1. Holm JE, Holroyd KA. The daily hassles scale (revised): does it measure stress or symptoms? Behav Assess. 1992; 4(3-4):465–482.
2. American Psychological Association. Stress in America: the State of our Nation. Washington, D.C., USA: American Psychological Association;2017.
3. Nipp RD, El-Jawahri A, Fishbein JN, Eusebio J, Stagl JM, Gallagher ER, et al. The relationship between coping strategies, quality of life, and mood in patients with incurable cancer. Cancer. 2016; 122(13):2110–2116. PMID:
27089045.

4. Parker PD, Jerrim J, Anders J. What effect did the global financial crisis have upon youth wellbeing? Evidence from four Australian cohorts. Dev Psychol. 2016; 52(4):640–651. PMID:
26854968.

5. di Tella R, MacCulloch RJ, Oswald AJ. The macroeconomics of happiness. Rev Econ Stat. 2003; 85(4):809–827.

6. Yun YH, Sim JA, Jung JY, Noh DY, Lee ES, Kim YW, et al. The association of self-leadership, health behaviors, and posttraumatic growth with health-related quality of life in patients with cancer. Psychooncology. 2014; 23(12):1423–1430. PMID:
24844184.

7. Covey SR. The 7 Habits of Highly Effective People: Powerful Lessons in Personal Change. New York, NY, USA: Simon and Schuster;2013.
8. McCorkle R, Ercolano E, Lazenby M, Schulman-Green D, Schilling LS, Lorig K, et al. Self-management: enabling and empowering patients living with cancer as a chronic illness. CA Cancer J Clin. 2011; 61(1):50–62. PMID:
21205833.

9. Kang E, Kim S, Rhee YE, Lee J, Yun YH. Self-management strategies and comorbidities in chronic disease patients: associations with quality of life and depression. Psychol Health Med. 2021; 26(8):1031–1043. PMID:
33095059.

10. Suzuki M, Furihata R, Konno C, Kaneita Y, Ohida T, Uchiyama M. Stressful events and coping strategies associated with symptoms of depression: a Japanese general population survey. J Affect Disord. 2018; 238:482–488. PMID:
29933216.

11. Perrin M, Vandeleur CL, Castelao E, Rothen S, Glaus J, Vollenweider P, et al. Determinants of the development of post-traumatic stress disorder, in the general population. Soc Psychiatry Psychiatr Epidemiol. 2014; 49(3):447–457. PMID:
24022753.

12. Grunfeld E, Levine MN, Julian JA, Coyle D, Szechtman B, Mirsky D, et al. Randomized trial of long-term follow-up for early-stage breast cancer: a comparison of family physician versus specialist care. J Clin Oncol. 2006; 24(6):848–855. PMID:
16418496.

13. Cosco TD, Kaushal A, Richards M, Kuh D, Stafford M. Resilience measurement in later life: a systematic review and psychometric analysis. Health Qual Life Outcomes. 2016; 14(1):16. PMID:
26821587.

14. Park SM, Lim MK, Jung KW, Shin SA, Yoo KY, Yun YH, et al. Prediagnosis smoking, obesity, insulin resistance, and second primary cancer risk in male cancer survivors: National Health Insurance Corporation Study. J Clin Oncol. 2007; 25(30):4835–4843. PMID:
17947733.
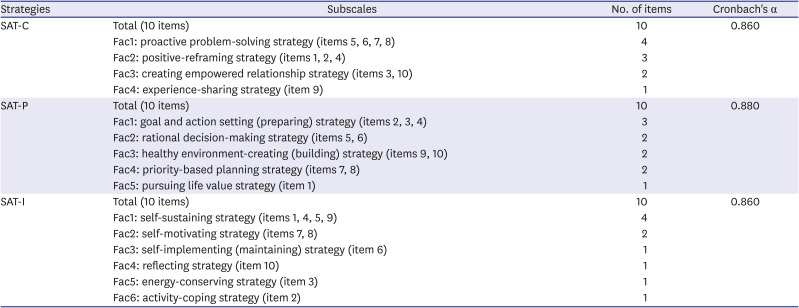
15. Yun YH, Jung JY, Sim JA, Choi H, Lee JM, Noh DY, et al. Patient-reported assessment of self-management strategies of health in cancer patients: development and validation of the Smart Management Strategy for Health Assessment Tool (SAT). Psychooncology. 2015; 24(12):1723–1730. PMID:
26014043.

16. Covey SR. The 7 Habits of Highly Effective People. New York, NY, USA: Free Press;2004.
17. Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med. 1997; 4(1):92–100. PMID:
16250744.
18. Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996; 9(3):455–471. PMID:
8827649.

19. Yun YH, Jung JY, Sim JA, Lee J, Noh DY, Han W, et al. Development and validation of the smart management strategy for health assessment tool-short form (SAT-SF) in cancer survivors. Qual Life Res. 2018; 27(2):347–354. PMID:
29086167.

20. Levy PS, Lemeshow S. Sampling of Populations: Methods and Applications. 4th ed. Hoboken, NJ, USA: Wiley;2013.
21. Yun YH, Sim JA. The validity of the smart management strategy for health assessment tool-life (SAT-Life) in general population. Res Square. Forthcoming. 2020; DOI:
10.21203/rs.3.rs-28834/v1.

22. Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932; 22(140):5–55.
23. Kim SH, Jo MW, Ahn J, Ock M, Shin S, Park J. Assessment of psychometric properties of the Korean SF-12 v2 in the general population. BMC Public Health. 2014; 14(1):1086. PMID:
25326684.

24. Santos IS, Tavares BF, Munhoz TN, Almeida LS, Silva NT, Tams BD, et al. Sensitivity and specificity of the Patient Health Questionnaire-9 (PHQ-9) among adults from the general population. Cad Saude Publica. 2013; 29(8):1533–1543. PMID:
24005919.
25. Han C, Jo SA, Kwak JH, Pae CU, Steffens D, Jo I, et al. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Compr Psychiatry. 2008; 49(2):218–223. PMID:
18243897.

26. Shin HW, Noh DY, Lee ES, Nam SJ, Park BW, Ahn SH, et al. Correlates of existential well-being and their association with health-related quality of life in breast cancer survivors compared with the general population. Breast Cancer Res Treat. 2009; 118(1):139–150. PMID:
19191021.

27. Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985; 49(1):71–75. PMID:
16367493.

28. Yun YH, Sim JA, Park EG, Park JD, Noh DY. Employee health behaviors, self-reported health status, and association with absenteeism: comparison with the general population. J Occup Environ Med. 2016; 58(9):932–939. PMID:
27513170.
29. Elvén M, Hochwälder J, Dean E, Hällman O, Söderlund A. Criterion scores, construct validity and reliability of a web-based instrument to assess physiotherapists' clinical reasoning focused on behaviour change: ‘Reasoning 4 Change’. AIMS Public Health. 2018; 5(3):235–259. PMID:
30280115.

30. Fayers P, Aaronson NK, Bjordal K, Sullivan M. EORTC QLQ-C30 Scoring Manual. Brussels, Belgium: European Organisation for Research and Treatment of Cancer;1995.
31. Wang J, Patten SB. The moderating effects of coping strategies on major depression in the general population. Can J Psychiatry. 2002; 47(2):167–173. PMID:
11926079.

32. Fernandez A, Garcia-Alonso J, Royo-Pastor C, Garrell-Corbera I, Rengel-Chica J, Agudo-Ugena J, et al. Effects of the economic crisis and social support on health-related quality of life: first wave of a longitudinal study in Spain. Br J Gen Pract. 2015; 65(632):e198–e203. PMID:
25733442.

33. Elder GH, Caspi A. Economic stress in lives: developmental perspectives. J Soc Issues. 1988; 44:25–45.

34. Elder GH. Children of the Great Depression: Social Change in Life Experience. New York, NY, USA: Routledge;2018.
35. Meng X, D'Arcy C. Coping strategies and distress reduction in psychological well-being? A structural equation modelling analysis using a national population sample. Epidemiol Psychiatr Sci. 2016; 25(4):370–383. PMID:
26077164.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download