2. Bhagyalakshmi N, Thimmaraju R, Venkatachalam L, Murthy KN, Sreedhar RV. Nutraceutical applications of garlic and the intervention of biotechnology. Crit Rev Food Sci Nutr. 2005; 45:607–621. PMID:
16371330.

3. Rivlin RS. Historical perspective on the use of garlic. J Nutr. 2001; 131:951S–954S.

4. Ngo SN, Williams DB, Cobiac L, Head RJ. Does garlic reduce risk of colorectal cancer? A systematic review. J Nutr. 2007; 137:2264–2269. PMID:
17885009.

5. Wu X, Kassie F, Mersch-Sundermann V. Induction of apoptosis in tumor cells by naturally occurring sulfur-containing compounds. Mutat Res. 2005; 589:81–102. PMID:
15795163.

6. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424. PMID:
30207593.

7. Shang A, Cao SY, Xu XY, Gan RY, Tang GY, Corke H, Mavumengwana V, Li HB. Bioactive compounds and biological functions of garlic (allium sativum l.). Foods. 2019; 8:246.

8. Miraghajani M, Rafie N, Hajianfar H, Larijani B, Azadbakht L. Aged garlic and cancer: a systematic review. Int J Prev Med. 2018; 9:84. PMID:
30487964.

9. Karmakar S, Choudhury SR, Banik NL, Ray SK. Molecular mechanisms of anti-cancer action of garlic compounds in neuroblastoma. Anticancer Agents Med Chem. 2011; 11:398–407. PMID:
21521157.

10. Nouroz F, Mehboob M, Noreen S, Zaidi F, Mobin T. A review on anticancer activities of garlic (Allium sativum L.). Middle East J Sci Res. 2015; 23:1145–1151.
11. Zhang W, Ha M, Gong Y, Xu Y, Dong N, Yuan Y. Allicin induces apoptosis in gastric cancer cells through activation of both extrinsic and intrinsic pathways. Oncol Rep. 2010; 24:1585–1592. PMID:
21042755.

12. World Cancer Research Fund. American Institute for Cancer Research. Continuous Update Project Expert Report 2018. Diet, nutrition, physical activity and colorectal cancer. London: World Cancer Research Fund;2018. cited 2019 December 1. Available from:
https://www.wcrf.org/diet-and-cancer/.
13. Fleischauer AT, Poole C, Arab L. Garlic consumption and cancer prevention: meta-analyses of colorectal and stomach cancers. Am J Clin Nutr. 2000; 72:1047–1052. PMID:
11010950.

14. Hu JY, Hu YW, Zhou JJ, Zhang MW, Li D, Zheng S. Consumption of garlic and risk of colorectal cancer: an updated meta-analysis of prospective studies. World J Gastroenterol. 2014; 20:15413–15422. PMID:
25386091.

15. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions. Hoboken (NJ): John Wiley & Sons;2019.
16. Chiavarini M, Minelli L, Fabiani R. Garlic consumption and colorectal cancer risk in man: a systematic review and meta-analysis. Public Health Nutr. 2016; 19:308–317. PMID:
25945653.

17. Kodali RT, Eslick GD. Meta-analysis: does garlic intake reduce risk of gastric cancer? Nutr Cancer. 2015; 67:1–11. PMID:
25411831.

18. Heine-Bröring RC, Winkels RM, Renkema JM, Kragt L, van Orten-Luiten AC, Tigchelaar EF, Chan DS, Norat T, Kampman E. Dietary supplement use and colorectal cancer risk: a systematic review and meta-analyses of prospective cohort studies. Int J Cancer. 2015; 136:2388–2401. PMID:
25335850.

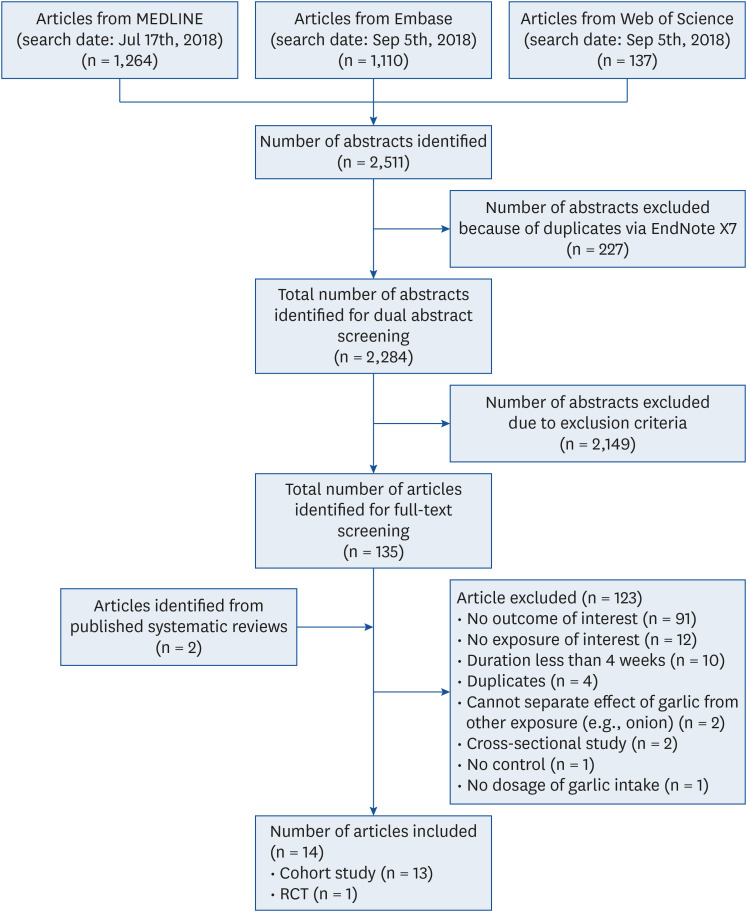
19. Wallace BC, Small K, Brodley CE, Lau J, Trikalinos TA. Deploying an interactive machine learning system in an evidence-based practice center: abstrackr. In : Proceedings of the 2nd ACM SIGHIT International Health Informatics Symposium; 2012 Jan 28–30; Miami (FL), USA. New York (NY): Association for Computing Machinery;2012. p. 819–824. DOI:
10.1145/2110363.2110464.
20. Wells GA, O'Connell D, Peterson J, Welch V, Lossos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Ottawa: Ottawa Hospital Research Institute;2011.
21. Higgins JP, Sterne JA, Savovic J, Page MJ, Hróbjartsson A, Boutron I, Reeves B, Eldridge S. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst Rev. 2016; 10:29–31.
22. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement 2009. place unknown: PRISMA;c2021. cited 2020 October 11. Available from:
http://www.prisma-statement.org/.
23. American Diabetes Association. Introduction: The American Diabetes Association's (ADA) evidence-based practice guidelines, standards, and related recommendations and documents for diabetes care. Diabetes Care. 2012; 35(Suppl 1):S1–S2. PMID:
22187466.
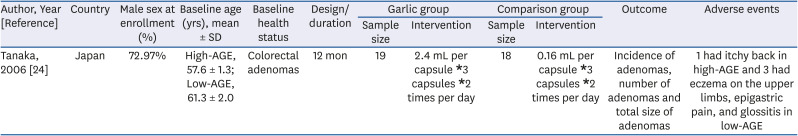
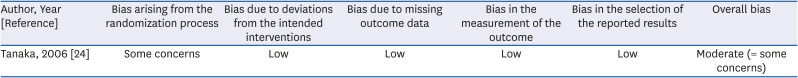
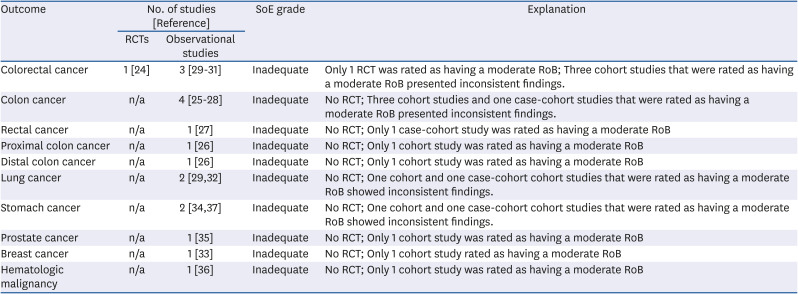
24. Tanaka S, Haruma K, Yoshihara M, Kajiyama G, Kira K, Amagase H, Chayama K. Aged garlic extract has potential suppressive effect on colorectal adenomas in humans. J Nutr. 2006; 136:821S–826S. PMID:
16484573.

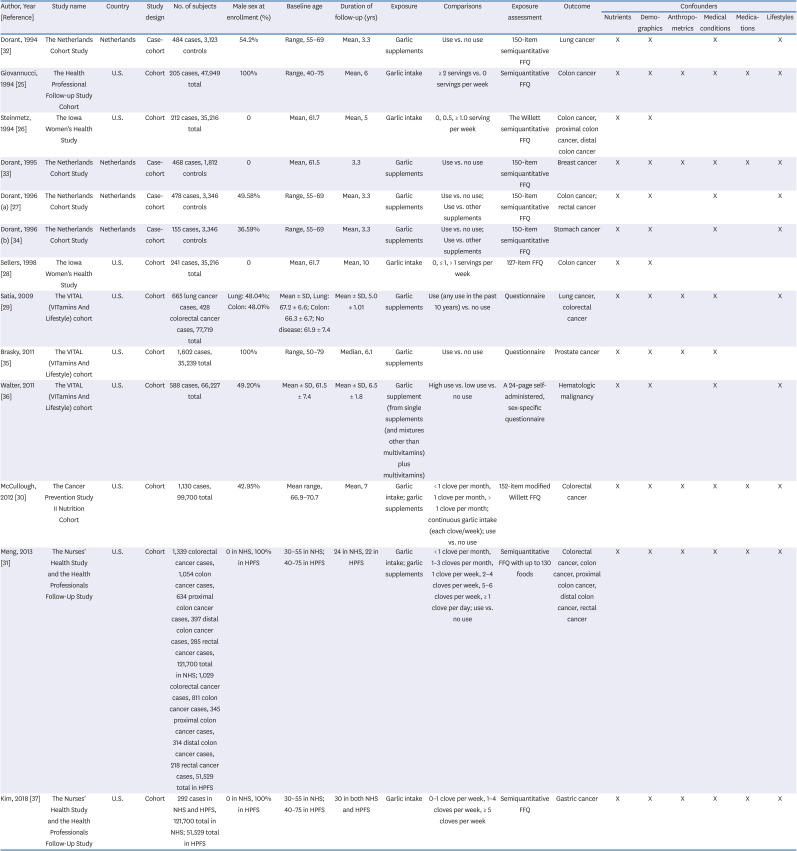
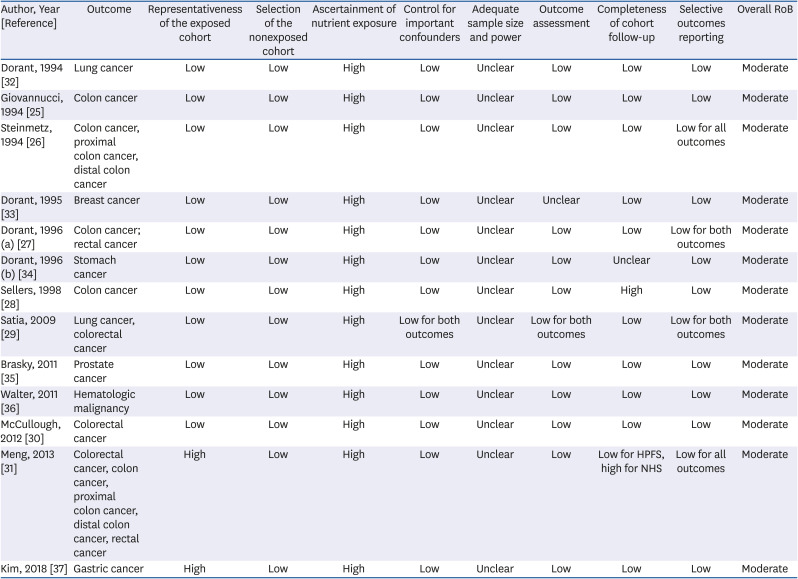
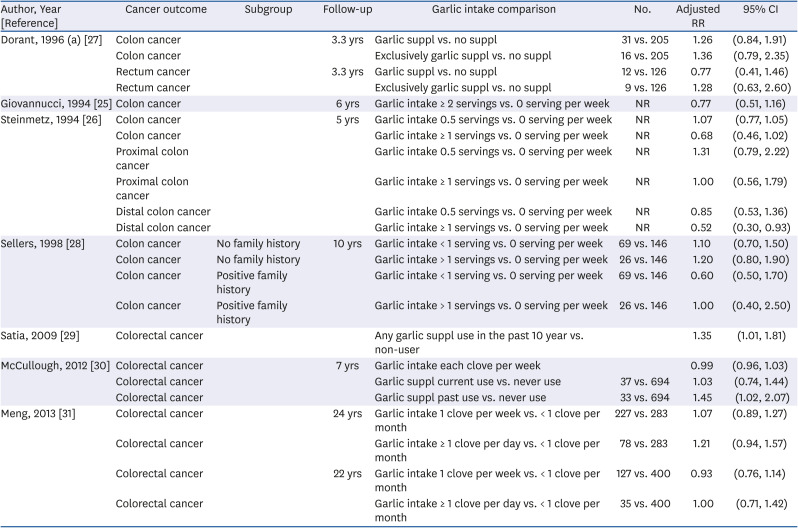
25. Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Ascherio A, Willett WC. Intake of fat, meat, and fiber in relation to risk of colon cancer in men. Cancer Res. 1994; 54:2390–2397. PMID:
8162586.
26. Steinmetz KA, Kushi LH, Bostick RM, Folsom AR, Potter JD. Vegetables, fruit, and colon cancer in the Iowa Women's Health Study. Am J Epidemiol. 1994; 139:1–15. PMID:
8296768.

27. Dorant E, van den Brandt PA, Goldbohm RA. A prospective cohort study on the relationship between onion and leek consumption, garlic supplement use and the risk of colorectal carcinoma in the Netherlands. Carcinogenesis. 1996; 17:477–484. PMID:
8631133.

28. Sellers TA, Bazyk AE, Bostick RM, Kushi LH, Olson JE, Anderson KE, Lazovich D, Folsom AR. Diet and risk of colon cancer in a large prospective study of older women: an analysis stratified on family history (Iowa, United States). Cancer Causes Control. 1998; 9:357–367. PMID:
9794167.
29. Satia JA, Littman A, Slatore CG, Galanko JA, White E. Associations of herbal and specialty supplements with lung and colorectal cancer risk in the VITamins And Lifestyle study. Cancer Epidemiol Biomarkers Prev. 2009; 18:1419–1428. PMID:
19423520.

30. McCullough ML, Jacobs EJ, Shah R, Campbell PT, Gapstur SM. Garlic consumption and colorectal cancer risk in the CPS-II Nutrition Cohort. Cancer Causes Control. 2012; 23:1643–1651. PMID:
22915096.

31. Meng S, Zhang X, Giovannucci EL, Ma J, Fuchs CS, Cho E. No association between garlic intake and risk of colorectal cancer. Cancer Epidemiol. 2013; 37:152–155. PMID:
23265869.

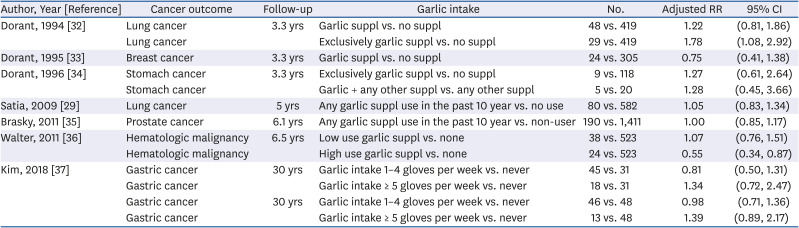
32. Dorant E, van den Brandt PA, Goldbohm RA. A prospective cohort study on Allium vegetable consumption, garlic supplement use, and the risk of lung carcinoma in The Netherlands. Cancer Res. 1994; 54:6148–6153. PMID:
7954460.
33. Dorant E, van den Brandt PA, Goldbohm RA. Allium vegetable consumption, garlic supplement intake, and female breast carcinoma incidence. Breast Cancer Res Treat. 1995; 33:163–170. PMID:
7749142.

34. Dorant E, van den Brandt PA, Goldbohm RA, Sturmans F. Consumption of onions and a reduced risk of stomach carcinoma. Gastroenterology. 1996; 110:12–20. PMID:
8536847.

35. Brasky TM, Kristal AR, Navarro SL, Lampe JW, Peters U, Patterson RE, White E. Specialty supplements and prostate cancer risk in the VITamins And Lifestyle (VITAL) cohort. Nutr Cancer. 2011; 63:573–582. PMID:
21598177.

36. Walter RB, Brasky TM, Milano F, White E. Vitamin, mineral, and specialty supplements and risk of hematologic malignancies in the prospective VITamins And Lifestyle (VITAL) study. Cancer Epidemiol Biomarkers Prev. 2011; 20:2298–2308. PMID:
21803844.

37. Kim H, Keum N, Giovannucci EL, Fuchs CS, Bao Y. Garlic intake and gastric cancer risk: results from two large prospective US cohort studies. Int J Cancer. 2018; 143:1047–1053. PMID:
29569711.

38. Nicastro HL, Ross SA, Milner JA. Garlic and onions: their cancer prevention properties. Cancer Prev Res (Phila). 2015; 8:181–189. PMID:
25586902.

39. Arunkumar A, Vijayababu MR, Srinivasan N, Aruldhas MM, Arunakaran J. Garlic compound, diallyl disulfide induces cell cycle arrest in prostate cancer cell line PC-3. Mol Cell Biochem. 2006; 288:107–113. PMID:
16691315.

40. Schaffer EM, Liu JZ, Green J, Dangler CA, Milner JA. Garlic and associated allyl sulfur components inhibit N-methyl-N-nitrosourea induced rat mammary carcinogenesis. Cancer Lett. 1996; 102:199–204. PMID:
8603370.

41. Belloir C, Singh V, Daurat C, Siess MH, Le Bon AM. Protective effects of garlic sulfur compounds against DNA damage induced by direct- and indirect-acting genotoxic agents in HepG2 cells. Food Chem Toxicol. 2006; 44:827–834. PMID:
16595265.

42. Xiao D, Pinto JT, Gundersen GG, Weinstein IB. Effects of a series of organosulfur compounds on mitotic arrest and induction of apoptosis in colon cancer cells. Mol Cancer Ther. 2005; 4:1388–1398. PMID:
16170031.

43. Ueda S, Masutani H, Nakamura H, Tanaka T, Ueno M, Yodoi J. Redox control of cell death. Antioxid Redox Signal. 2002; 4:405–414. PMID:
12215208.

44. Yi L, Su Q. Molecular mechanisms for the anti-cancer effects of diallyl disulfide. Food Chem Toxicol. 2013; 57:362–370. PMID:
23583486.

45. Fleischauer AT, Arab L. Garlic and cancer: a critical review of the epidemiologic literature. J Nutr. 2001; 131:1032S–1040S. PMID:
11238811.

46. Jacobs DR Jr, Gross MD, Tapsell LC. Food synergy: an operational concept for understanding nutrition. Am J Clin Nutr. 2009; 89:1543S–1548S. PMID:
19279083.

47. Shim JS, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014; 36:e2014009. PMID:
25078382.

48. Olafsdottir AS, Thorsdottir I, Gunnarsdottir I, Thorgeirsdottir H, Steingrimsdottir L. Comparison of women's diet assessed by FFQs and 24-hour recalls with and without underreporters: associations with biomarkers. Ann Nutr Metab. 2006; 50:450–460. PMID:
16877864.

49. Prati P, Henrique CM, de Souza AS, da Silva VSN, Pacheco MTB. Evaluation of allicin stability in processed garlic of different cultivars. Food Sci Technol. 2014; 34:623–628.

50. Marchese A, Barbieri R, Sanches-Silva A, Daglia M, Nabavi SF, Jafari NJ, Izadi M, Ajami M, Nabavi SM. Antifungal and antibacterial activities of allicin: a review. Trends Food Sci Technol. 2016; 52:49–56.

51. Praticò G, Gao Q, Manach C, Dragsted LO. Biomarkers of food intake for
Allium vegetables. Genes Nutr. 2018; 13:34. PMID:
30607216.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download