death due to suicide. This is consistent with several previous studies. According to a Danish study, the relative risk for suicide amongst healthcare workers is 1.90 (95% CI, 1.63–2.21), being 1.87 (95% CI, 1.55–2.26) for physicians and 2.10 (95% CI, 1.58–2.79) for dentists.
17 Previous studies have also shown a high prevalence of mental illness amongst healthcare workers, particularly doctors. According to one study, the prevalence of depression and mental illness among doctors is higher than that in the general population.
18 According to a 2005 study of physicians in Korea, the overall mortality rate of physicians is lower than that of the general population, but the mortality rate from drug addiction and suicide is higher.
11 Other studies have reported that doctors are more vulnerable to suicide than individuals with other occupations.
12 Our data indicate that the rate of deaths from addiction was higher in healthcare worker than in the general public, but more research is needed to confirm this.
The highest PMR amongst healthcare personnel was for death associated with malignant neoplasm (1.50). We also found that the mortality rate of healthcare workers was higher than expected for blood diseases, and hematopoietic diseases related to immune mechanisms, pregnancy, childbirth, and postpartum abnormalities, injury, and addiction (higher than 1.0). Both doctors and nurses had high PMRs for malignant neoplasm, indicating that healthcare workers need special management to reduce mortality from malignant neoplasms. Considering the high prevalence of cancer in a 2016 survey of Korean doctors, a systematic study of the relationship between the occupational characteristics of healthcare workers and changes in health status due to malignant neoplasm is needed. For doctors, the highest PMR (1.73) was for death associated with pregnancy, childbirth, and postpartum conditions, and for nurses, this PMR was also not low (1.04). These results indicate that specialized healthcare for healthcare workers is needed, particularly in the postpartum period.
Healthcare workers had a high prevalence of stress-related diseases such as gastrointestinal and respiratory diseases. Previous studies have shown that doctors have a relatively high risk for hospitalization for all diseases compared to individuals with other occupations. In particular, there was a high risk for hospitalization for malignant neuropathy (cancer) and respiratory diseases.
19 In addition, among the healthcare workers in this study, the prevalence of cancers more likely to affect women was higher in nurses. Previous studies conducted in Taiwan have shown that men in the general population had a lower risk for all cancers compared to women in the general population, and that female doctors had a higher risk for cancer than male doctors, particularly breast cancer. Male doctors had a lower risk for all cancers compared to people in the general population, but a higher risk for prostate cancer.
20 Meanwhile, a study on the prevalence of chronic diseases in Taiwan reported that digestive system diseases were more common among medical personnel, and particularly doctors, than in the general population. Further, doctors had a higher prevalence of high blood pressure, hyperlipidemia, and asthma.
21 Doctors, nurses, and other healthcare workers have also been found to have a higher risk for migraine than the general population. Finally, doctors and nurses had a higher risk for stroke, high blood pressure, epilepsy, anxiety, depression, and insomnia.
22
The prevalence proportion of healthcare workers with infectious diseases was higher than that in the general population. This may be due to occupational characteristics such as busy schedules, night shifts, and exposure to harmful substances, although healthcare workers have better self-diagnosis ability than the general population. The vulnerability of medical personnel to infectious diseases has also been identified in previous studies. For instance, a study of 200 healthcare workers showed a high rate of needle injury
23, and studies estimating the burden of injury from contaminated sharp objects reported that the rates of HCV, HBV, and HIV infection in this population were 39%, 37%, and 4.4%, respectively, due to occupational exposure.
24
In some countries, databases that contain the health statuses of healthcare personnel are well established. In the USA, the Physicians Foundation continues to investigate job satisfaction, healthcare system trends, medical patterns, and workload through an e-mail survey called “A Survey of America’s Physicians.”
25 Taiwan has also conducted population-based cohort studies on stroke, chronic disease, and malignant neoplasms based on the National Health Insurance Research Database.
72021 These databases can facilitate population-based health research by integrating outpatient and hospitalization history, medical databases, and healthcare databases of prescription drugs, and by separating data from the general population and healthcare personnel within the integrated data.
2627
Some studies on the health status of doctors and nurses are also being conducted in Korea. In 2016 and 2020, the Korean Medical Association conducted a massive survey of doctors across the country on working conditions and satisfaction, evaluation of the healthcare system, lifestyle, and health conditions.
28 The Korean Center for Disease Control and Prevention has conducted the KNHS every six months since 2013 as an international joint study with Harvard University’s Graduate School of Health, which hosted the USA-based Nurses’ Health Study.
29 However, most of the research currently underway is cross-sectional, which makes it difficult to compare collected data, and the content of such surveys is limited.
30
While previous studies have been based on surveys, this study is unique in that we examined large national medical history datasets. However, this had several limitations. First, the prevalence of injuries could not be analyzed because the data sources were different. Healthcare workers who were not currently working may have been included in the subject group. In addition, a nurse as defined in this study was someone who worked in a healthcare institution from 2002 to 2017 and underwent at least one general health examination. Since the actual nurse turnover rate is high, most nurses working in healthcare institutions are young, which might have affected the type of disease causing the deaths of nurses. Nevertheless, this study of the health status of healthcare workers, based on the National Health Insurance Corporation database, demonstrates that it is possible to track health status continuously in the nation’s healthcare workforce and make plans to improve the existing infrastructure. In addition, our analysis of the cause of death, mortality, and prevalence of health conditions in healthcare personnel in Korea can be used to improve the working environment and quality of life of healthcare workers.
The health status of healthcare workforce is an important factor affecting the productivity of clinical sites as well as individual healthcare workers. Thus, identifying health problems in healthcare personnel is an important factor to improve the quality of healthcare services. Based on data from the Health Insurance Corporation, this study provides a foundation for improving the health of healthcare workers by evaluating the disease prevalence and risk for death, as well as identifying health-related factors, in this population. Our data indicate that healthcare workers face different health-related risks than those in the general population, and thus, the occupational characteristics of healthcare personnel should be considered when attempting to improve the existing infrastructure. Based on the findings of this prospective cohort study, health research and intervention programs are needed to improve the quality of life of healthcare workers in Korea.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download