INTRODUCTION
Since the Internal Organs, etc. Transplant Act was enacted in 1999, the number of deceased organ tissue donations (OTD) steadily increased to 573 until 2016, but has been declining since 2017 in Korea.
1 Contrarily, the number of people waiting for transplantation has increased yearly from 2,840 people in 2000 to 32,990 in 2019 according to the Korean Organ Donation Agency (KODA) annual report.
2 This is a serious problem for OTD.
Since February 2018, it has been possible to legally suspend or stop life-sustaining treatment (LST), such as cardiopulmonary resuscitation and mechanical ventilation, for end-of-life patients due to the Decisions on Life-Sustaining Treatment for Patients in Hospice and Palliative Care or at the End-of-life Act (the LST Decision Act) in Korea.
3 In the process of discontinuing LST, there may be less opportunity to consider brain death and organ donation.
4 In the end, the notification of brain death by estimators has decreased, affecting the rate of OTD. In particular, it is unclear whether cessation of LST for potentially brain-dead patients accelerates death and whether such an action is legally problematic.
5
When a brain-dead patient is notified to the KODA, the coordinator confirms the patient’s medical condition, contacts the guardian, and finally, obtains the guardian’s consent. Although the total number of notifications has increased, the final consent rate has steadily decreased from 51.7% in 2015 to 33.0% in 2019.
2 This overlaps with the passage of the LST Decision Act, which may have had an influence. In a previous study analyzing the KODA 2013-2018 annual reports, a reason suggested for the decrease in donations was the tendency of families of brain-dead patients to give up LST due to the enforcement of the LST Decision Act.
6 As the donations decreased despite the increase in the number of patients, family consent had a major impact. It was suggested that the implementation of the LST Decision Act had the greatest impact. A study by Cho also mentions the LST decision system as a cause of the decrease in donations. Currently, when patients give an advanced directive for LST and registered their wish to donate organs, the systems conflict because there is no national consensus on which decision should take precedence and the order in which to proceed. Additionally, there is a lack of education for medical staff.
4
In Korea, the number of emergency physicians (EPs) is second only to that of neurosurgeons among the medical staff notifying suspected brain death.
2 The number of organ donations through EPs increased from 49 in 2015 to 144 in 2019.
2 In clinical practice, the role of EPs in identifying potential brain-death in patients and linking them to donors is growing. In the United States, Australia, and the United Kingdom, policy statements were made at the academic level, highlighting the significant role EPs play in the process of discovery of brain-dead individuals and subsequent OTD.
789
Emergency departments (ED) operate 24-hour shifts to provide emergency care. When patients with severe trauma, a need for cardiopulmonary resuscitation, or whose lives are in jeopardy due to a drug overdose or hanging for suicide, are brought to the ED, the EPs examine the suspected brain-dead patient. Additionally, the EDs of tertiary hospitals in Korea directly admit these critically ill patients to the intensive care unit for treatment. With the enforcement of the LST Decision Act in 2018, LST for patients with no possibility of regaining consciousness in the intensive care unit is also suspended. As a result, EPs examine both the suspected brain-dead patients and patients in whom LST is stopped, which potentially lead to OTD.
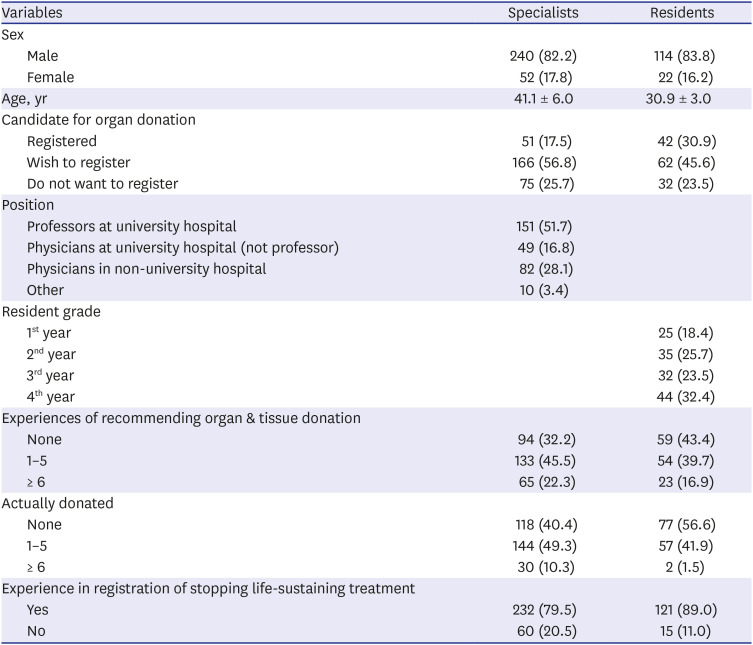
Depending on the physicians’ experience or knowledge of deceased OTD, attitude towards it, and perceptions of withdrawal of stopping LST, physicians will vary in their organ donation recommendations to the patient’s guardian. They will also differ in the degree of notification of a brain death determination. Therefore, in this study, we sought firstly to investigate the knowledge and attitudes towards deceased OTD. Secondly, we compared the differences according to the characteristics of the respondents. Thirdly, we analyzed the factors affecting attitudes toward deceased OTD according to the characteristics of EPs. By understanding this, we intend to identify ways to encourage more organ donation.
METHODS
This study was a cross-sectional online survey, conducted using SurveyMonkey
® (
https://en.surveymonkey.com) in December 2020. The questionnaire link was distributed using the emails of regular members (specialists) and associate members (residents) of the Korean Society of Emergency Medicine. When the survey was conducted, 2,168 regular members and 590 associate members were registered with the society. The calculated sample size for this study was 337 at a 95% confidence level and 5% margin of error.
Survey tools
Since there were no validated survey tools for EPs or medical doctors in Korea, questionnaires were created using material from existing studies. In the study of knowledge and attitudes toward organ donation in Korea, the questionnaire items from 2 master’s thesis written in Korean, mainly targeting university students and nurses, were used as drafts.
1011 The questionnaire used in a study by Lee after the 2018 enactment of the LST Decision Act on attitudes toward stopping LST was also used as a draft.
12 The 3 questionnaire tools on knowledge and attitudes toward organ donation and attitudes toward stopping LST mainly targeted nurses. As these are not recent studies, the questionnaire items were reviewed for validity. Seven specialist doctors and 9 nurses with extensive experience in organ donation and stopping LST were asked to rate on a 5-point Likert scale (where 5 indicated very valid and 1 indicated very invalid) how appropriate the items were for evaluating the knowledge and attitude of EPs. Additionally, they were asked to indicate what they thought should be consolidated, deleted, or corrected. After two surveys of experts, the final questionnaire items were constructed. The section on the knowledge of deceased OTD contained 19 questions. There were 5 questions on legal knowledge, 2 on the definition of brain death, 9 on the conditions and procedure for organ donation, 1 on managing brain-dead organs, and 2 on medical knowledge. A correct answer earned 1 point, and an incorrect or unknown answer earned 0 points. A higher knowledge score indicated more knowledge. The section on attitudes toward deceased OTD contained 16 questions, covering cognitive, emotional, and behavioral aspects. Respondents were asked to rate on a 5-point scale. The higher the attitude score, the more positive is the attitude toward OTD. Attitudes toward stopping LST were assessed with 13 questions on a 5-point scale. The higher the attitude score, the more positive they were to stopping LST (
Supplementary Table 1).
We also collected information on the respondents’ gender, age, status (specialist or resident), whether they were registered as an organ/tissue donor, position in the hospital, resident grade, experience of organ donation solicitation and actual organ donation, education provided by KODA, and experience of withdrawal of LST.
Statistical analysis
Descriptive analysis was used for the basic demographics of respondents. T-tests, analysis of variance with Scheffe (post hoc analysis), and χ2-tests were conducted to investigate the differences in knowledge and attitude toward deceased OTD according to the characteristics of respondents. Pearson’s correlation coefficient analysis was conducted to examine the relationship between knowledge and attitudes toward deceased OTD and attitudes toward stopping LST. Stepwise hierarchical multiple regression analysis was performed to investigate the variables affecting the attitudes toward deceased OTD. To explore the factors influencing attitudes toward deceased OTD, a 2-stage hierarchical regression analysis was conducted. We used individual characteristic variables (sex, organ donation registration intention, specialist or resident, organ donation experience, organ donation education) and independent variables for knowledge on deceased OTD and attitudes toward stopping LST. In step 1, individual characteristics were analyzed as dummy variables. Knowledge of deceased OTD and attitudes toward stopping LST were put into the 2-step regression equation. We checked the tolerance and variance inflation factor (VIF) statistics to identify problems with multicollinearity of the predictors. The tolerance value of 0.20 or higher, VIF value less than 10, and Durbin–Watson value of 2.071, close to 2, confirmed that there was no multicollinearity. IBM SPSS ver. 23.0 software (IBM Corp., Armonk, NY, USA) was used for the analyses; significance was set at P < 0.05.
Ethics statement
The present study was reviewed and approved by the Institutional Review Board of Yonsei University Wonju Christian Severance Hospital (approval No. CR320149). Informed consent was obtained from all participants at the time of the survey.
DISCUSSION
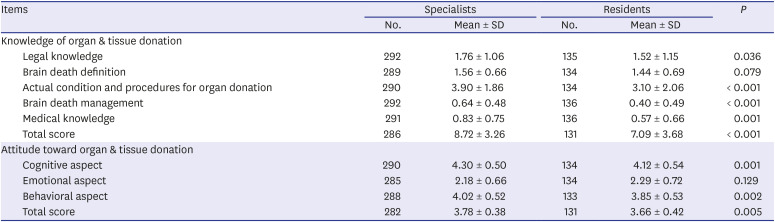
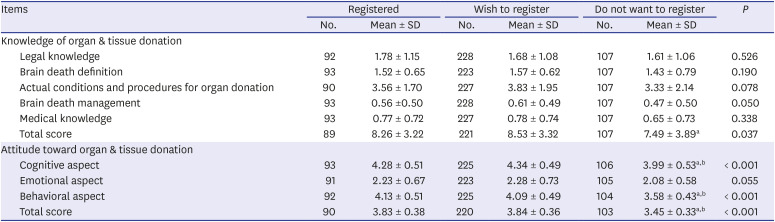
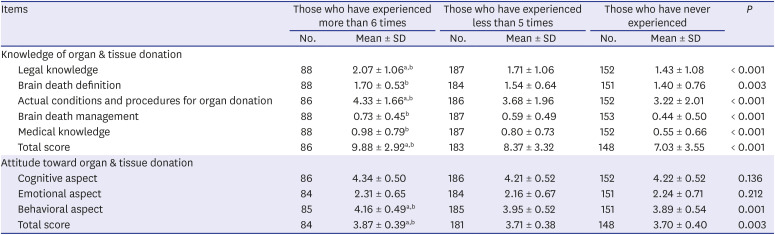
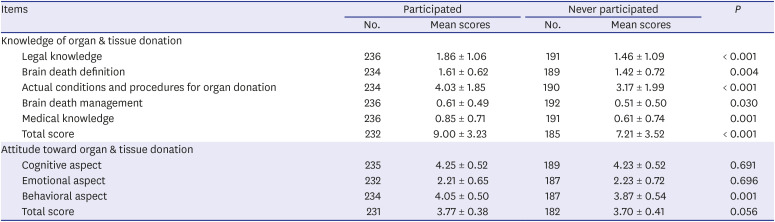
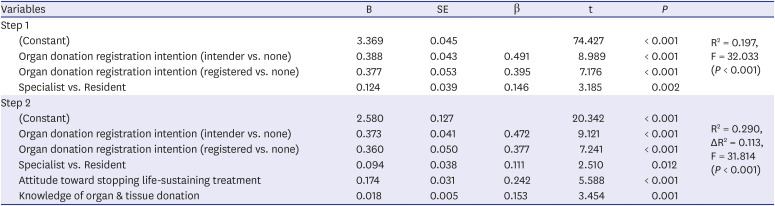
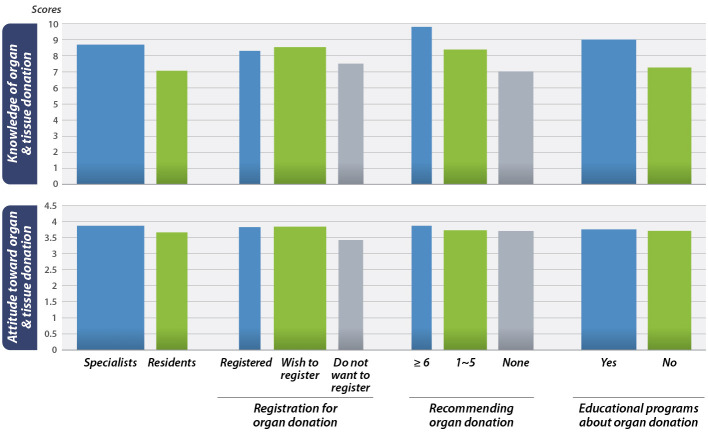
In this study, differences in knowledge and attitudes on deceased OTD were investigated according to the characteristics of EPs. Deceased OTD knowledge and attitude scores were higher in specialists or respondents who were registered as donors or intended to donate organs. Those who had experience soliciting organ donation and those who received KODA’s OTD education had higher deceased OTD knowledge scores. Additionally, regarding factors influencing attitudes toward deceased OTD, specialists, those who wished to donate or had registered as organ donors, and those with a higher stopping LST attitude score and knowledge about deceased OTD had a more positive attitude.
According to Siminoff et al.,
1314 the positive attitude of healthcare professionals toward organ donation may affect the processes of organ donation and consent acquisition from caregivers. Studies have reported that when potential organ donation recipients are notified in the ED, there is a high probability that the organ donation will proceed successfully.
151617 Therefore, the advantage of this study is that we investigated EPs’ responses regarding factors related to attitude toward deceased OTD. This has not been previously reported in Korea. It is also significant because this study reported the correlation between the attitudes toward stopping LST and deceased OTD, which can affect the notification of brain-death estimates.
Although the gap was not large, specialists were more knowledgeable and had more positive attitudes toward deceased OTD than residents. This may be due to specialists having relatively longer clinical experience and experience related to brain death decisions or OTD procedures than residents. Those who have already registered as donors or wish to donate might have a high interest in donation, which seems to have led to a higher organ and tissue donation-related knowledge score and a more positive attitude toward deceased OTD. In a survey of EPs in Canada, it was reported that those who expressed their intention to be a donor were 5.8 times more likely to refer potential donors than those who did not.
18 Emergency medicine specialist, and more than 10 years of working experience were also reported as factors related to referral for organ donation.
18 Although only 2.8% responded that negative attitudes toward OTD could be a barrier, the above results suggest that clinicians’ values can influence the decision-making process of OTD.
18 In this study, individual characteristics, such as registration, intent to donate, or specialist status, were related to a positive attitude toward deceased OTD. These factors may affect the procedure for deceased OTD referral. Due to the fact that specialists have a more positive attitude toward deceased OTD than residents, it is necessary that specialists actively participate in the treatment and referral process for suspected brain-dead patients.
Those who have donation solicitation experience and education on OTD have a high organ donation knowledge score as they have encountered information about organ donation procedures. Although the attitude score in the behavioral aspect was higher in individuals who have prior education, previous education itself was excluded from the factors related to the attitude toward deceased OTD in this study. However, in the Canadian EPs study, the clinician’s unfamiliarity with the organ donation procedure was the biggest perceived barrier to organ donation.
18 Additionally, it was reported that EPs who received organ donation education had a high organ donation request rate.
1819 In the UK, since most donors are ED patients who die in intensive care units due to brain injury, the National Health System published the “Organ Donation and the Emergency Department. A strategy for implementation of best practice.” The strategy includes organ donation specialist nurses providing regular training to key medical staff in EDs, as EPs are important for donor discovery.
9 Approximately 55.6% of the respondents had prior education on OTD. The knowledge mean score related to the OTD was 8.72 ± 3.26 for specialists and 7.09 ± 3.68 for residents out of a total of 19 points, indicating that the relevant knowledge and prior education were insufficient. Therefore, improving legal knowledge and knowledge of organ donation procedures through regular education for EPs in Korea is recommended. An educational program connected with the academic level or maintenance education should be organized, and the content should be included in the residents’ training curriculum.
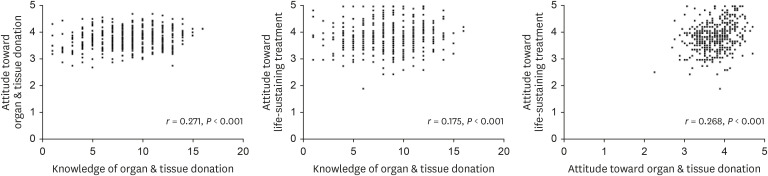
The stopping LST attitude score was correlated with the knowledge and attitude toward deceased organ and tissue donation in our study. According to a survey of healthcare professionals and workers in a Korean tertiary hospital, there was a significant positive correlation between the attitudes towards organ donation and the knowledge and perception of hospice palliative care.
20 This is consistent with the results of this study. However, we should be cautious in assuming that a more positive attitude toward stopping LST results in a more positive attitude toward OTD. In fact, in previous domestic studies, one of the causes of the decrease in brain-dead organ donation was the tendency of the family of the brain-dead potential donor to decide to withdraw or withhold LST after the enactment of the life-sustaining treatment decision law.
45 In our study, the positive correlation between the attitude scores for the opposing situations can be explained by the fact that EPs deal with both situations in the process of treating patients. In other words, they seem to have a positive attitude toward both situations because they think and decide both situations in the best interest of the patient. Overseas, the organ donation procedures are linked with the clinician’s awareness of the possibility of organ donation in the process of deferring end-of-life care or stopping LST.
212223 The Australian College of Emergency Medicine publishes and revises the document stipulating the role of EPs in the donation process every 3 years. If a suspected brain death occurs in the ED, the patient is admitted to the intensive care unit, where the medical staff must contact the department or staff responsible for OTD before stopping the patient’s LST.
8 Therefore, unlike the domestic situation where 2 conflicting medical decisions are being dealt with separately, a process is needed to determine the possibility of organ or tissue donation before LST is discontinued, as is done in the EDs of foreign systems. To improve the recent decrease in deceased OTD in Korea, policy and institutional measures that can simultaneously address organ donation in the process of making LST decisions should be discussed.
This study has the following limitations. First, the survey’s response rate was 15.5%. The survey’s response rate was lower for specialists than for residents, which may act as a potential bias. Second, because the questionnaire items were made based on those for nurses, there is a possibility that the attitudes of EPs could not be accurately evaluated. In addition, as the attitude toward stopping LST was evaluated with the questionnaire items devised before the implementation of the LST Decision Act, the clinical situations after implementation may not be actually reflected. Third, a socially desirable bias may occur when measuring attitudes, as respondents tend to provide responses in a positive direction.
24 Whether positive attitude scores lead to actual behavior changes should be evaluated through a qualitative study using interviews. Fourth, the reason for the lack of deceased OTD in Korea includes factors other than the doctors, such as donation refusal, non-brain death, and incompatible donors.
625 However, since such factors were not addressed in this study, understanding the factors affecting physicians’ attitudes toward deceased organ donation in clinical situations may be limited. Lastly, the questionnaire items used in this study were all questions reflecting the Korean system and medical environment, and were based on the thesis in Korean. Therefore, in countries with different medical systems or environments, the results of the study should be generalized with caution.
In conclusion, emergency medicine specialists, those who had registered or wished to be organ donors, and those who had higher knowledge score regarding deceased OTD, and higher attitude scores toward stopping LST were more positive toward deceased OTD. For more potential deceased OTD donors to be referred, continuous educational efforts toward increased deceased OTD-related knowledge and better procedures for EPs should be provided. In addition, when deciding on the withdrawal of LST, there is a need for institutional or systemic improvements that can lead to organ donation.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download