METHODS
We conducted a retrospective review of data from our AC team activation registry, prospectively collected for a 4-year period (June 2017 to May 2021) from our institution (a single tertiary academic hospital in South Korea).
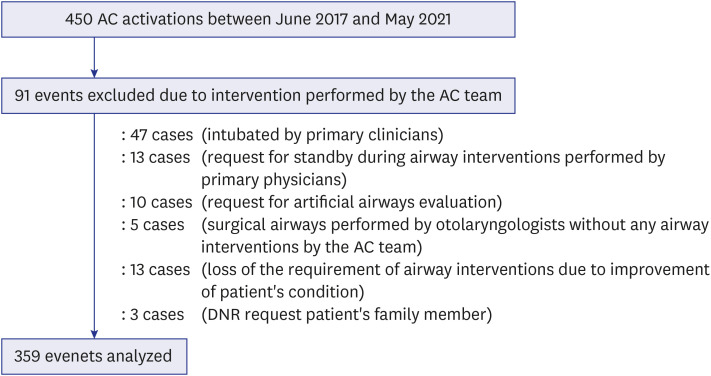
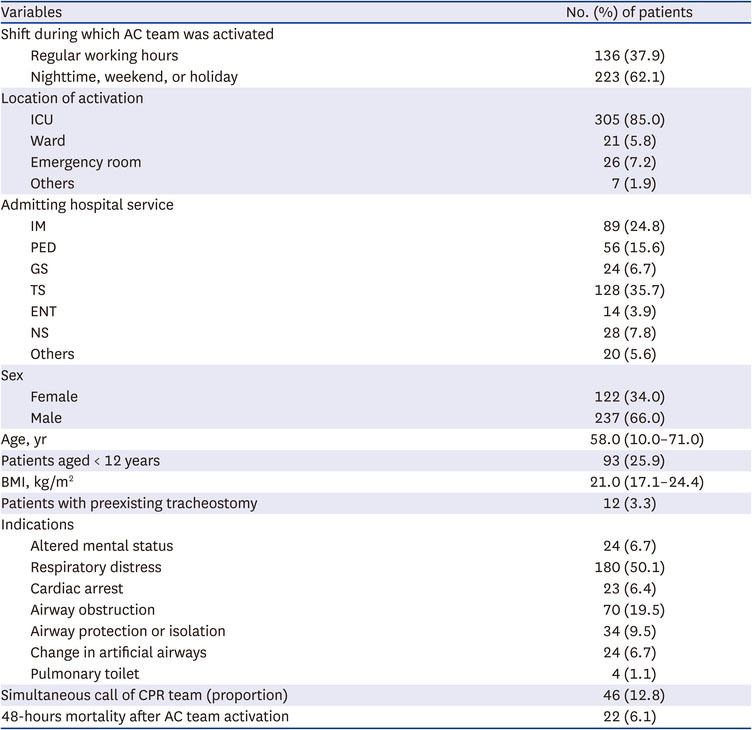
All AC team activation events involving airway intervention by the AC team during the study period were included in the analysis. Definitive airway intervention was defined as tracheal intubation, tracheostomy tube placement, or a change in an artificial airway. AC team activation events in which intubation was performed by the primary physician before the arrival of the AC team or with the AC team on standby were excluded. In addition, events involving an evaluation of an artificial airway were also excluded (
Fig. 1). Multiple AC team activations for single patients were included in the analysis.
Fig. 1
Flowchart for case selection.
AC = airway call, DNR = do-not-resuscitation.

Establishment of the AC team
Before the AC team system was established at our hospital, physicians from the anesthesiology department were individually called to assist with the management of difficult airways. In view of repeated episodes of failed intubation outside of the operating room, a hospital quality improvement committee decided to implement a rapid response system for airway emergencies outside the operating room in May 2017, with the goal of preventing delayed and failed intubation.
Our hospital (almost 2,000 beds) has three buildings connected through a walkway with three operating rooms in each building. During working hours (8 am to 5 pm), two AC teams operated independently. The AC teams consisted of anesthesiologists with subspecialty of pediatric or ear, nose, and throat (ENT) anesthesia and a senior anesthesia resident, who was in a charge of the post-anesthesia care room. Outside of working hours, a single AC team (an anesthesiologist and a senior anesthesia resident) was called from the anesthesia team on duty in the operating room. Thus, at any given time, one or two AC teams provided airway rescue services.
The AC team was activated through an emergency paging system with an expected response time of less than 10 minutes. When activated, the AC team brought a handheld emergency airway bag and glidescope (GVL Verathon Inc., Bothell, WA, USA) (
Supplementary Fig. 1). The standardized emergency airway bag included a video stylet (UE Video Stylet VL400-S2; UE Medical Devices, Newton, MA, USA), intubating stylets, tube exchangers, i-gel
® supraglottic airways (Intersurgical Ltd., Wokingham, UK) of all sizes, Yanker suction tube, portable real-time capnometer (EMMA Capnograph, Masimo Corporation, Irvine, CA, USA), and sugammadex. In some cases, other types of videolaryngoscope or fiberoptic bronchoscope were also brought to the bedside at the discretion of the AC team. A portable real-time capnometer was used to confirm successful tracheal intubation.
As each AC event was unique and different techniques might be needed to establish the airway, selection of the intubating devices was at the discretion of the AC team. However, a maximum of three attempts at intubation was recommended. If the patient required a surgical airway, the primary physicians or AC team providers activated the ENT call during the AC alert, which prompted the ENT physician to create a surgical airway.
According to policies in our hospital, intubation without the use of sedatives (primarily, midazolam or etomidate) was attempted in patients in cardiopulmonary distress. If patients were unable to cooperate with the intubation procedure, neuromuscular blocker was administered at the discretion of the AC team providers.
Data acquisition and analysis
AC activation-related data were recorded in a confidential airway registry by a member of the AC team shortly after the event. Data were collected using a standardized survey form, which included the date, time, patient demographics, location of the activation, indication for the AC team activation, number of intubation attempts, drugs and devices used for airway management, subjective difficulty of intubation (easy, moderate, or difficult), and a brief description of the overall event (
Supplementary Fig. 2). Detailed information regarding the patient’s condition before and after the AC team call were obtained through a review of the medical records.
Categorical variables are reported as number or proportion and continuous variables as median with interquartile range. Data are presented in a tabulated form and analyzed using descriptive statistics. Statistical analyses were performed using SPSS software (version 20; IBM Corp., Armonk, NY, USA).
Ethics statement
This study adhered to the Declaration of Helsinki. This study was registered with the Clinical Research Information Service (CRIS:
https://cris.nih.go.kr/cris/; ref:
KCT0006643) and approved by the Institutional Review Board of the Samsung Medical Center (SMC 2021–06–153; approved on June 25, 2021). Informed consent was waived by the board.
RESULTS
During the 4-year study period, the team was activated 450 times, at an average of 9.4 events per month. Out of these, 91 activations (20.2%) did not require airway intervention and were excluded from the analysis (
Fig. 1). Thus, we analyzed data from 359 events.
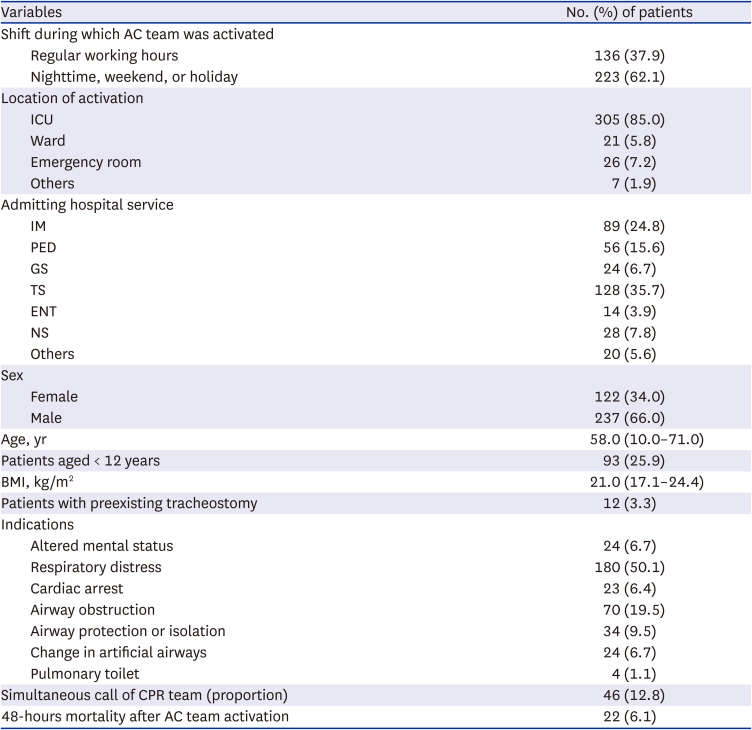
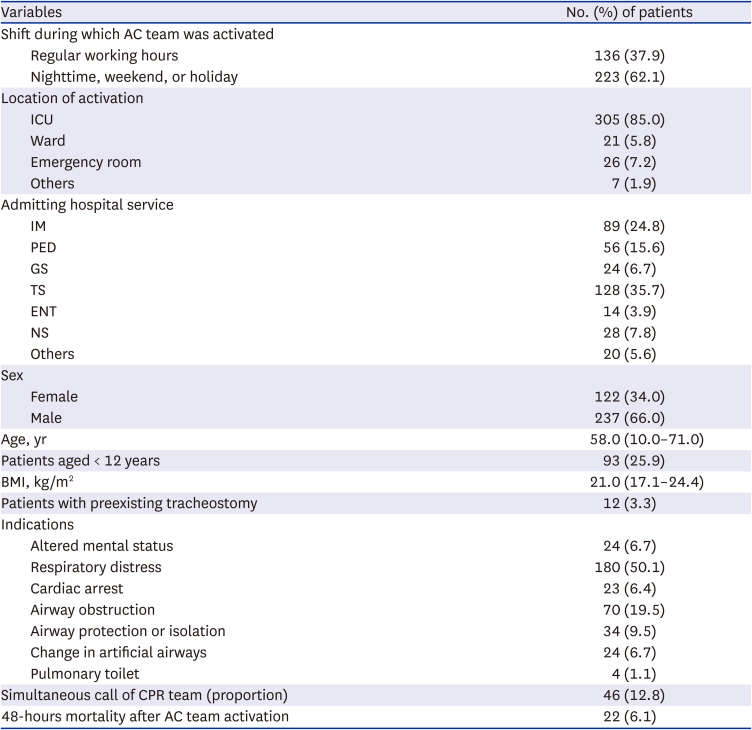
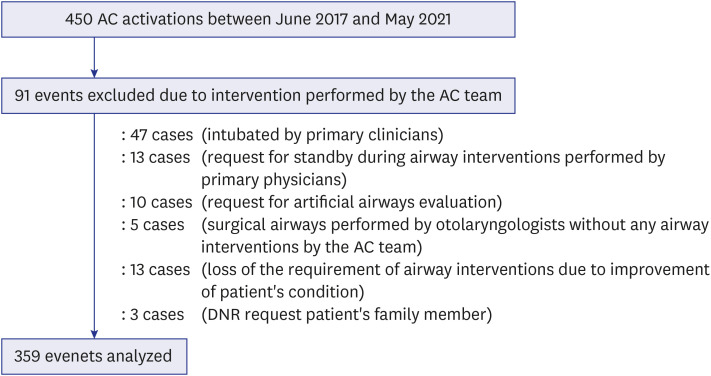
Activations were more common outside of normal working hours (62.1%, 223/359). Most events occurred in the intensive care unit (ICU) (n = 305, 85.0%), followed by the emergency room (n = 26, 7.2%) and general wards (n = 21, 5.8%) (
Table 1).
Table 1
AC team activations and patient characteristics (n = 359)
|
Variables |
No. (%) of patients |
|
Shift during which AC team was activated |
|
|
Regular working hours |
136 (37.9) |
|
Nighttime, weekend, or holiday |
223 (62.1) |
|
Location of activation |
|
|
ICU |
305 (85.0) |
|
Ward |
21 (5.8) |
|
Emergency room |
26 (7.2) |
|
Others |
7 (1.9) |
|
Admitting hospital service |
|
|
IM |
89 (24.8) |
|
PED |
56 (15.6) |
|
GS |
24 (6.7) |
|
TS |
128 (35.7) |
|
ENT |
14 (3.9) |
|
NS |
28 (7.8) |
|
Others |
20 (5.6) |
|
Sex |
|
|
Female |
122 (34.0) |
|
Male |
237 (66.0) |
|
Age, yr |
58.0 (10.0–71.0) |
|
Patients aged < 12 years |
93 (25.9) |
|
BMI, kg/m2
|
21.0 (17.1–24.4) |
|
Patients with preexisting tracheostomy |
12 (3.3) |
|
Indications |
|
|
Altered mental status |
24 (6.7) |
|
Respiratory distress |
180 (50.1) |
|
Cardiac arrest |
23 (6.4) |
|
Airway obstruction |
70 (19.5) |
|
Airway protection or isolation |
34 (9.5) |
|
Change in artificial airways |
24 (6.7) |
|
Pulmonary toilet |
4 (1.1) |
|
Simultaneous call of CPR team (proportion) |
46 (12.8) |
|
48-hours mortality after AC team activation |
22 (6.1) |

Ninety-three events (25.9%) involved patients aged < 12 years and most of them (78.5%, 73/93) involved pediatric patients aged < 2 years. In 46 events, the cardiopulmonary resuscitation team was simultaneously activated due to combined cardiac arrest (
Table 1).
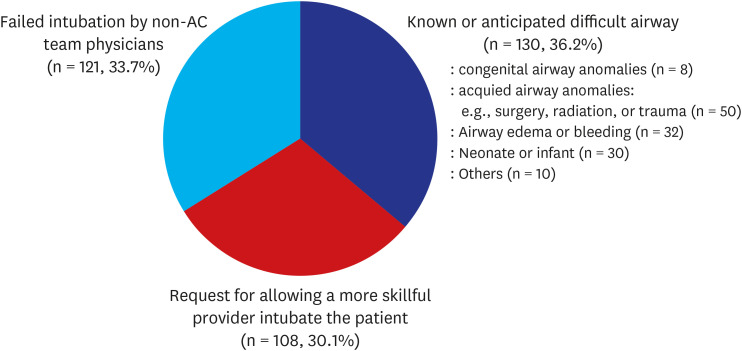
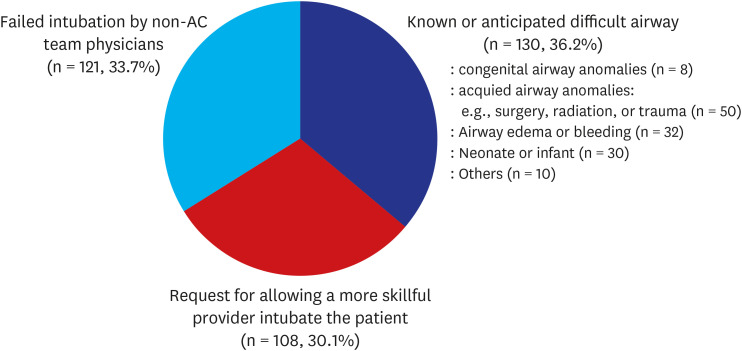
The AC team was activated due to known or anticipated difficulty securing the airway in only 36.2% of the events, which in most patients was due to acquired airway anomalies (n = 49), such as having a mass adjacent to, invading, or compressing the airway; or a history of oral, pharyngeal, or laryngeal surgeries, radiation therapy, or trauma. Other factors included airway edema or bleeding (n = 32) and very young age (≤ 1 years; n = 30). Many AC activation (30.1%) were requested for allowing a more skillful provider intubate the patient by the determination of the primary physicians (
Fig. 2).
Fig. 2
Reasons for AC team activations.
AC = airway call.

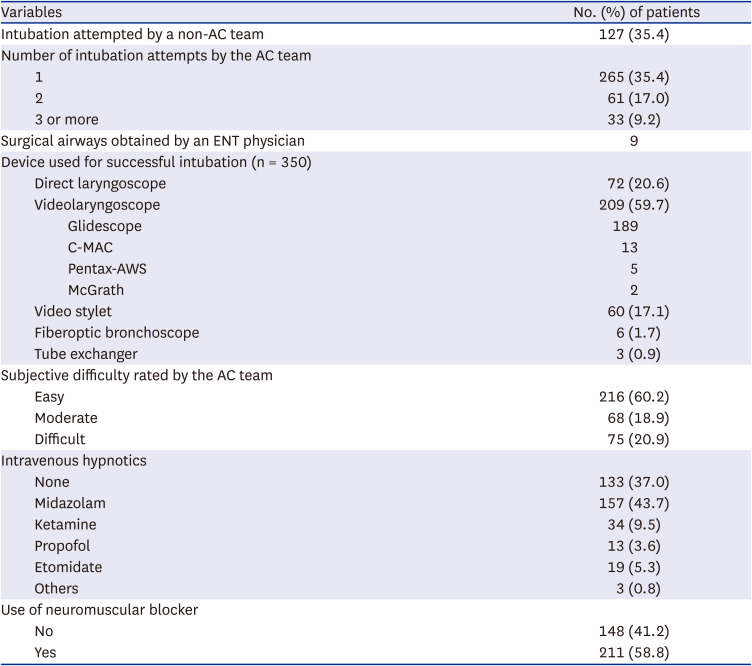
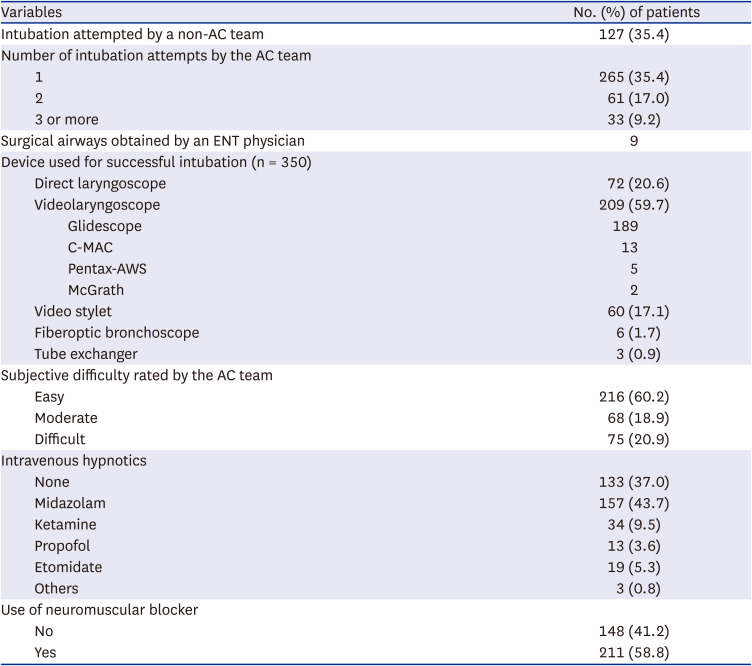
Prior to the arrival of the AC team, non-AC team physicians attempted intubation in 35.4% (n = 127) of patients. In 71.3% (256/359) of the cases, successful intubation was performed by the AC team on the first attempt. However, three or more attempts were performed in 33 cases. In nine cases, tracheal intubation failed and cricothyrotomy or tracheostomy was required, for which the ENT physicians were called (
Table 2).
Table 2
Characteristics of airway interventions performed by the AC team (n = 359)
|
Variables |
No. (%) of patients |
|
Intubation attempted by a non-AC team |
127 (35.4) |
|
Number of intubation attempts by the AC team |
|
|
1 |
265 (35.4) |
|
2 |
61 (17.0) |
|
3 or more |
33 (9.2) |
|
Surgical airways obtained by an ENT physician |
9 |
|
Device used for successful intubation (n = 350) |
|
|
Direct laryngoscope |
72 (20.6) |
|
Videolaryngoscope |
209 (59.7) |
|
|
Glidescope |
189 |
|
|
C-MAC |
13 |
|
|
Pentax-AWS |
5 |
|
|
McGrath |
2 |
|
Video stylet |
60 (17.1) |
|
Fiberoptic bronchoscope |
6 (1.7) |
|
Tube exchanger |
3 (0.9) |
|
Subjective difficulty rated by the AC team |
|
|
Easy |
216 (60.2) |
|
Moderate |
68 (18.9) |
|
Difficult |
75 (20.9) |
|
Intravenous hypnotics |
|
|
None |
133 (37.0) |
|
Midazolam |
157 (43.7) |
|
Ketamine |
34 (9.5) |
|
Propofol |
13 (3.6) |
|
Etomidate |
19 (5.3) |
|
Others |
3 (0.8) |
|
Use of neuromuscular blocker |
|
|
No |
148 (41.2) |
|
Yes |
211 (58.8) |

The most common device used for successful intubation was the videolaryngoscope (59.7%, 209/350). The most common type of videolaryngoscope was the glidescope. Intravenous sedatives were administered in 63.0% (n = 226) of cases. The most commonly used sedatives included midazolam (n = 157), followed by ketamine (n = 34) and etomidate (n = 19). In 93.4% (211/226) of the patients who received sedatives, a neuromuscular blocker was also administered. Sedatives were not administered in 44.3% (31/70) of the patients with airway obstruction and 91.3% (21/23) with cardiac arrest.
The AC teams rated the subjective difficulty of the intubation process as easy, moderate, and difficult in 60.2% (n = 216), 18.9% (n = 68), and 20.9% (n = 75) of the cases, respectively (
Table 2).
In 350 of the 359 events, tracheal intubation was successfully performed by the AC team without the need for a surgical airway, a success rate of 97.5%.
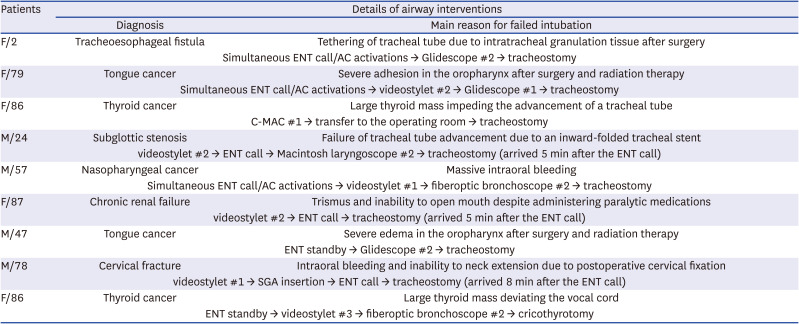
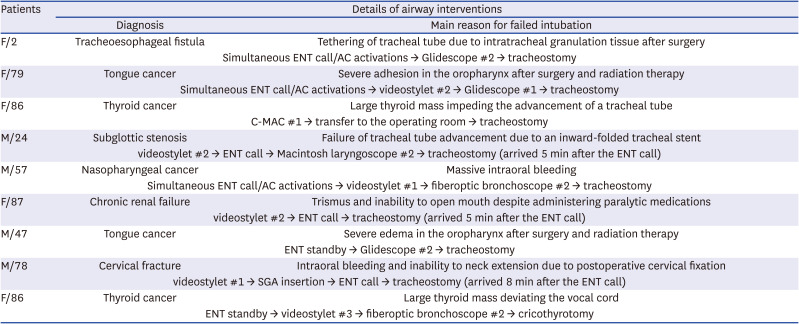
Table 3 presents brief descriptions of the events (n = 9) in which a surgical airway was created by ENT physicians due to failed laryngoscopy. In 5 of 9 events, ENT airway calls were activated by the primary physicians prior to AC activations or simultaneously.
Table 3
Brief description of events (n = 9) in which intubation by the AC team failed and surgical airway was performed by an ENT physician
|
Patients |
Details of airway interventions |
|
Diagnosis |
Main reason for failed intubation |
|
F/2 |
Tracheoesophageal fistula |
Tethering of tracheal tube due to intratracheal granulation tissue after surgery |
|
Simultaneous ENT call/AC activations → Glidescope #2 → tracheostomy |
|
F/79 |
Tongue cancer |
Severe adhesion in the oropharynx after surgery and radiation therapy |
|
Simultaneous ENT call/AC activations → videostylet #2 → Glidescope #1 → tracheostomy |
|
F/86 |
Thyroid cancer |
Large thyroid mass impeding the advancement of a tracheal tube |
|
C-MAC #1 → transfer to the operating room → tracheostomy |
|
M/24 |
Subglottic stenosis |
Failure of tracheal tube advancement due to an inward-folded tracheal stent |
|
videostylet #2 → ENT call → Macintosh laryngoscope #2 → tracheostomy (arrived 5 min after the ENT call) |
|
M/57 |
Nasopharyngeal cancer |
Massive intraoral bleeding |
|
Simultaneous ENT call/AC activations → videostylet #1 → fiberoptic bronchoscope #2 → tracheostomy |
|
F/87 |
Chronic renal failure |
Trismus and inability to open mouth despite administering paralytic medications |
|
videostylet #2 → ENT call → tracheostomy (arrived 5 min after the ENT call) |
|
M/47 |
Tongue cancer |
Severe edema in the oropharynx after surgery and radiation therapy |
|
ENT standby → Glidescope #2 → tracheostomy |
|
M/78 |
Cervical fracture |
Intraoral bleeding and inability to neck extension due to postoperative cervical fixation |
|
videostylet #1 → SGA insertion → ENT call → tracheostomy (arrived 8 min after the ENT call) |
|
F/86 |
Thyroid cancer |
Large thyroid mass deviating the vocal cord |
|
ENT standby → videostylet #3 → fiberoptic bronchoscope #2 → cricothyrotomy |

The main reasons for failed laryngoscopy were failure of tracheal tube advancement due to an intrinsic or extrinsic mass (n = 4), active intraoral bleeding (n = 2), severe oropharyngeal adhesions (n = 2), and severe airway edema (n = 1).
No deaths or hypoxic brain damage were attributed to the inability to secure the airway by the AC or ENT teams. The main cause of all deaths within 48 hours of the event was known underlying disease progression.
DISCUSSION
We describe the implementation of an AC system composed of anesthesiologists, and the characteristics and clinical context of AC activations during the first 4 years of operation in a Korean tertiary hospital.
Inappropriate management of difficult airway situations can lead to devastating consequences for the patients, their families, healthcare providers, and hospitals. Airway management outside the operating room is particularly challenging due to a lack of availability of advanced airway equipment and inadequate training and experience of providers regarding advanced airway management.
249 Thus, a rapid response team for the management of difficult airways outside the operating room was first developed at Johns Hopkins Hospital in 2008.
9 This system was subsequently modified and introduced to many other hospitals worldwide. The use of AC teams leads to reduced airway-related morbidity and mortality outside of the operating room.
56789 In this context, we established an AC team (composed of anesthesiologists) to improve emergency airway management outside the operating room in 2017.
In contrast to other studies,
1011 the AC teams were activated more frequently outside working hours than during working hours in our study, which may be attributed to a lack of supervising staff in the wards and ICU on weekends, holidays, and nights. Because emergency intubation performed by primary physicians outside of working hours is associated with a lower success rate and higher complication rate compared to that performed during working hours,
1213 it is highly recommended that the AC team provides continuous coverage.
In our study, the AC team was activated in the ICU in a majority of the cases (85.0%), suggesting that high-risk patients were effectively routed to the ICU. A previous study
2 reported that patient location (general ward
vs. emergency room) is an independent predictor of adverse outcomes. Thus, a clinical pathway that ensures that patients at high risk for airway compromise are admitted to the ICU is necessary for the efficient operation of the AC team system.
During the study period, the AC team was activated at an average of 9.4 times per month. In addition to the generally accepted indications of AC team activation (failed intubation by primary physicians or an anticipated or known difficult airway), the AC team was activated in 108 events solely to allow intubation by a more skillful provider, despite no intubation attempts by the primary physicians. Such activation may be reduced by following stringent AC team activation criteria. However, because multiple intubation attempts are associated with poor outcomes,
214 AC team activation criteria should be tailored on the basis of potential risk related to failed intubation attempts by the primary physicians or delayed AC team activation.
Most studies have recommended a multidisciplinary model of the airway rapid response team outside of the operating room, including an anesthesiologist, ENT physician, emergency department physician or trauma surgeon, nurse, pharmacist, and respiratory therapist.
567891011 If effective teamwork, communication, and coordination are ensured among clinicians, an ENT physician can manage tracheostomy-related problems and create surgical airways. However, instead of including the ENT physician in all AC activations, we implemented a separate ENT airway call system, similar to a previous study.
15
Although most patients requiring AC team activation had a natural airway, some had a tracheostomy tube. When such tubes are dislodged or occluded, an AC team would be activated. In our study, 30 AC team activations were for patients with a tracheostomy, of which only 12 cases needed airway intervention. In such cases, appropriate medical decision by the primary physicians may divert a considerable number of activations from the AC team to the ENT physicians.
In our study, nine patients (i.e., 2.5% of the cases needed intubation by the AC team) required an additional ENT airway call for securing a surgical airway, similar to a report from a 628-bed pediatric hospital (2.5% of 162 activations),
16 but much higher than that of another hospital (0.26% of 3,423 activations).
2
The frequency of emergent surgical airways is significantly influenced by the proportion of patients with complex airways, such as medical or surgical patients with oro-pharyngo-laryngeal diseases or congenital airway anomalies. If AC team is composed solely of anesthesiologists, medical decision of the primary physicians (ENT airway call, AC activation, or both) is more important, especially in a tertiary or academic hospitals. In this regard, the deficiency of the institutional consensus criteria for ENT airway call might increase the intubation failure rate of the AC team in this study.
Notably, introduction of diverse videolaryngoscopes and supra-glottic airways can significantly reduce the need for surgical airways or even the morbidity/mortality of delayed call for surgical airways. In this study, although an ENT call was activated after the failure of intubation attempts by the AC team, oxygenation via a supra-glottic airway could provide with enough time for the completion of tracheostomy in a patient with cervical fracture (
Table 3). Thus, dual operation of an AC team composed of anesthesiologists and an ENT airway call team may be an alternative option, particularly in small or non-academic hospitals.
In addition to the development of an AC team and a universal paging system, a standardized emergency airway bag (or cart/trolley) is a critical component of an AC system.
79 In the UK Fourth National Audit Project report, equipment- or resource-related causal and contributory factors were found in 36.1% of major airway complications in the ICU.
17 Considering the limited availability of equipment and drugs outside the operating room, optimal composition and regular checks of the emergency airway bag are essential.
In our study, videolaryngoscope was the most common device (209 cases) used for definitive airway intervention. In particular, the glidescope was the most common type of videolaryngoscope and the default included in the emergency airway bag. A recent meta-analysis
18 suggested that videolaryngoscopy may reduce the incidence of failed intubations, particularly in patients with a difficult airway, compared to direct laryngoscopy. In our study, videolaryngoscopes were particularly useful for patients with anatomically distorted views of the glottis or limited mouth opening or neck extension. However, because securing a clear view is necessary for successful videolaryngoscopy, these devices have limited usefulness in patients with active airway bleeding.
Portable capnography was included in the emergency airway response kit of the AC team to confirm successful intubation. A previous study demonstrated the lack of capnography as a major factor in airway-related mortality and morbidity outside the operating room.
17 Considering the lack of immediate availability outside the operating room, sugammadex was also in the kit for rapid reversal of neuromuscular blocker when needed.
Prior to this analysis, a percutaneous cricothyrotomy set was not included in the kit due to limited clinical expertise of anesthesiologists in performing this procedure.
19 Since the introduction of a biannual difficult airway course, a percutaneous cricothyrotomy set is now included in the emergency airway response kit. All AC team activation events should be reviewed at regular intervals, and items included in the kit may be removed or added based on advances in airway management.
9
This study had limitations inherent in such analyses. Data were retrospectively collected from a single hospital and were not compared to data from before the implementation of the AC system. Because immediate complications were not included in the prospective airway registry, we could not assess hemodynamic changes, hypoxemia, and airway injuries associated with airway intervention.
The absence of the data regarding the time from AC activation to establishment of the airway may be criticized. When planning the construction of the airway registry, we realized that the value of such a variable could be distorted by delayed AC activation, patient’s specific condition, or capability of maintaining the oxygenation during AC alert. Thus, we did not collect these time data prospectively.
In addition, our results must be cautiously applied to non-academic or small hospitals. The airway rescue system should be tailored based on the resources, capabilities, and patient population of the hospital.
In conclusion, when coupled with appropriate assistance from an ENT airway call team, an AC team composed of anesthesiologists could be an efficient alternative to a multidisciplinary airway response team for outside the operating room. As the primary physician’s assessment of need for surgical airway is pivotal in this system, institutional consensus criteria for each airway call activation is necessary. In addition, incorporation of percutaneous cricothyrotomy to the AC team’s interventions can close a realistic gap between ENT airway call and AC team activation.
Our study offers insight into the implementation of a difficult airway response system in non-academic and small hospitals with limited financial resources, no residents or fellows, and few in-house medical staff. Further studies in various hospital settings are necessary to evaluate the effects of such a team on patient outcomes and cost effectiveness.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download