INTRODUCTION
METHODS
Study population
Basic characteristics and group distribution
Surgical technique
1. A zero-degree lens was used from the beginning of the surgery. An incision was made on the anterior peritoneum to access the Retzius space, followed by dorsal vein ligation and placement of a periurethral suspension stitch (anchoring of periosteum) in all patients.18
2. Thereafter, the surgery was performed using a 30° down lens. The anterior bladder neck was incised between the bladder and prostate to expose the vas deference and seminal vesicle.
3. After dissection of the vas deference and seminal vesicle without thermal ligation, the posterior plane could be accessed through the interfascial plane (Fig. 1A). Here, it was important for the assistant to symmetrically hold the seminal vesicle in the antero-cranial aspect with the 4th robotic arm.
4. After some degree of detachment, the lens was switched from 30° down to 30° up by toggling (Fig. 1B). The proper dissection of the interfascial plane with exposure of the medial side of the NVB is a good sign of nerve sparing. When the bilateral NVB is dissected carefully with scissors while maintaining the interfascial plane, the surgeon may sense that nerve sparing is almost complete.
5. The 30° down lens was used again. The levator fascia over the prostate was opened sharply to expose the NVB. The NVB can be easily separated even with a little dissection, and surgeon may find successful tunneling present below (Fig. 1C). The plane was then continued in a retrograde direction toward the base of the prostate to detach the NVB from the prostatic pedicle completely. “Tunneling” is defined as a connection between the prostatic anterior aspect and Denonvillier's fascia following the separation of the NVB (Fig. 1C).
6. The plane was then continued toward the apex by detaching the prostate from the NVB.
7. All cases underwent bladder neck and posterior reconstruction as described in a previous study.16
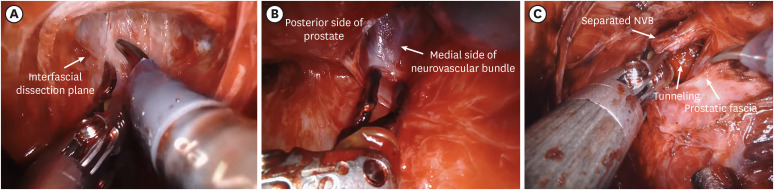 | Fig. 1Key surgical steps for retrograde early release using toggling technique. (A) 30° down view: The appropriate dissection approach into the interfascial plane is important in this step. The deeper dissection plane between the prostate fascia and the neurovascular bundle is rarely seen in this view. (B) 30° up view: After the proper dissection of the interfascial plane followed by toggling, the medial side of the neurovascular bundle is visible. The accomplishment of this process guarantees sparing of the whole neurovascular bundle. (C) 30° down view: After toggling again, the final step of the neurovascular bundle sparing process is performed anteriorly. Tunneling, defined as a connection between the anterior aspect of the prostrate and the Denonvillier’s fascia following separation of the neurovascular bundle, can be observed here.NVB = neurovascular bundle.
|
Main outcome measures
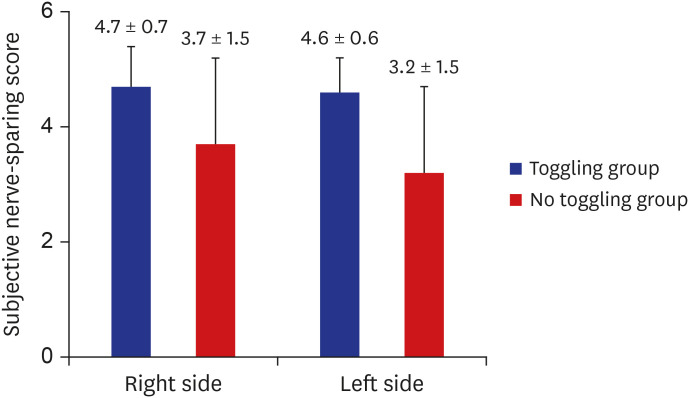
Facilitation of NVB sparing: correlation test and subjective nerve sparing score
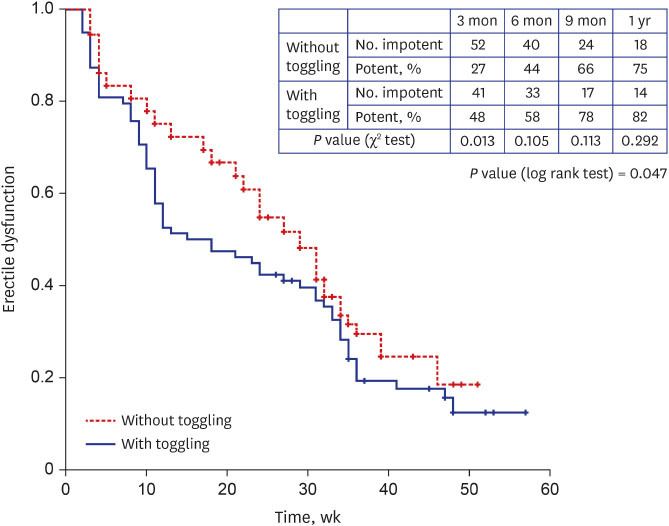
Recovery rate of ED between groups: Kaplan-Meier analysis
Statistical analysis
Ethics statement
RESULTS
Table 1
Baseline demographics and clinical data of patients with ≥ 1 year follow-up of the two groups
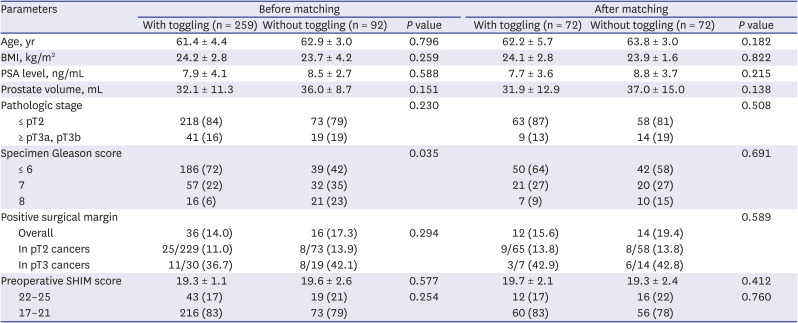
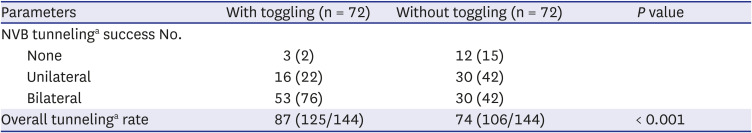
Table 2
Neurovascular bundle tunneling success rate between the two groups
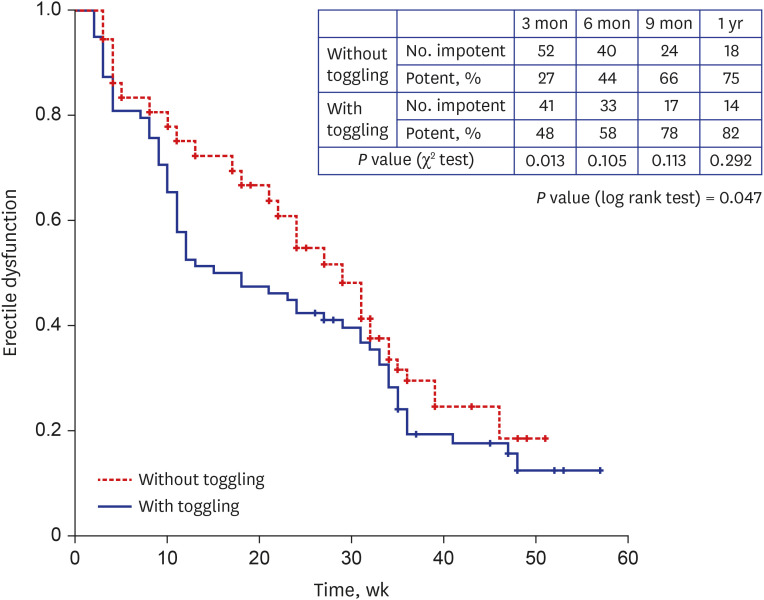 | Fig. 3Kaplan-Meier curve showing erectile dysfunction reduction rate over time. Numbers along the Y-axis represent rate of men at risk (those who were still impotent) at beginning of the corresponding timeline (weeks). Specific percentages depicted in the separate table represent proportion of those men who were potent by the end of the corresponding timeline. |
DISCUSSION
Table 3
Potency outcomes of representative studies after robot-assisted radical prostatectomy (≥ 1 year follow-up)
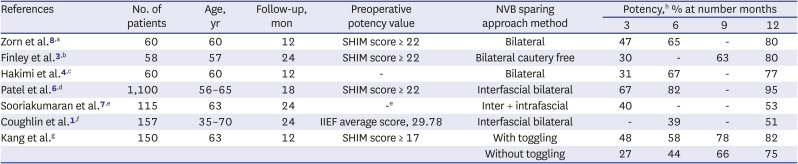
| References | No. of patients | Age, yr | Follow-up, mon | Preoperative potency value | NVB sparing approach method | Potency,h % at number months | |||
|---|---|---|---|---|---|---|---|---|---|
| 3 | 6 | 9 | 12 | ||||||
| Zorn et al.8,a | 60 | 60 | 12 | SHIM score ≥ 22 | Bilateral | 47 | 65 | - | 80 |
| Finley et al.3,b | 58 | 57 | 24 | SHIM score ≥ 22 | Bilateral cautery free | 30 | - | 63 | 80 |
| Hakimi et al.4,c | 60 | 60 | 12 | - | Bilateral | 31 | 67 | - | 77 |
| Patel et al.6,d | 1,100 | 56–65 | 18 | SHIM score ≥ 22 | Interfascial bilateral | 67 | 82 | - | 95 |
| Sooriakumaran et al.7,e | 115 | 63 | 24 | -e | Inter + intrafascial | 40 | - | - | 53 |
| Coughlin et al.1,f | 157 | 35–70 | 24 | IIEF average score, 29.78 | Interfascial bilateral | - | 39 | - | 51 |
| Kang et al.g | 150 | 63 | 12 | SHIM score ≥ 17 | With toggling | 48 | 58 | 78 | 82 |
| Without toggling | 27 | 44 | 66 | 75 | |||||




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download