1. Leopold JA. Vascular calcification: an age-old problem of old age. Circulation. 2013; 127:2380–2382. PMID:
23690467.
2. Demer LL, Tintut Y. Vascular calcification: pathobiology of a multifaceted disease. Circulation. 2008; 117:2938–2948. PMID:
18519861.
3. Braun J, Oldendorf M, Moshage W, Heidler R, Zeitler E, Luft FC. Electron beam computed tomography in the evaluation of cardiac calcification in chronic dialysis patients. Am J Kidney Dis. 1996; 27:394–401. PMID:
8604709.
4. Goodman WG, Goldin J, Kuizon BD, et al. Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000; 342:1478–1483. PMID:
10816185.

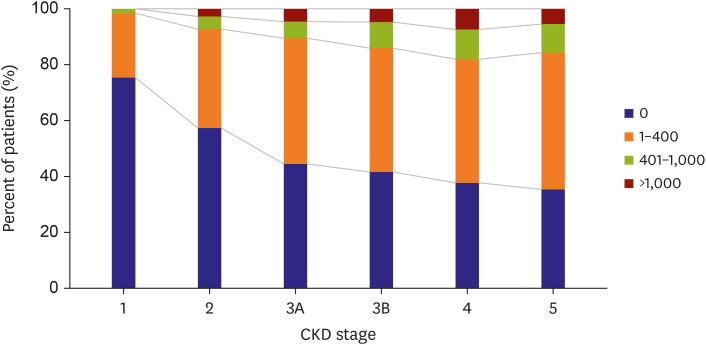
5. Fang Y, Ginsberg C, Sugatani T, Monier-Faugere MC, Malluche H, Hruska KA. Early chronic kidney disease-mineral bone disorder stimulates vascular calcification. Kidney Int. 2014; 85:142–150. PMID:
23884339.

6. Mizobuchi M, Towler D, Slatopolsky E. Vascular calcification: the killer of patients with chronic kidney disease. J Am Soc Nephrol. 2009; 20:1453–1464. PMID:
19478096.

7. Rennenberg RJ, Kessels AG, Schurgers LJ, van Engelshoven JM, de Leeuw PW, Kroon AA. Vascular calcifications as a marker of increased cardiovascular risk: a meta-analysis. Vasc Health Risk Manag. 2009; 5:185–197. PMID:
19436645.

8. Fang Y, Ginsberg C, Seifert M, et al. CKD-induced wingless/integration1 inhibitors and phosphorus cause the CKD-mineral and bone disorder. J Am Soc Nephrol. 2014; 25:1760–1773. PMID:
24578135.

9. Zhan JK, Wang YJ, Wang Y, et al. The protective effect of GLP-1 analogue in arterial calcification through attenuating osteoblastic differentiation of human VSMCs. Int J Cardiol. 2015; 189:188–193. PMID:
25897902.

10. Hénaut L, Chillon JM, Kamel S, Massy ZA. Updates on the mechanisms and the care of cardiovascular calcification in chronic kidney disease. Semin Nephrol. 2018; 38:233–250. PMID:
29753400.

11. Metz RP, Patterson JL, Wilson E. Vascular smooth muscle cells: isolation, culture, and characterization. Methods Mol Biol. 2012; 843:169–176. PMID:
22222531.

12. Durham AL, Speer MY, Scatena M, Giachelli CM, Shanahan CM. Role of smooth muscle cells in vascular calcification: implications in atherosclerosis and arterial stiffness. Cardiovasc Res. 2018; 114:590–600. PMID:
29514202.

13. Monroy MA, Fang J, Li S, et al. Chronic kidney disease alters vascular smooth muscle cell phenotype. Front Biosci (Landmark Ed). 2015; 20:784–795. PMID:
25553479.

14. Madsen M, Aarup A, Albinsson S, et al. Uremia modulates the phenotype of aortic smooth muscle cells. Atherosclerosis. 2017; 257:64–70. PMID:
28107707.

15. Patidar A, Singh DK, Thakur S, Farrington K, Baydoun AR. Uremic serum-induced calcification of human aortic smooth muscle cells is a regulated process involving Klotho and RUNX2. Biosci Rep. 2019; 39:BSR20190599. PMID:
31519772.

16. Cazaña-Pérez V, Cidad P, Donate-Correa J, et al. Phenotypic modulation of cultured primary human aortic vascular smooth muscle cells by uremic serum. Front Physiol. 2018; 9:89. PMID:
29483881.

17. Patidar A, Singh DK, Winocour P, Farrington K, Baydoun AR. Human uraemic serum displays calcific potential in vitro that increases with advancing chronic kidney disease. Clin Sci (Lond). 2013; 125:237–245. PMID:
23464884.

18. Moradi H, Sica DA, Kalantar-Zadeh K. Cardiovascular burden associated with uremic toxins in patients with chronic kidney disease. Am J Nephrol. 2013; 38:136–148. PMID:
23941724.

19. Cottone S, Lorito MC, Riccobene R, et al. Oxidative stress, inflammation and cardiovascular disease in chronic renal failure. J Nephrol. 2008; 21:175–179. PMID:
18446711.
20. Kelly D, Rothwell PM. Disentangling the multiple links between renal dysfunction and cerebrovascular disease. J Neurol Neurosurg Psychiatry. 2020; 91:88–97. PMID:
31511306.

21. Johnson-Davis KL, Fernelius C, Eliason NB, Wilson A, Beddhu S, Roberts WL. Blood enzymes and oxidative stress in chronic kidney disease: a cross sectional study. Ann Clin Lab Sci. 2011; 41:331–339. PMID:
22166502.
22. Yamada S, Taniguchi M, Tokumoto M, et al. The antioxidant tempol ameliorates arterial medial calcification in uremic rats: important role of oxidative stress in the pathogenesis of vascular calcification in chronic kidney disease. J Bone Miner Res. 2012; 27:474–485. PMID:
21987400.

23. Huang M, Zheng L, Xu H, et al. Oxidative stress contributes to vascular calcification in patients with chronic kidney disease. J Mol Cell Cardiol. 2020; 138:256–268. PMID:
31866376.

24. Podkowińska A, Formanowicz D. Chronic kidney disease as oxidative stress- and inflammatory-mediated cardiovascular disease. Antioxidants. 2020; 9:752.

25. Bover J, Evenepoel P, Ureña-Torres P, et al. Pro: cardiovascular calcifications are clinically relevant. Nephrol Dial Transplant. 2015; 30:345–351. PMID:
25712934.

26. Kiu Weber CI, Duchateau-Nguyen G, Solier C, et al. Cardiovascular risk markers associated with arterial calcification in patients with chronic kidney disease Stages 3 and 4. Clin Kidney J. 2014; 7:167–173. PMID:
24683472.

27. Benz K, Hilgers KF, Daniel C, Amann K. Vascular calcification in chronic kidney disease: the role of inflammation. Int J Nephrol. 2018; 2018:4310379. PMID:
30186632.

28. Choi SR, Lee YK, Cho AJ, et al. Malnutrition, inflammation, progression of vascular calcification and survival: Inter-relationships in hemodialysis patients. PLoS One. 2019; 14:e0216415. PMID:
31048884.

29. Hénaut L, Massy ZA. New insights into the key role of interleukin 6 in vascular calcification of chronic kidney disease. Nephrol Dial Transplant. 2018; 33:543–548. PMID:
29420799.

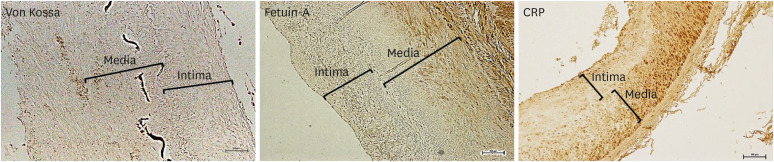
30. Benz K, Varga I, Neureiter D, et al. Vascular inflammation and media calcification are already present in early stages of chronic kidney disease. Cardiovasc Pathol. 2017; 27:57–67. PMID:
28171827.

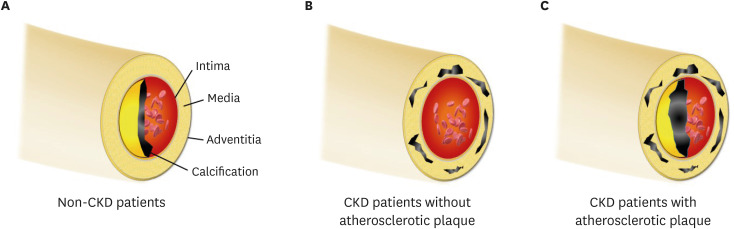
31. Gross ML, Meyer HP, Ziebart H, et al. Calcification of coronary intima and media: immunohistochemistry, backscatter imaging, and x-ray analysis in renal and nonrenal patients. Clin J Am Soc Nephrol. 2007; 2:121–134. PMID:
17699396.

32. Masuda M, Miyazaki-Anzai S, Levi M, Ting TC, Miyazaki M. PERK-eIF2α-ATF4-CHOP signaling contributes to TNFα-induced vascular calcification. J Am Heart Assoc. 2013; 2:e000238. PMID:
24008080.

33. Moe SM, Drüeke T, Lameire N, Eknoyan G. Chronic kidney disease-mineral-bone disorder: a new paradigm. Adv Chronic Kidney Dis. 2007; 14:3–12. PMID:
17200038.

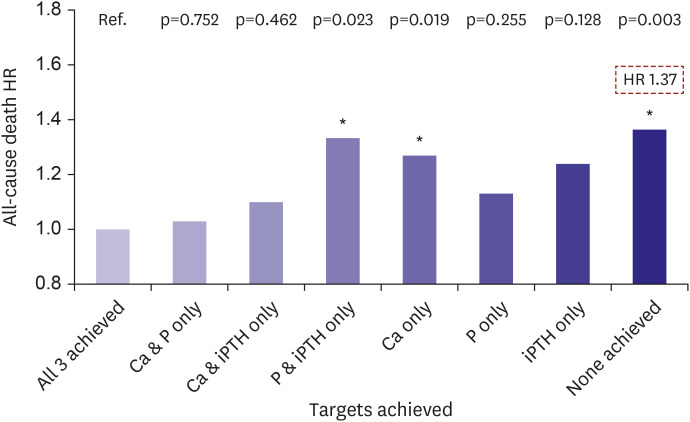
34. Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004; 15:2208–2218. PMID:
15284307.

35. Yang H, Curinga G, Giachelli CM. Elevated extracellular calcium levels induce smooth muscle cell matrix mineralization in vitro. Kidney Int. 2004; 66:2293–2299. PMID:
15569318.
36. Giachelli CM. The emerging role of phosphate in vascular calcification. Kidney Int. 2009; 75:890–897. PMID:
19145240.

37. Jono S, McKee MD, Murry CE, et al. Phosphate regulation of vascular smooth muscle cell calcification. Circ Res. 2000; 87:E10–E17. PMID:
11009570.

38. Jono S, Shioi A, Ikari Y, Nishizawa Y. Vascular calcification in chronic kidney disease. J Bone Miner Metab. 2006; 24:176–181. PMID:
16502129.

39. Hwang HS, Lim SW, Sun IO, et al. Clinical significance of preexisting microcalcification in the iliac artery in renal transplant recipients. Transplantation. 2015; 99:811–817. PMID:
25211516.

40. Quarles LD. Role of FGF23 in vitamin D and phosphate metabolism: implications in chronic kidney disease. Exp Cell Res. 2012; 318:1040–1048. PMID:
22421513.

41. Scialla JJ, Xie H, Rahman M, et al. Fibroblast growth factor-23 and cardiovascular events in CKD. J Am Soc Nephrol. 2014; 25:349–360. PMID:
24158986.

42. Hu MC, Shi M, Zhang J, et al. Klotho deficiency causes vascular calcification in chronic kidney disease. J Am Soc Nephrol. 2011; 22:124–136. PMID:
21115613.

43. Krishnasamy R, Tan SJ, Hawley CM, et al. Progression of arterial stiffness is associated with changes in bone mineral markers in advanced CKD. BMC Nephrol. 2017; 18:281. PMID:
28870151.

44. Baralić M, Brković V, Stojanov V, et al. Dual roles of the mineral metabolism disorders biomarkers in prevalent hemodilysis patients: in renal bone disease and in vascular calcification. J Med Biochem. 2019; 38:134–144. PMID:
30867641.

45. Desjardins L, Liabeuf S, Renard C, et al. FGF23 is independently associated with vascular calcification but not bone mineral density in patients at various CKD stages. Osteoporos Int. 2012; 23:2017–2025. PMID:
22109743.

46. Morena M, Jaussent I, Halkovich A, et al. Bone biomarkers help grading severity of coronary calcifications in non dialysis chronic kidney disease patients. PLoS One. 2012; 7:e36175. PMID:
22567137.

47. Zhu D, Mackenzie NC, Millan JL, Farquharson C, MacRae VE. A protective role for FGF-23 in local defence against disrupted arterial wall integrity? Mol Cell Endocrinol. 2013; 372:1–11. PMID:
23523568.

48. Boyce BF, Xing L. Functions of RANKL/RANK/OPG in bone modeling and remodeling. Arch Biochem Biophys. 2008; 473:139–146. PMID:
18395508.

49. Bucay N, Sarosi I, Dunstan CR, et al. Osteoprotegerin-deficient mice develop early onset osteoporosis and arterial calcification. Genes Dev. 1998; 12:1260–1268. PMID:
9573043.
50. Kiechl S, Werner P, Knoflach M, Furtner M, Willeit J, Schett G. The osteoprotegerin/RANK/RANKL system: a bone key to vascular disease. Expert Rev Cardiovasc Ther. 2006; 4:801–811. PMID:
17173497.

51. Kaden JJ, Bickelhaupt S, Grobholz R, et al. Receptor activator of nuclear factor kappaB ligand and osteoprotegerin regulate aortic valve calcification. J Mol Cell Cardiol. 2004; 36:57–66. PMID:
14734048.
52. Van Campenhout A, Golledge J. Osteoprotegerin, vascular calcification and atherosclerosis. Atherosclerosis. 2009; 204:321–329. PMID:
19007931.

53. Morena M, Jaussent I, Dupuy AM, et al. Osteoprotegerin and sclerostin in chronic kidney disease prior to dialysis: potential partners in vascular calcifications. Nephrol Dial Transplant. 2015; 30:1345–1356. PMID:
25854266.

54. Mesquita M, Demulder A, Damry N, et al. Plasma osteoprotegerin is an independent risk factor for mortality and an early biomarker of coronary vascular calcification in chronic kidney disease. Clin Chem Lab Med. 2009; 47:339–346. PMID:
19676147.

55. Mikami S, Hamano T, Fujii N, et al. Serum osteoprotegerin as a screening tool for coronary artery calcification score in diabetic pre-dialysis patients. Hypertens Res. 2008; 31:1163–1170. PMID:
18716364.

56. Heiss A, DuChesne A, Denecke B, et al. Structural basis of calcification inhibition by alpha 2-HS glycoprotein/fetuin-A. Formation of colloidal calciprotein particles. J Biol Chem. 2003; 278:13333–13341. PMID:
12556469.
57. Cai MM, Smith ER, Holt SG. The role of fetuin-A in mineral trafficking and deposition. Bonekey Rep. 2015; 4:672. PMID:
25987986.

58. Schäfer C, Heiss A, Schwarz A, et al. The serum protein alpha 2-Heremans-Schmid glycoprotein/fetuin-A is a systemically acting inhibitor of ectopic calcification. J Clin Invest. 2003; 112:357–366. PMID:
12897203.
59. Ketteler M, Bongartz P, Westenfeld R, et al. Association of low fetuin-A (AHSG) concentrations in serum with cardiovascular mortality in patients on dialysis: a cross-sectional study. Lancet. 2003; 361:827–833. PMID:
12642050.

60. Reynolds JL, Skepper JN, McNair R, et al. Multifunctional roles for serum protein fetuin-a in inhibition of human vascular smooth muscle cell calcification. J Am Soc Nephrol. 2005; 16:2920–2930. PMID:
16093453.

61. Matsui I, Hamano T, Mikami S, et al. Fully phosphorylated fetuin-A forms a mineral complex in the serum of rats with adenine-induced renal failure. Kidney Int. 2009; 75:915–928. PMID:
19190677.

62. Hamano T, Matsui I, Mikami S, et al. Fetuin-mineral complex reflects extraosseous calcification stress in CKD. J Am Soc Nephrol. 2010; 21:1998–2007. PMID:
20947626.

63. Disthabanchong S, Boongird S. Role of different imaging modalities of vascular calcification in predicting outcomes in chronic kidney disease. World J Nephrol. 2017; 6:100–110. PMID:
28540199.

64. Kauppila LI, Polak JF, Cupples LA, Hannan MT, Kiel DP, Wilson PW. New indices to classify location, severity and progression of calcific lesions in the abdominal aorta: a 25-year follow-up study. Atherosclerosis. 1997; 132:245–250. PMID:
9242971.

65. Raggi P, Bellasi A, Ferramosca E, Islam T, Muntner P, Block GA. Association of pulse wave velocity with vascular and valvular calcification in hemodialysis patients. Kidney Int. 2007; 71:802–807. PMID:
17311068.

66. Bellasi A, Ferramosca E, Muntner P, et al. Correlation of simple imaging tests and coronary artery calcium measured by computed tomography in hemodialysis patients. Kidney Int. 2006; 70:1623–1628. PMID:
16955104.

67. Okuno S, Ishimura E, Kitatani K, et al. Presence of abdominal aortic calcification is significantly associated with all-cause and cardiovascular mortality in maintenance hemodialysis patients. Am J Kidney Dis. 2007; 49:417–425. PMID:
17336703.

68. Verbeke F, Van Biesen W, Honkanen E, et al. CORD Study Investigators. Prognostic value of aortic stiffness and calcification for cardiovascular events and mortality in dialysis patients: outcome of the calcification outcome in renal disease (CORD) study. Clin J Am Soc Nephrol. 2011; 6:153–159. PMID:
20829424.

69. Bellasi A, Raggi P. Techniques and technologies to assess vascular calcification. Semin Dial. 2007; 20:129–133. PMID:
17374086.
70. Guérin AP, London GM, Marchais SJ, Metivier F. Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol Dial Transplant. 2000; 15:1014–1021. PMID:
10862640.

71. Oh DJ. Continuous ambulatory peritoneal dialysis patients show high prevalence of carotid artery calcification which is associated with a higher left ventricular mass index. J Korean Med Sci. 2005; 20:848–852. PMID:
16224161.

72. Sumida Y, Nakayama M, Nagata M, et al. Carotid artery calcification and atherosclerosis at the initiation of hemodialysis in patients with end-stage renal disease. Clin Nephrol. 2010; 73:360–369. PMID:
20420796.

73. Nakayama M, Ura Y, Nagata M, et al. Carotid artery calcification at the initiation of hemodialysis is a risk factor for cardiovascular events in patients with end-stage renal disease: a cohort study. BMC Nephrol. 2011; 12:56. PMID:
21999942.

74. Disthabanchong S. Vascular calcification in chronic kidney disease: Pathogenesis and clinical implication. World J Nephrol. 2012; 1:43–53. PMID:
24175241.

75. Lima A, Carrilho P, Germano A. Clinical and ultrasound evaluation for hemodialysis access creation. Nefrologia (Engl Ed). 2021.

76. Shenoy S, Darcy M. Ultrasound as a tool for preoperative planning, monitoring, and interventions in dialysis arteriovenous access. AJR Am J Roentgenol. 2013; 201:W539–W543. PMID:
24059390.

77. Dube P, DeRiso A, Patel M, et al. Vascular calcification in chronic kidney disease: diversity in the vessel wall. Biomedicines. 2021; 9:404. PMID:
33917965.

78. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990; 15:827–832. PMID:
2407762.

79. Karohl C, D'Marco Gascón L, Raggi P. Noninvasive imaging for assessment of calcification in chronic kidney disease. Nat Rev Nephrol. 2011; 7:567–577. PMID:
21862991.

80. De Mauri A, Brambilla M, Chiarinotti D, Matheoud R, Carriero A, De Leo M. Estimated radiation exposure from medical imaging in hemodialysis patients. J Am Soc Nephrol. 2011; 22:571–578. PMID:
21355057.

81. Marinelli A, Pistolesi V, Pasquale L, et al. Diagnosis of arterial media calcification in chronic kidney disease. Cardiorenal Med. 2013; 3:89–95. PMID:
23922548.

82. Mehrotra R, Budoff M, Hokanson JE, Ipp E, Takasu J, Adler S. Progression of coronary artery calcification in diabetics with and without chronic kidney disease. Kidney Int. 2005; 68:1258–1266. PMID:
16105059.

83. Poli FE, Gulsin GS, McCann GP, Burton JO, Graham-Brown MP. The assessment of coronary artery disease in patients with end-stage renal disease. Clin Kidney J. 2019; 12:721–734. PMID:
31583096.

84. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl (2011). 2017; 7:1–59. PMID:
30675420.
85. Reiss AB, Miyawaki N, Moon J, et al. CKD, arterial calcification, atherosclerosis and bone health: inter-relationships and controversies. Atherosclerosis. 2018; 278:49–59. PMID:
30253289.

86. Zoccali C. Traditional and emerging cardiovascular and renal risk factors: an epidemiologic perspective. Kidney Int. 2006; 70:26–33. PMID:
16723985.

87. Kim Y, Cho JS, Cho WK, et al. Retinopathy and left ventricular hypertrophy in patients with chronic kidney disease: Interrelationship and impact on clinical outcomes. Int J Cardiol. 2017; 249:372–376. PMID:
29121742.

88. Hwang HS, Choi YA, Kim SY, et al. Diabetes retinopathy is a poor predictor for renal and cardiovascular outcomes in comparison with hypertensive retinopathy in patients with chronic kidney disease. Diabetes Res Clin Pract. 2015; 109:312–318. PMID:
26008724.

89. Drüeke TB, Massy ZA. Atherosclerosis in CKD: differences from the general population. Nat Rev Nephrol. 2010; 6:723–735. PMID:
20978469.

90. Nakano T, Ninomiya T, Sumiyoshi S, et al. Association of kidney function with coronary atherosclerosis and calcification in autopsy samples from Japanese elders: the Hisayama study. Am J Kidney Dis. 2010; 55:21–30. PMID:
19765871.

91. Nakamura S, Ishibashi-Ueda H, Niizuma S, Yoshihara F, Horio T, Kawano Y. Coronary calcification in patients with chronic kidney disease and coronary artery disease. Clin J Am Soc Nephrol. 2009; 4:1892–1900. PMID:
19833908.

92. Oh KH, Kang M, Kang E, et al. The KNOW-CKD Study: What we have learned about chronic kidney diseases. Kidney Res Clin Pract. 2020; 39:121–135. PMID:
32550711.

93. Goodman WG, London G, Amann K, et al. Vascular calcification in chronic kidney disease. Am J Kidney Dis. 2004; 43:572–579. PMID:
14981617.

94. Moe SM, O'Neill KD, Duan D, et al. Medial artery calcification in ESRD patients is associated with deposition of bone matrix proteins. Kidney Int. 2002; 61:638–647. PMID:
11849407.

95. Milliner DS, Zinsmeister AR, Lieberman E, Landing B. Soft tissue calcification in pediatric patients with end-stage renal disease. Kidney Int. 1990; 38:931–936. PMID:
2266678.

96. Hwang HS, Cho JS, Hong YA, et al. Vascular calcification and left ventricular hypertrophy in hemodialysis patients: interrelationship and clinical impacts. Int J Med Sci. 2018; 15:557–563. PMID:
29725245.

97. London GM, Marchais SJ, Guérin AP, Métivier F. Arteriosclerosis, vascular calcifications and cardiovascular disease in uremia. Curr Opin Nephrol Hypertens. 2005; 14:525–531. PMID:
16205470.

98. Lee HY, Lim S, Park S. Role of inflammation in arterial calcification. Korean Circ J. 2021; 51:114–125. PMID:
33525066.

99. Mori D, Matsui I, Shimomura A, et al. Protein carbamylation exacerbates vascular calcification. Kidney Int. 2018; 94:72–90. PMID:
29716796.

100. Voelkl J, Cejka D, Alesutan I. An overview of the mechanisms in vascular calcification during chronic kidney disease. Curr Opin Nephrol Hypertens. 2019; 28:289–296. PMID:
30985336.

101. Merjanian R, Budoff M, Adler S, Berman N, Mehrotra R. Coronary artery, aortic wall, and valvular calcification in nondialyzed individuals with type 2 diabetes and renal disease. Kidney Int. 2003; 64:263–271. PMID:
12787418.

102. Kramer H, Toto R, Peshock R, Cooper R, Victor R. Association between chronic kidney disease and coronary artery calcification: the Dallas Heart Study. J Am Soc Nephrol. 2005; 16:507–513. PMID:
15601745.

103. Lee W, Yoon YE, Kwon O, et al. Evaluation of coronary artery calcium progression in asymptomatic individuals with an initial score of zero. Korean Circ J. 2019; 49:448–457. PMID:
30808082.

104. Bover J, Aguilar A, Arana C, et al. Clinical approach to vascular calcification in patients with non-dialysis dependent chronic kidney disease: mineral-bone disorder-related aspects. Front Med (Lausanne). 2021; 8:642718. PMID:
34095165.

105. Budoff MJ, Rader DJ, Reilly MP, et al. CRIC Study Investigators. Relationship of estimated GFR and coronary artery calcification in the CRIC (Chronic Renal Insufficiency Cohort) Study. Am J Kidney Dis. 2011; 58:519–526. PMID:
21783289.

106. Górriz JL, Molina P, Cerverón MJ, et al. Vascular calcification in patients with nondialysis CKD over 3 years. Clin J Am Soc Nephrol. 2015; 10:654–666. PMID:
25770175.

107. Kestenbaum BR, Adeney KL, de Boer IH, Ix JH, Shlipak MG, Siscovick DS. Incidence and progression of coronary calcification in chronic kidney disease: the Multi-Ethnic Study of Atherosclerosis. Kidney Int. 2009; 76:991–998. PMID:
19692998.

108. Kronmal RA, McClelland RL, Detrano R, et al. Risk factors for the progression of coronary artery calcification in asymptomatic subjects: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2007; 115:2722–2730. PMID:
17502571.
109. Reynolds JL, Joannides AJ, Skepper JN, et al. Human vascular smooth muscle cells undergo vesicle-mediated calcification in response to changes in extracellular calcium and phosphate concentrations: a potential mechanism for accelerated vascular calcification in ESRD. J Am Soc Nephrol. 2004; 15:2857–2867. PMID:
15504939.

110. Daniel WT, Weber C, Bailey JA, Raggi P, Sharma J. Prospective analysis of coronary calcium in patients on dialysis undergoing a near-total parathyroidectomy. Surgery. 2013; 154:1315–1321. PMID:
24238050.

111. Savage T, Clarke AL, Giles M, Tomson CR, Raine AE. Calcified plaque is common in the carotid and femoral arteries of dialysis patients without clinical vascular disease. Nephrol Dial Transplant. 1998; 13:2004–2012. PMID:
9719155.

112. Schlieper G, Aretz A, Verberckmoes SC, et al. Ultrastructural analysis of vascular calcifications in uremia. J Am Soc Nephrol. 2010; 21:689–696. PMID:
20203159.

113. Kim SY, Hong YA, Yoon HE, et al. Vascular calcification and intradialytic hypotension in hemodialysis patients: Clinical relevance and impact on morbidity and mortality. Int J Cardiol. 2016; 217:156–160. PMID:
27183451.

114. Alappan HR, Vasanth P, Manzoor S, O'Neill WC. Vascular calcification slows but does not regress after kidney transplantation. Kidney Int Rep. 2020; 5:2212–2217. PMID:
33305114.

115. Schankel K, Robinson J, Bloom RD, et al. Determinants of coronary artery calcification progression in renal transplant recipients. Am J Transplant. 2007; 7:2158–2164. PMID:
17640315.

116. Bargnoux AS, Dupuy AM, Garrigue V, et al. Evolution of coronary artery calcifications following kidney transplantation: relationship with osteoprotegerin levels. Am J Transplant. 2009; 9:2571–2579. PMID:
19775319.

117. Mazzaferro S, Pasquali M, Taggi F, et al. Progression of coronary artery calcification in renal transplantation and the role of secondary hyperparathyroidism and inflammation. Clin J Am Soc Nephrol. 2009; 4:685–690. PMID:
19211668.

118. Messa P, Sindici C, Cannella G, et al. Persistent secondary hyperparathyroidism after renal transplantation. Kidney Int. 1998; 54:1704–1713. PMID:
9844148.

119. Lou I, Foley D, Odorico SK, et al. How well does renal transplantation cure hyperparathyroidism? Ann Surg. 2015; 262:653–659. PMID:
26366545.

120. Mathur A, Sutton W, Ahn JB, et al. Association between treatment of secondary hyperparathyroidism and posttransplant outcomes. Transplantation. 2021.

121. Hwang HS, Kim JS, Kim YG, et al. Circulating PCSK9 level and risk of cardiovascular events and death in hemodialysis patients. J Clin Med. 2020; 9:9.

122. Hwang HS, Kim JS, Kim YG, et al. Circulating neprilysin level predicts the risk of cardiovascular events in hemodialysis patients. Front Cardiovasc Med. 2021; 8:684297. PMID:
34212014.

123. Cho IJ, Chang HJ, Lee SE, Shim CY, Hong GR, Chung N. Prognostic application of thoracic aortic calcium scoring for adverse clinical outcome risk in elderly patients with left ventricular hypertrophy. Korean Circ J. 2017; 47:918–928. PMID:
29035431.

124. Chen J, Budoff MJ, Reilly MP, et al. Coronary artery calcification and risk of cardiovascular disease and death among patients with chronic kidney disease. JAMA Cardiol. 2017; 2:635–643. PMID:
28329057.

125. Nelson AJ, Raggi P, Wolf M, Gold AM, Chertow GM, Roe MT. Targeting vascular calcification in chronic kidney disease. JACC Basic Transl Sci. 2020; 5:398–412. PMID:
32368697.

126. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl. 2009; S1–S130.
127. Dilsizian V, Gewirtz H, Marwick TH, et al. Cardiac imaging for coronary heart disease risk stratification in chronic kidney disease. JACC Cardiovasc Imaging. 2021; 14:669–682. PMID:
32828780.
128. Herzog CA, Natwick T, Li S, Charytan DM. Comparative utilization and temporal trends in cardiac stress testing in U.S. Medicare beneficiaries with and without chronic kidney disease. JACC Cardiovasc Imaging. 2019; 12:1420–1426. PMID:
29909107.
129. Mathew RO, Bangalore S, Lavelle MP, et al. Diagnosis and management of atherosclerotic cardiovascular disease in chronic kidney disease: a review. Kidney Int. 2017; 91:797–807. PMID:
28040264.
130. Schwarz U, Buzello M, Ritz E, et al. Morphology of coronary atherosclerotic lesions in patients with end-stage renal failure. Nephrol Dial Transplant. 2000; 15:218–223. PMID:
10648668.

131. Sharples EJ, Pereira D, Summers S, et al. Coronary artery calcification measured with electron-beam computerized tomography correlates poorly with coronary artery angiography in dialysis patients. Am J Kidney Dis. 2004; 43:313–319. PMID:
14750097.

132. Haydar AA, Hujairi NM, Covic AA, Pereira D, Rubens M, Goldsmith DJ. Coronary artery calcification is related to coronary atherosclerosis in chronic renal disease patients: a study comparing EBCT-generated coronary artery calcium scores and coronary angiography. Nephrol Dial Transplant. 2004; 19:2307–2312. PMID:
15213315.

133. Yiu KH, de Graaf FR, van Velzen JE, et al. Different value of coronary calcium score to predict obstructive coronary artery disease in patients with and without moderate chronic kidney disease. Neth Heart J. 2013; 21:347–353. PMID:
23579986.

134. Hwang HS, Kim SY, Hong YA, et al. Clinical impact of coexisting retinopathy and vascular calcification on chronic kidney disease progression and cardiovascular events. Nutr Metab Cardiovasc Dis. 2016; 26:590–596. PMID:
27089976.

135. Hwang HS, Park MW, Yoon HE, et al. Clinical significance of chronic kidney disease and atrial fibrillation on morbidity and mortality in patients with acute myocardial infarction. Am J Nephrol. 2014; 40:345–352. PMID:
25358406.

136. Naves M, Rodríguez-García M, Díaz-López JB, Gómez-Alonso C, Cannata-Andía JB. Progression of vascular calcifications is associated with greater bone loss and increased bone fractures. Osteoporos Int. 2008; 19:1161–1166. PMID:
18180973.

137. London GM, Marty C, Marchais SJ, Guerin AP, Metivier F, de Vernejoul MC. Arterial calcifications and bone histomorphometry in end-stage renal disease. J Am Soc Nephrol. 2004; 15:1943–1951. PMID:
15213285.

138. Lee SM, Kim SE, Lee JY, Jeong HJ, Son YK, An WS. Serum myostatin levels are associated with abdominal aortic calcification in dialysis patients. Kidney Res Clin Pract. 2019; 38:481–489. PMID:
31537054.

139. Osako MK, Nakagami H, Koibuchi N, et al. Estrogen inhibits vascular calcification via vascular RANKL system: common mechanism of osteoporosis and vascular calcification. Circ Res. 2010; 107:466–475. PMID:
20595654.
140. Viegas C, Araújo N, Marreiros C, Simes D. The interplay between mineral metabolism, vascular calcification and inflammation in Chronic Kidney Disease (CKD): challenging old concepts with new facts. Aging (Albany NY). 2019; 11:4274–4299. PMID:
31241466.

141. Nam YJ, Hwang SY, Kim DW, Kim D, Shin SJ, Yoon HE. Sex-specific relationship between vascular calcification and incident fracture in patients with end-stage renal disease. Kidney Res Clin Pract. 2020; 39:344–355. PMID:
32522894.

142. An WS. Sex hormones impact vascular calcification and fracture in dialysis patients. Kidney Res Clin Pract. 2020; 39:236–238. PMID:
32958722.

143. Jensky NE, Criqui MH, Wright CM, Wassel CL, Alcaraz JE, Allison MA. The association between abdominal body composition and vascular calcification. Obesity (Silver Spring). 2011; 19:2418–2424. PMID:
21475146.

144. Ko BJ, Chang Y, Jung HS, et al. Relationship between low relative muscle mass and coronary artery calcification in healthy adults. Arterioscler Thromb Vasc Biol. 2016; 36:1016–1021. PMID:
27034471.

145. Lee MJ, Park JT, Park KS, et al. Normal body mass index with central obesity has increased risk of coronary artery calcification in Korean patients with chronic kidney disease. Kidney Int. 2016; 90:1368–1376. PMID:
27884313.

146. Paoli S, Mitsnefes MM. Coronary artery calcification and cardiovascular disease in children with chronic kidney disease. Curr Opin Pediatr. 2014; 26:193–197. PMID:
24632542.

147. Cordeiro AC, Qureshi AR, Lindholm B, et al. Visceral fat and coronary artery calcification in patients with chronic kidney disease. Nephrol Dial Transplant. 2013; 28(Suppl 4):iv152–iv159. PMID:
23832273.

148. Moreno-Gonzalez R, Corbella X, Mattace-Raso F, et al. Prevalence of sarcopenia in community-dwelling older adults using the updated EWGSOP2 definition according to kidney function and albuminuria: the Screening for CKD among Older People across Europe (SCOPE) study. BMC Geriatr. 2020; 20(Suppl 1):327. PMID:
33008317.

149. Kim SH, Choi G, Song Y, et al. Low muscle mass in patients receiving hemodialysis: correlations with vascular calcification and vascular access failure. J Clin Med. 2021; 10:10.

150. Pérez-Ricart A, Galicia-Basart M, Comas-Sugrañes D, Cruzado-Garrit JM, Segarra-Medrano A, Montoro-Ronsano JB. Long-term effectiveness of cinacalcet in non-dialysis patients with chronic kidney disease and secondary hyperparathyroidism. Kidney Res Clin Pract. 2019; 38:229–238. PMID:
31022778.

151. Park EJ, Jung SW, Kim DR, et al. Conversion from acetate dialysate to citrate dialysate in a central delivery system for maintenance hemodialysis patients. Kidney Res Clin Pract. 2019; 38:100–107. PMID:
30754934.

152. Shroff R, Egerton M, Bridel M, et al. A bimodal association of vitamin D levels and vascular disease in children on dialysis. J Am Soc Nephrol. 2008; 19:1239–1246. PMID:
18337484.

153. Mathew S, Lund RJ, Chaudhary LR, Geurs T, Hruska KA. Vitamin D receptor activators can protect against vascular calcification. J Am Soc Nephrol. 2008; 19:1509–1519. PMID:
18448587.

154. Ketteler M, Martin KJ, Wolf M, et al. Paricalcitol versus cinacalcet plus low-dose vitamin D therapy for the treatment of secondary hyperparathyroidism in patients receiving haemodialysis: results of the IMPACT SHPT study. Nephrol Dial Transplant. 2012; 27:3270–3278. PMID:
22387567.

155. Teng M, Wolf M, Lowrie E, Ofsthun N, Lazarus JM, Thadhani R. Survival of patients undergoing hemodialysis with paricalcitol or calcitriol therapy. N Engl J Med. 2003; 349:446–456. PMID:
12890843.

156. Anis KH, Pober D, Rosas SE. Vitamin D analogues and coronary calcification in CKD Stages 3 and 4: a randomized controlled trial of calcitriol versus paricalcitol. Kidney Med. 2020; 2:450–458. PMID:
32775985.

157. Raggi P, Chertow GM, Torres PU, et al. The ADVANCE study: a randomized study to evaluate the effects of cinacalcet plus low-dose vitamin D on vascular calcification in patients on hemodialysis. Nephrol Dial Transplant. 2011; 26:1327–1339. PMID:
21148030.

158. Moe SM, Abdalla S, Chertow GM, et al. Effects of cinacalcet on fracture events in patients receiving hemodialysis: the EVOLVE trial. J Am Soc Nephrol. 2015; 26:1466–1475. PMID:
25505257.

159. Chertow GM, Block GA, Correa-Rotter R, et al. Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med. 2012; 367:2482–2494. PMID:
23121374.

160. Komaba H, Wang M, Taniguchi M, et al. Initiation of sevelamer and mortality among hemodialysis patients treated with calcium-based phosphate binders. Clin J Am Soc Nephrol. 2017; 12:1489–1497. PMID:
28724618.

161. Kakuta T, Tanaka R, Hyodo T, et al. Effect of sevelamer and calcium-based phosphate binders on coronary artery calcification and accumulation of circulating advanced glycation end products in hemodialysis patients. Am J Kidney Dis. 2011; 57:422–431. PMID:
21239096.

162. Patel L, Bernard LM, Elder GJ. Sevelamer versus calcium-based binders for treatment of hyperphosphatemia in CKD: a meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol. 2016; 11:232–244. PMID:
26668024.

163. Block GA, Raggi P, Bellasi A, Kooienga L, Spiegel DM. Mortality effect of coronary calcification and phosphate binder choice in incident hemodialysis patients. Kidney Int. 2007; 71:438–441. PMID:
17200680.

164. Krueger T, Schlieper G, Schurgers L, et al. Vitamin K1 to slow vascular calcification in haemodialysis patients (VitaVasK trial): a rationale and study protocol. Nephrol Dial Transplant. 2014; 29:1633–1638. PMID:
24285427.

165. Caluwé R, Pyfferoen L, De Boeck K, De Vriese AS. The effects of vitamin K supplementation and vitamin K antagonists on progression of vascular calcification: ongoing randomized controlled trials. Clin Kidney J. 2016; 9:273–279. PMID:
26985380.

166. Caluwé R, Verbeke F, De Vriese AS. Evaluation of vitamin K status and rationale for vitamin K supplementation in dialysis patients. Nephrol Dial Transplant. 2020; 35:23–33. PMID:
30590803.

167. Chan KE, Lazarus JM, Thadhani R, Hakim RM. Warfarin use associates with increased risk for stroke in hemodialysis patients with atrial fibrillation. J Am Soc Nephrol. 2009; 20:2223–2233. PMID:
19713308.

168. Olesen JB, Lip GY, Kamper AL, et al. Stroke and bleeding in atrial fibrillation with chronic kidney disease. N Engl J Med. 2012; 367:625–635. PMID:
22894575.

169. Rattazzi M, Faggin E, Bertacco E, et al. Warfarin, but not rivaroxaban, promotes the calcification of the aortic valve in ApoE-/- mice. Cardiovasc Ther. 2018; 36:e12438. PMID:
29847020.

170. Hasific S, Øvrehus KA, Gerke O, et al. Extent of arterial calcification by conventional vitamin K antagonist treatment. PLoS One. 2020; 15:e0241450. PMID:
33119722.

171. Plank F, Beyer C, Friedrich G, et al. Influence of vitamin K antagonists and direct oral anticoagulation on coronary artery disease: a CTA analysis. Int J Cardiol. 2018; 260:11–15. PMID:
29530620.

172. Lee J, Nakanishi R, Li D, et al. Randomized trial of rivaroxaban versus warfarin in the evaluation of progression of coronary atherosclerosis. Am Heart J. 2018; 206:127–130. PMID:
30227941.

173. Win TT, Nakanishi R, Osawa K, et al. Apixaban versus warfarin in evaluation of progression of atherosclerotic and calcified plaques (prospective randomized trial). Am Heart J. 2019; 212:129–133. PMID:
31002997.

174. De Vriese AS, Caluwé R, Pyfferoen L, et al. Multicenter randomized controlled trial of vitamin K antagonist replacement by rivaroxaban with or without vitamin K2 in hemodialysis patients with atrial fibrillation: the Valkyrie study. J Am Soc Nephrol. 2020; 31:186–196. PMID:
31704740.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download