INTRODUCTION
The hearing aid fitting process involves first making an ear mold to better fixate the device in the ear canal and reduce feedback. Taking an impression of the external auditory canal (EAC) might seem like a simple procedure. However, when done inappropriately, it can cause severe damage, including conductive hearing loss, sensorineural hearing loss, ossicular dislocation, perilymph fistula, vestibular dysfunction, and persistent tympanic membrane (TM) perforation.
1234
Based on data presented in the Korea National Health and Nutrition Examination (2010–2012), the prevalence of mild (over 25 dB) and moderate-to-profound (over 40 dB) hearing loss in adults older than 65 was 69.7% and 36.8%, respectively.
5 The prevalence of hearing impairment increases with age. Adults over the age of 50 frequently show impairment limited to high frequency, and most adults over 60 years old experience impairment across all frequencies. Before the age of 80, the impairment is mild; however, the average hearing of adults over 80 even more decreases to the extent that it corresponds to moderate hearing loss.
567 With one of the world’s fastest aging populations, South Korea is expected to become a superaged society, defined as having more than 21% of citizens 65 years old and older by the WHO within the next 5 years. This implies an inevitable increase in patients with hearing loss. With cochlear implants being performed on just 10% of patients with age-related hearing loss, hearing aids are the predominant treatment method.
89 However, concerns have been raised over the lack of regulation and monitoring of the hearing aid market.
In South Korea, a financial support system for people registered as hearing-disabled was first granted in 1997. In 2015, the amount of financial assistance for hearing aids was significantly raised from $300 per patient to $1,175. According to the National Health and Insurance Sharing Service (NHISS), hearing aid prescriptions and financial assistance requested skyrocketed in 2016 and have been increasing ever since.
10 In 2016 alone, the number of hearing aid prescriptions was 58,235, and government-insured total spending was $60,214,166. This represents a 3.8-fold increase in the number of prescriptions and a 15-fold increase in the funding amount compared to the prior year.
10
According to a press release from the Korean Ministry of Health and Welfare in June 2020, several hearing aid dispensers were caught providing illegal incentives to patients with hearing loss to register themselves as hearing-disabled and buy cheap hearing aids from the dispensers.
101112 These dispensers made profits by reporting inflated prices to the government for the low-quality hearing aids that they sold. In such cases, proper follow-up care was not provided to the patients, leading to unsatisfactory usage and adaptation failure of hearing aids.
12 According to the Korea Consumer Agency’s national consumer helpline, throughout 2013 to 2017, a hearing aid had the largest number (19%) among the medical device-related complaints filed by elderly individuals.
13 The most frequent reasons cited included poor device quality, poor follow-up care, and expensive costs, which indicates the problem of many unprofessional hearing aid shops lacking proper fitting service and knowledge.
With the increase in hearing aid users and insufficient quality control of the system, complications related to hearing aids are expected to have increased as well. However, cases are rarely reported, and there is still no standardized approach to handling such complications. Herein, we report 11 cases of patients who presented with complications from the earmold fitting procedure. The purpose of this study is to share our experience treating patients with earmold material as a foreign body in their ears and to raise awareness of such complications. Based on our analysis of cases and review of the available literature, we suggest clinical guidelines for patients with iatrogenic damage after hearing aid fitting in this paper. We also investigated the South Korean hearing aid market, its sales and distribution network, and policies in place to identify the weaknesses in the system that warrant better quality control.
Go to :

DISCUSSION
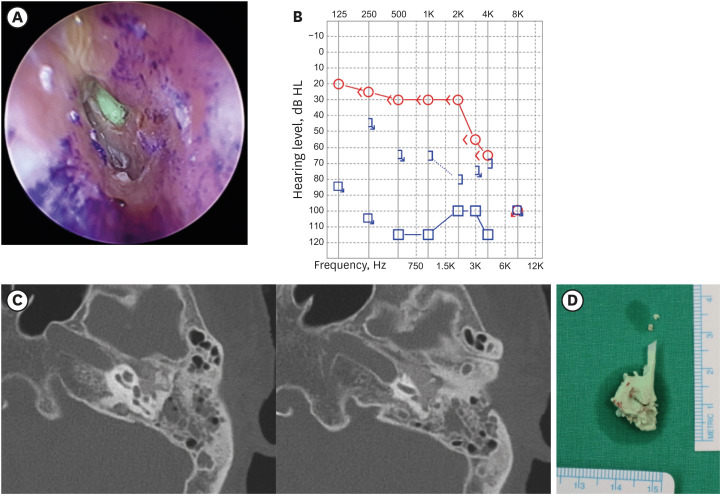
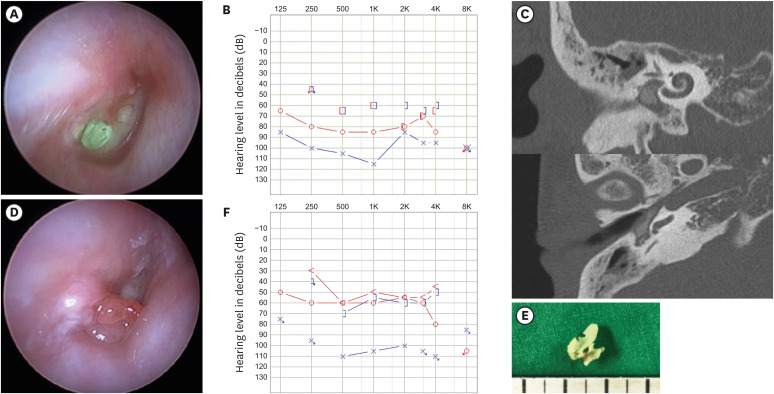
According to the literature, most of the complications related to earmold fitting cases presented symptoms, such as acute otalgia, facial pain, dizziness, and vertigo, all of which should be considered alarming and should have resulted in a referral to an otolaryngologist.
24 Verdam et al.
2 conducted a literature review of 34 cases of impression material entering the middle ear and found that 20 cases reported severe otalgia upon the introduction of the impression material into the EAC. Seven cases of dizziness, three cases of tinnitus, one case of hematorrhea, and one case of facial pain were also reported. These acute onset symptoms may imply that the earmold escapes beyond the otoblock barrier. Therefore, immediate cessation of injection and careful examination by an otolaryngologist are recommended.
2414
High-risk patients should be carefully examined by otolaryngologists before an ear mold impression procedure. Commonly reported features of patients who develop complications after ear mold impression taking were abnormal aural anatomy, such as TM perforation, retraction pocket, or CWD mastoid cavity. Other risk factors include narrow EAC, high facial ridge, deep mastoid bowl, underlying chronic otitis media (COM), history of tympanomastoidectomy, and presence of tympanostomy tubes.
2414 The earmold fitting procedure can be challenging due to the restricted visualization of the TM and EAC, hindering precise positioning of the otoblock and adequate sealing.
214 If the impression material becomes stuck in the ear of these patients, attempting to remove the impression material manually can be dangerous. Hearing aid providers should take extra caution when dealing with patients with these risk factors and refer the patients to an otolaryngologist for a proper examination.
Van den Boer et al.
3 reviewed 49 cases of middle ear foreign bodies to compare different clinical approaches and their outcomes. Among all 12 in-office removal attempts without CT imaging, only one attempt was successful.
3 Blind removal of the mold material has a significant risk of additional damage, including traumatic TM perforation, hematoma, or hemotympanum.
2 However, the nine cases we reviewed imply that some cases without middle ear extension do not necessarily require imaging. One case of blind removal presented with otalgia, but it was mild pain with delayed onset, which was different in character from the alarming symptoms listed above. Safe removal of ear mold material may be achieved by applying local anesthesia in a properly equipped office setting with an appropriate instrument and an ENT specialist if there is no sign of middle ear involvement.
14 In the absence of both patient risk factors and acute symptoms mentioned above, blind removal may be considered. If alarming symptoms such as severe otalgia or dizziness occur in the course of removal, the physician should stop the procedure until the middle ear status is confirmed with a temporal bone CT scan. High-resolution temporal bone CT is highly recommended when the condition of the TM is unknown or middle ear involvement is clinically suspicious.
2 One patient in our series developed TM perforation after EAC foreign body removal. This patient had a history of CWD mastoidectomy, which means CT imaging should have been performed before the removal attempt. High-resolution temporal bone CT scans reveal the extent of foreign body intrusion in relation to critical middle ear structures. It is also needed preoperatively for surgical plans.
12314
Various surgical options for ear mold removal include meatoplasty, middle ear exploration, and tympanoplasty with mastoidectomy.
4 There were no significant differences in outcomes between transcanal and transmastoidal approaches.
3 However, in cases with ossicle involvement, transmastoid facial recess approach is preferred due to better visualization.
34 Proper visualization of the foreign body and surrounding structures is key to successful removal and reducing postoperative complications.
4 A CO
2 laser can help dissect the ossicular chain, allowing removal of the foreign body while sustaining ossicular continuity.
315 Canaloplasty can be useful for reaching the hypotympanum and anterior EAC. CWD mastoidectomy is preferred only for specific cases of chronic inflammation or functionally deaf ears.
3
According to Verdam et al.
2, a favorable audiometric outcome can be achieved in the majority of cases after surgical removal. However, there are postoperative risks of worsening hearing loss, facial nerve injury, semicircular canal injury, and persistent vestibular symptoms.
121416 Delayed referral to an otologic specialist or extensive foreign body invasion into the middle ear may result in unsuccessful and undesired audiologic outcomes.
1
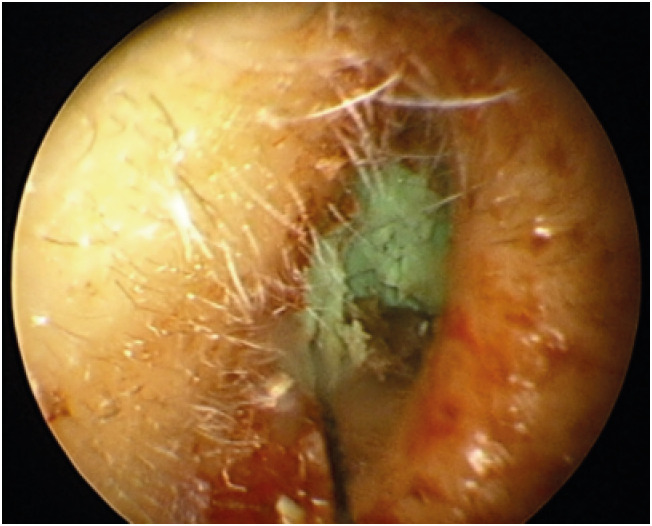
Patients from the two cases involving the middle ear both exhibited similar symptoms as COM: refractory otorrhea and granulation tissue formation. If refractory COM occurs after hearing aid fitting, one should consider ear mold material entering the middle ear as a possible cause. In such cases, CT is the key diagnostic tool.
4 The time of removal after the ear mold fitting procedure ranged from hours to years. In different case reports, a patient showed purulent otorrhea with dizziness five years after an impression mold was taken, and another patient whose impression material was incompletely removed did not experience any symptoms for 9 years.
3 Verdam et al.
2 reported that 4 out of 34 cases presented with delayed-onset symptoms, including persistent otorrhea, TM perforation, and conductive hearing loss, which mimicked COM.
Hearing aid distribution in Korea is entirely dependent on individual providers. Fifty-seven percent of people with hearing loss in Korea bought their hearing aids from private shops without a doctor’s prescription.
4 Per the current South Korean regulations, anyone can provide hearing aids as long as the provider reports the medical device sales business to the government.
48 In the absence of a national standard for hearing aid dispensing licenses, there are many unofficial certificates issued by different licensing authorities, such as Audiologic Testing Service (ATS), Korean Society of Otorhinolaryngology-Head and Neck Surgery, and Acoustical Society of Korea.
8 The requirements to receive the certificates are vastly diverse, and some are obtainable just by passing a single test without a related degree, education, or training. According to the literature, the ATS certificate, the most widely held certificate in South Korea, is held by less than 50% of hearing aid dispensers.
8 In the United States, there is a minimum requirement of education, training, and hands-on experience in the field of hearing rehabilitation for all hearing aid dispensers, although requirement details vary across states.
15
Hearing aids for the hearing disabled covered by national health insurance require an otolaryngologist’s prescription after a comprehensive assessment to determine the suitability of the use. A validation statement ensuring that the device is performing as intended is also requested. These steps are in place to allow patients to receive professional medical attention from otolaryngologists for the best results, to maximize satisfaction with using hearing aids and to prevent inappropriate prescriptions by nonprofessionals. However, there are no policies in place to monitor the procedure of taking an ear impression, preventive measures for high-risk patients, or a referral system for patients who develop complications. The situation is often worse for patients with mild hearing loss who are not registered as disabled because they are not required to be examined by a doctor.
Recently, the Korean government announced a revision of policies that went into effect in July 2020 to improve the quality of fitting hearing aids.
10 As a result, newly registered hearing aid dispensers for hearing-disabled individuals must be otolaryngologists, have received at least 540 hours of education focused on fitting and customization, or have received at least 120 hours of education with over one year of practical experience. They must also be equipped with proper audiometric instruments and a counseling room with a fitting device. This was the first measure legally enforced to limit the qualifications of hearing aid dispensers in Korea, but there is still a long way to go to ensure professional integrity of hearing aid dispensers.
Hearing aid fitting should be performed by medical professionals or well-trained professionals with strict regulations to follow established guidelines. Proper fitting of hearing aids by ENT specialists rarely causes serious complications.
14 Among the two patients with middle ear involvement, the patient from Case 1 had profound hearing loss in the affected ear and serviceable hearing (mild sensorineural hearing loss) in the other, which is an arguable indication for hearing aids. The patient from Case 2 experienced significant damage in her better-hearing ear, which greatly decreased the quality of life. Such unfortunate events could have been avoided by an otolaryngologist’s prompt intervention and involvement.
Complications arise when hearing aid dispensers fail to use a protective otoblock or other material to occlude the EAC or perform an overly pressurized injection of the impression material, causing damage to the TM.
14 Assessment of the EAC and TM with complete visualization and proper placement and sealing of the otoblock is needed.
414 For safe and nontraumatic injection of the impression material, it is important to gradually increase pressure when injecting the impression material. The application device, which is typically a pistol, should not be inserted too deeply.
Ear impression taking procedures should be included in the training of all hearing aid providers, audiologists and hearing aid dispensers. In addition to receiving proper, quality education, they should also be required to complete numerous apprenticeship hours. They should also be trained to immediately refer the patient to an otolaryngologist if any alarming symptoms arise during the procedure. These guidelines should be mandated by law to ensure patient safety and to prevent irreversible harm. In the U.S., it is mandated by federal law that hearing aid dispensers should consult promptly with a licensed physician, an otology specialist, before dispensing hearing aids if the patient exhibits deformity of the ear, otalgia, active otorrhea, dizziness, sudden hearing loss within the previous 90 days, air-bone gap greater than 15 dB, or impacted cerumen.
15 Due to the lack of regulations that require hearing aid providers to immediately refer patients showing alarming symptoms, both patients in Case 1 and Case 2 sought medical attention weeks and months after symptom onset. The hearing aid dispensers argued that they were not at fault, which led to ongoing litigations in Case 1. Guidelines and systematic regulations for referrals should be adopted to minimize such complications through prompt medical intervention.
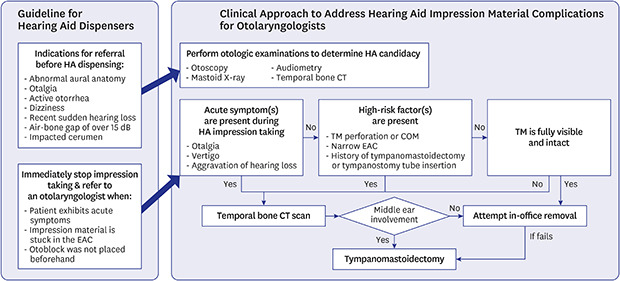
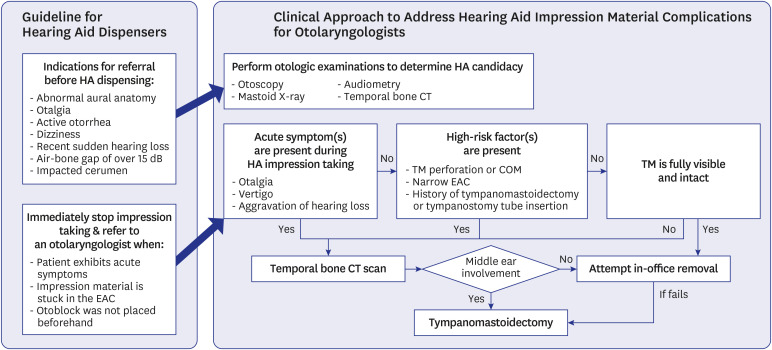
An algorithm for the management of ear foreign body complications due to hearing aid impression material was generated based on a literature review, in addition to our experience (
Fig. 4). All hearing aid sellers should recognize a patient’s previous medical and operation history and adequately perform otoscopic examination, including an evaluation of the EAC and TM. Prescribing and dispensing hearing aids should only be authorized to certified professionals who have received proper education, such as physicians or government-certified audiologists with training in audiometric testing, hearing aid fitting, and follow-up care for the device. Ongoing support and follow-up care by highly qualified specialists are needed to ensure maximum benefit and successful use of hearing aids. Systematic and regulatory changes, such as requiring apprenticeship and raising the required level of education, can help reduce complications. Educated hearing aid dispensers can discern patients who may benefit from evaluation in conjunction with an otolaryngologist. Under the supervision of medical professionals, complications from hearing aid fitting can be significantly avoided.
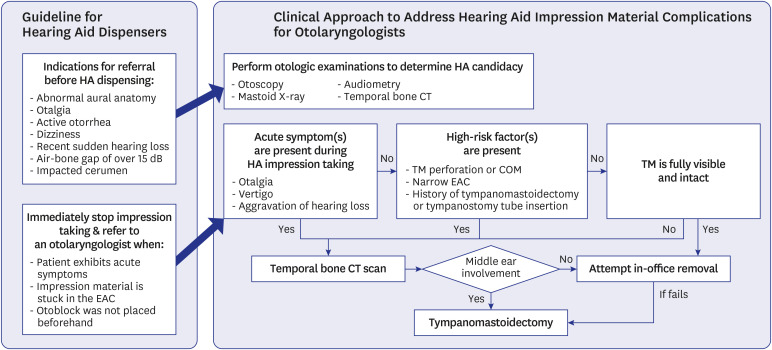 | Fig. 4
A proposed clinical guideline algorithm to address foreign body complications in ears due to hearing aid impression materials.
HA = hearing aid, EAC = external auditory canal, CT = computed tomography, COM = chronic otitis media, TM = tympanic membrane.

|
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download