INTRODUCTION
METHODS
Study design and the Korea TB cohort database
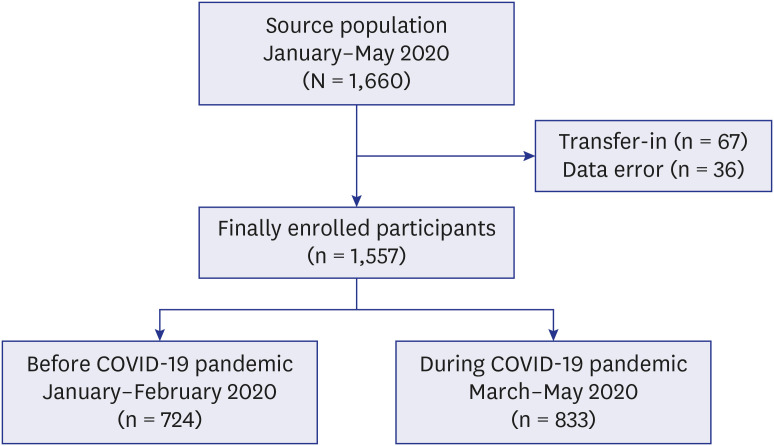
Study setting and participants
Outcome variables
Independent variables
Statistical analyses
Sample size
Ethics statement
RESULTS
Comparison of baseline characteristics
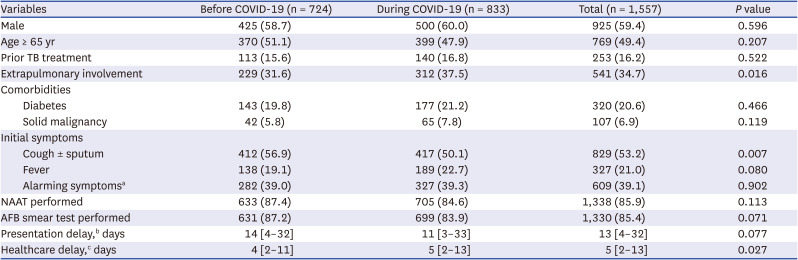
Table 1
Comparison of baseline characteristics of all enrolled participants with tuberculosis before and during the COVID-19 pandemic
Symptoms and Laboratory findings among pulmonary TB patients
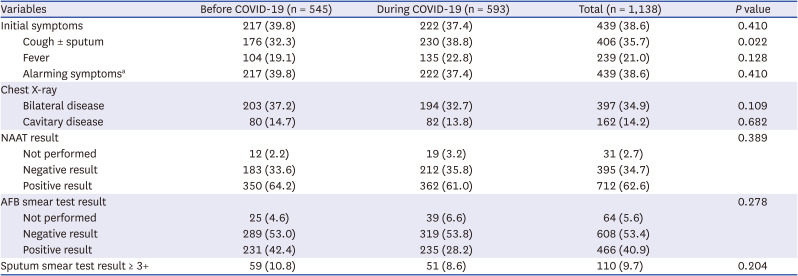
Table 2
Clinical profiles and laboratory findings of 1,138 participants with pulmonary tuberculosis before and during the COVID-19 pandemic
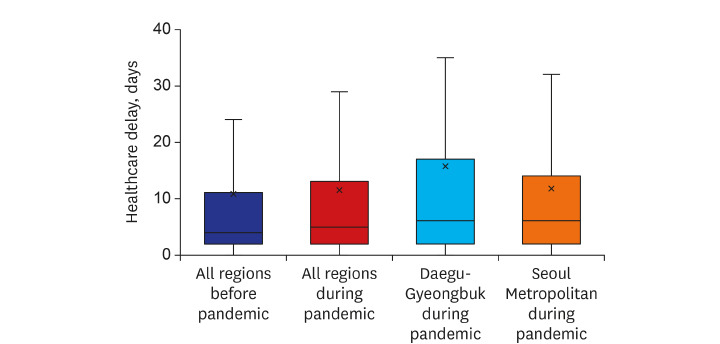
TB care delays across the country before and during the COVID-19 pandemic
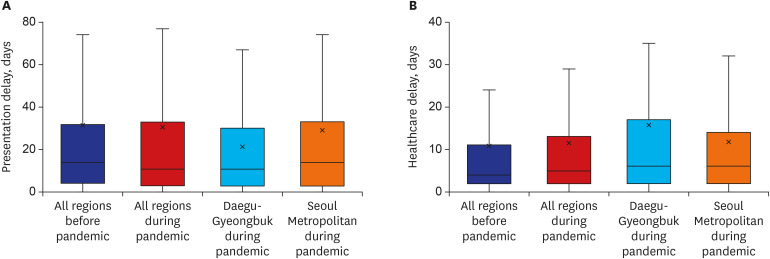 | Fig. 2Box plots of tuberculosis care delays across the country before and during the COVID-19 pandemic. (A) Presentation delay. (B) Healthcare delays.The five regions with the most reported cases of COVID-19 were selected during early pandemic and re-categorized into two regions based on their proximity; Daegu-Gyeongbuk, and Seoul Metropolitan Area (Seoul, Incheon, and Gyeonggi), and both presentation and healthcare delays were also calculated in two regions.
COVID-19 = coronavirus disease 2019.
|
Presentation delay
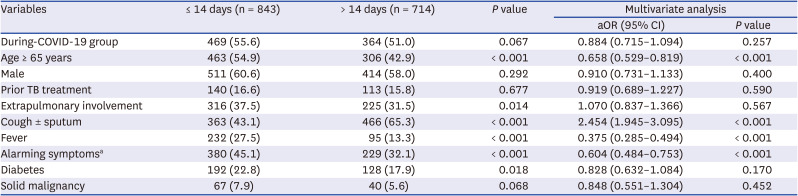
Table 3
Multivariate analysis for factors associated with presentation delay > 14 days
Healthcare delay
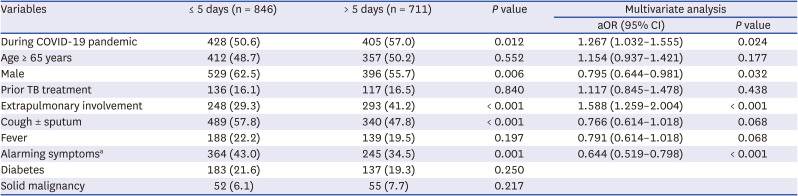
Table 4
Multivariate analysis for factors associated with healthcare delay > 5 days




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download