Scabies is a tropical disease caused by the mite
Sarcoptes scabiei that affects 300 million individuals annually.
1 The prevalence of scabies in Korea increases with age, and it is peaked at 3.0 to 4.1 per 1,000 people over 80 years old.
2 It can be spread via direct or indirect transmission in the medical environment.
3 Scabies infection can increase morbidity in elderly patients through secondary bacterial infection.
4 It can cause an outbreak and occasionally lasts for a couple of months.
5 Tracking contacts, and post-exposure treatment requires a considerable cost and inconvenience.
67 Meticulous suspicion and early diagnosis are required to prevent scabies from entering a medical institution. Although pruritus is the main symptom of scabies, sometimes skin symptom is non-specific in elderly patients, and sometimes it is difficult to communicate with elderly patients to get a subjective complaint.
8 Moreover, itching or skin lesions were not significant factors in detecting scabies.
9 Therefore, finding risk factors for scabies infection in a medical environment at the time of patients' admission is necessary. However, there was limited information regarding risk factors for scabies in the acute medical environment in Korea. This study evaluated risk factors of scabies based on the status at the time of admission in various clinical aspects, including symptoms and skin lesions.
This study is a case-control study. Scabies cases were collected from data of the infection control team of an acute-care teaching hospital in Korea between January 2008 and December 2019. Scabies was diagnosed by microscopic identification of the mite or mite eggs by a dermatologist from scraped skin. Suspicion and diagnosis of scabies were made by clinical suspicion by the attending physician and referral to a dermatologist. The control group was selected from the same hospital at a ratio of two controls for every one scabies case. To match the scabies group and control group similarly, independent of the patients' medical status at the admission date, we selected controls as a person who had the same sex and age and were hospitalized on the same day as the case. When no patient was the same sex and age as the case, a patient hospitalized on the closest day before or after the case's admission date was selected.
Clinical information and laboratory data were retrospectively collected from the electrical medical record system. We investigated admission status (admission route, intensive care unit admission), date of scabies diagnosis, history of scabies, previous admission to a long-term care facility within 1 year, previous corticosteroid use (more than prednisolone 20 mg/day in any duration), immunosuppressed status, medical history of chronic diseases (hypertension, diabetes mellitus, malignancy, dementia etc.), catheter indwelling status, skin lesion or itching sensation, and laboratory results of white blood count, hemoglobin, albumin, creatinine, C-reactive protein, erythrocyte sedimentation rate. Laboratory results in the period of one week before or after the admission day were collected.
The χ2 or Fisher's exact test was conducted to compare the distribution of categorical variables, and t-test was conducted to compare the mean of continuous variables. Then with significantly different variables, a logistic regression model was designed to elucidate independent risk factors. Variables were selected from those that showed a significant difference in univariate analysis, except for variables with many missing values and variables expected to have multicollinearity. In the process of selecting variables for multivariate analysis, albumin and C-reactive protein level were excluded as a variable that was difficult to interpret and apply due to their nonspecific nature. Previous steroid use was excluded due to the small absolute number, and skin lesions and itching were excluded because there was a possibility that bias occurred due to under-detection in the control group. Variables with a P value of < 0.05 were considered to be statistically significant. All statistical analyses were performed using SPSS (IBM SPSS statistics for Windows, version 27.0; IBM Corp., Armonk, NY, USA).
A total of 35 cases of scabies infection were diagnosed during the study period. One case in the outpatient clinic was excluded. Then 34 cases were finally analyzed in the study. Annually, there was a median of 2.5 cases (ranged, 0–11 cases) of scabies infection between 2008 and 2019 (
Supplementary Fig. 1A). Although the number of scabies cases varied by month (
Supplementary Fig. 1B), it was similar by season (9 in spring, 8 in summer, 9 in fall, 8 in winter, respectively). Scabies infection was diagnosed in a median of 10 days (interquartile range, 5–42 days) after admission (
Supplementary Fig. 1C). Exposure was confirmed in a median of 19 (ranged, 0–51) patients or health care personnel by epidemiological investigation to prevent further transmission.
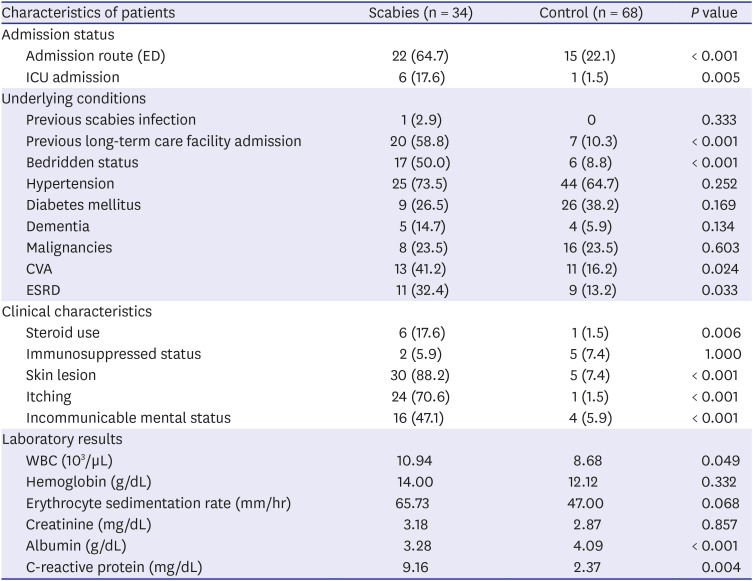
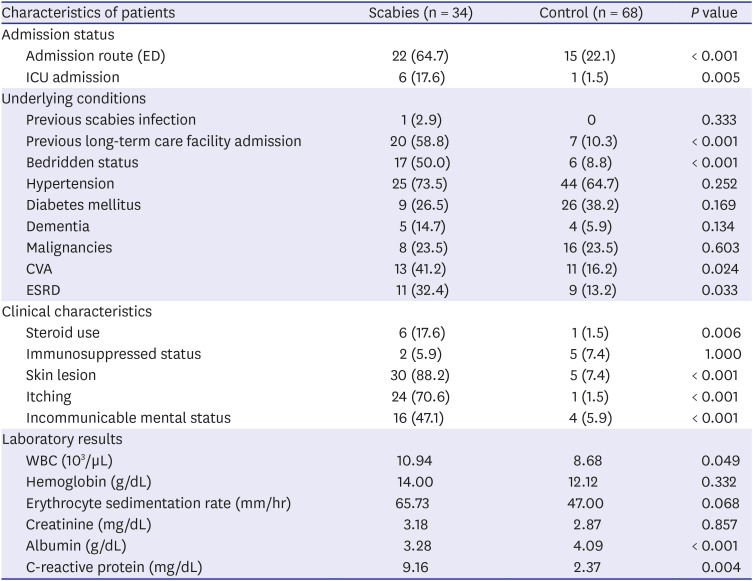
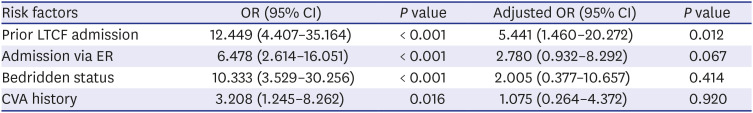
Scabies group had 17 men and 17 women. Mean age was 61 years (range, 31–96 years). Compared to the control group, there were more cases of admission via the emergency department in the scabies group (64.7% vs. 22.1%,
P < 0.001,
Table 1). Previous scabies infection was only in the scabies group (2.9%) and not in the control group. Long-term care facility admission history was more in the scabies group although the difference was not significant (58.8% vs. 10.3%;
P < 0.001). In the scabies group, more were admitted to the intensive care unit, and they had more indwelling catheters (17.6% vs. 1.5%;
P = 0.005, 61.8% vs. 19.1%;
P = 0.069, respectively). Scabies group had a higher prevalence of hypertension, dementia, and end-stage renal disease (73.5% vs. 64.7%;
P = 0.252, 14.7% vs. 5.9%;
P = 0.134, 32.4% vs. 13.2%;
P = 0.033, respectively). Scabies group had more ischemic or hemorrhagic cerebrovascular accident, were more incommunicable, and had higher proportion of bedridden status (41.2% vs. 16.2%;
P = 0.024, 47.1% vs. 5.9%;
P < 0.001, 50.0% vs. 8.8%;
P < 0.001, respectively). The scabies group showed more skin lesions and itching symptoms (88.25% vs. 7.4%;
P < 0.001, 70.6% vs. 1.5%;
P < 0.001). Regarding medication, scabies group used more corticosteroid than control group (17.6% vs. 1.5%;
P = 0.006). There was no significant difference in the proportion of immunosuppressed patients.
Table 1
Characteristics comparison of scabies group and control group in a hospital environment
|
Characteristics of patients |
Scabies (n = 34) |
Control (n = 68) |
P value |
|
Admission status |
|
|
|
|
Admission route (ED) |
22 (64.7) |
15 (22.1) |
< 0.001 |
|
ICU admission |
6 (17.6) |
1 (1.5) |
0.005 |
|
Underlying conditions |
|
|
|
|
Previous scabies infection |
1 (2.9) |
0 |
0.333 |
|
Previous long-term care facility admission |
20 (58.8) |
7 (10.3) |
< 0.001 |
|
Bedridden status |
17 (50.0) |
6 (8.8) |
< 0.001 |
|
Hypertension |
25 (73.5) |
44 (64.7) |
0.252 |
|
Diabetes mellitus |
9 (26.5) |
26 (38.2) |
0.169 |
|
Dementia |
5 (14.7) |
4 (5.9) |
0.134 |
|
Malignancies |
8 (23.5) |
16 (23.5) |
0.603 |
|
CVA |
13 (41.2) |
11 (16.2) |
0.024 |
|
ESRD |
11 (32.4) |
9 (13.2) |
0.033 |
|
Clinical characteristics |
|
|
|
|
Steroid use |
6 (17.6) |
1 (1.5) |
0.006 |
|
Immunosuppressed status |
2 (5.9) |
5 (7.4) |
1.000 |
|
Skin lesion |
30 (88.2) |
5 (7.4) |
< 0.001 |
|
Itching |
24 (70.6) |
1 (1.5) |
< 0.001 |
|
Incommunicable mental status |
16 (47.1) |
4 (5.9) |
< 0.001 |
|
Laboratory results |
|
|
|
|
WBC (103/µL) |
10.94 |
8.68 |
0.049 |
|
Hemoglobin (g/dL) |
14.00 |
12.12 |
0.332 |
|
Erythrocyte sedimentation rate (mm/hr) |
65.73 |
47.00 |
0.068 |
|
Creatinine (mg/dL) |
3.18 |
2.87 |
0.857 |
|
Albumin (g/dL) |
3.28 |
4.09 |
< 0.001 |
|
C-reactive protein (mg/dL) |
9.16 |
2.37 |
0.004 |

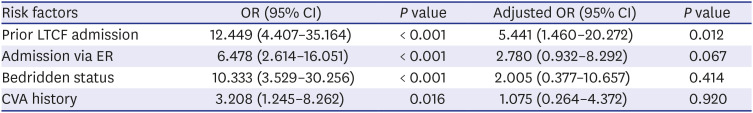
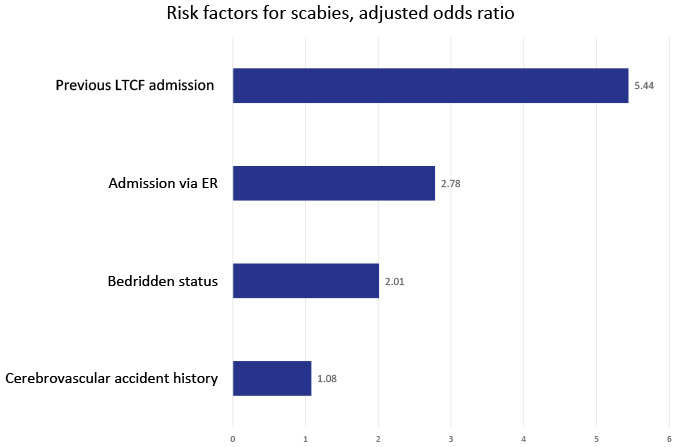
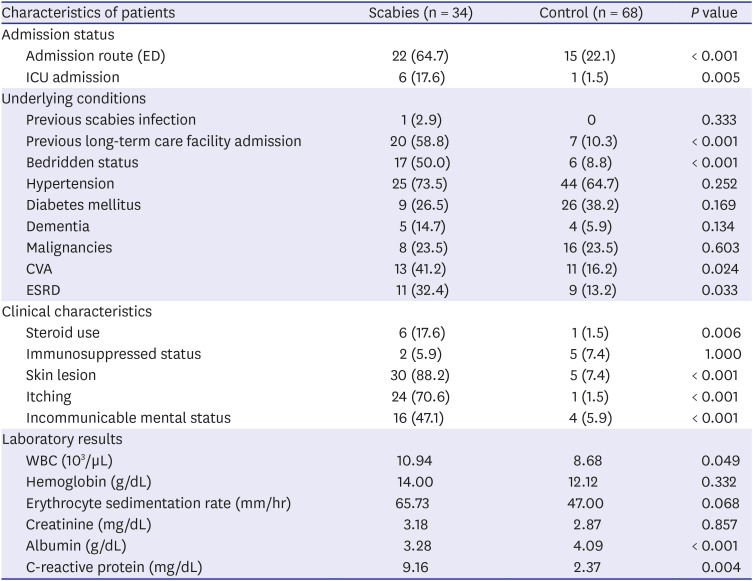
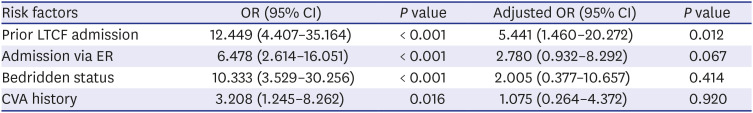
After adjusting other variables' effect, previous long-term care facility admission was associated significantly with scabies (adjusted odds ratio, 5.441; 95% confidence interval, 1.460–20.272;
P = 0.012;
Table 2).
Table 2
Risk factors for scabies
|
Risk factors |
OR (95% CI) |
P value |
Adjusted OR (95% CI) |
P value |
|
Prior LTCF admission |
12.449 (4.407–35.164) |
< 0.001 |
5.441 (1.460–20.272) |
0.012 |
|
Admission via ER |
6.478 (2.614–16.051) |
< 0.001 |
2.780 (0.932–8.292) |
0.067 |
|
Bedridden status |
10.333 (3.529–30.256) |
< 0.001 |
2.005 (0.377–10.657) |
0.414 |
|
CVA history |
3.208 (1.245–8.262) |
0.016 |
1.075 (0.264–4.372) |
0.920 |

This study showed the characteristics of scabies patients at the admission date in a nosocomial environment compared to a control group. We identified that previous long-term care facility admission was significantly associated with scabies infection in those patients. Patients with scabies infection were more incommunicable, bedridden, and had a more medically severe status, although these variables were not significant after adjustment. In this study, variables that can be used for screening early in hospitalization were examined so that scabies could be suspected early after hospitalization. Furthermore, factors that can be easily identified in the clinical environment were considered. Although several variables were considered, the variable that can be usefully confirmed in the clinical field was the history of long-term care facility admission.
Long-term care facility was associated in previous research, albeit the circumstances were different according to the country. In Taiwan, living in a nursing home was confirmed as a risk factor for scabies in a tertiary hospital with bedridden status, indwelling catheter, and clinical severe status.
10 In Japan, rapid turnover of patients was a risk factor among psychiatric and long-term care hospitals.
11 Dementia history was a risk factor in another report from Japan. Besides national differences or study design, long-term care facilities are variously operated and heterogenous in private medical sector, making it difficult to generalize. In patients with long-term care facility admission history, additional attention to scabies might help early diagnosis.
According to the 2019 national long-term care survey of Korea, the average age of long-term care recipients is 80.1, and those who can move independently account for 21.3% of the total. The most common period of admission to a long-term care facility was less than 1–2 years, accounting for 26.6%, indicating that at least several months after admission.
12 It is estimated that the risk of transmission increases from the point that high age of long-term care facility patients and non-specific dermatitis is common in elderly patients, and the patient's inability to complain about subjective symptoms makes it difficult to detect scabies infection clinically, and the structural characteristics of long term care facilities, as multiple patients and medical staff cross-contact and the patient is hospitalized for a long period of time.
Dermal screening for all the residents of long-term care facilities is not a solution to prevent scabies introduction to acute care hospital. Because of incubation period, scabies patients do not necessarily develop symptoms at the time of admission. Sensitivity of skin scrapes is limited because the number of adult mites on a human with ordinary scabies is low and fewer than 15.
3 The sensitivity of microscopic diagnosis might be even lower when the exam was not done from a clearly suspected lesion. Based on our results, scabies patients were very few among many patients who come from long-term care facilities to acute care hospitals. It is difficult to diagnosis all the cases with a low prevalence by a low sensitive test. Therefore, it is necessary to educate health-care workers about atypical presentation and pay attention to skin of patients practically. Particularly in patients with long-term care facility admission history, thorough skin examination and including scabies in the differential diagnosis of all the patients with pruritic skin lesion, papules, vesicles, pustules, and pruritus would be helpful for early detection of scabies.
13
Most of the scabies patients in this study were diagnosed within 10 days after admission, but some patients were diagnosed after a considerable time (
Supplementary Fig. 1C). There is a risk of nosocomial transmission when scabies is not diagnosed early after admission to a medical institute. In this study, we conducted an epidemiological investigation of medical staff and caregivers exposed to the index patient and treated them with prophylactic permethrin cream to prevent possible transmission. Although the absolute number of cases was not many every year, scabies was continuously diagnosed in the hospital, and in some patients, it is diagnosed after 2 months of admission or more. In such a case, it is related to infection control in the institution and many exposure events are happening. In order to improve this aspect, it is necessary to continuously observe skin symptoms even in patients who have been hospitalized and to actively suspect scabies in patients with skin symptoms. Moreover, if the skin symptoms do not improve with symptomatic treatment, repeated tests may be necessary even if it is confirmed as negative.
7
There are limited reports about regional data of scabies prevalence in long-term care facilities. Japanese research reported 41% of psychiatric and long-term care hospitals experienced scabies in 2004.
11 Another Canadian report reported 25% of 130 chronic healthcare institutions experienced scabies cases during a one-year period.
14 The following study about regional data on the prevalence of scabies in a long-term care facility would help assessing region-specific risk of scabies in the medical environment.
Interestingly, patients with scabies were medically severe at the admission date and more were admitted via the emergency department. Patients with severe status need intensive acute treatment and it is hard for scabies to get attention in this situation. Overcrowding and time constraints were reported as risk factors of missed diagnosis of scabies during emergency department stay in another study.
15 It might be burdensome to check many risk factors in a situation of acute medical care for medically severe patients. We confirmed the other variables were not independent of each other. In that aspect, this study is meaningful for identifying a single independent risk factor that can be used to suspect scabies in a hospital environment.
This study has limitations from the retrospective nature. In particular, skin lesion and itching symptom was reported in the scabies group more than 70%, it was detected while scabies infection was suspicious and diagnosed, not at the time of admission. Only limited information was extracted from the admission note, and it might reflect that medical staff cannot afford to take a meticulous examination of skin lesions during the admission process, which gives reason for elucidating representative risk factors of scabies infection in these patients.
In conclusion, scabies infection in an acute medical environment is associated with patient's previous long-term care facility admission.
Ethics statement
This study was ethically approved by the Institute Review Board of Soonchunhyang University Seoul Hospital (No. 2018-04-031). Informed consent was waived by the board considering the nature of this retrospective study.