INTRODUCTION
With the advancement in medicine came a rise in demand for medical resources, thus leading to a sharp increase in healthcare expenditures.
1 This situation created a need for an efficient utilization of medical resources. Thus, the concept of the healthcare delivery system was introduced.
2 In the Republic of Korea, to ensure the efficient distribution and use of medical resources, the healthcare delivery system divides the hospitals into clinics, hospitals, general hospitals, and tertiary referral general hospitals (tertiary hospitals) according to referral levels.
3
Tertiary hospitals are used principally for the treatment of seriously ill patients. Owing to the complexity of the required treatments, a higher rate of insurance reimbursement is disbursed to tertiary hospitals. However, when patients with non-severe diseases are treated in a tertiary hospital, this high payment rate results in an increase in medical expenses. Therefore, the Korean Ministry of Health and Welfare designed a system that considers the severity of patients' diseases. The Ministry issues a penalty to a tertiary hospital if a patient is treated with a low severity disease. In this system, the diseases that are the most difficult to diagnose/treat are classified into the “disease group requiring specialized management.”
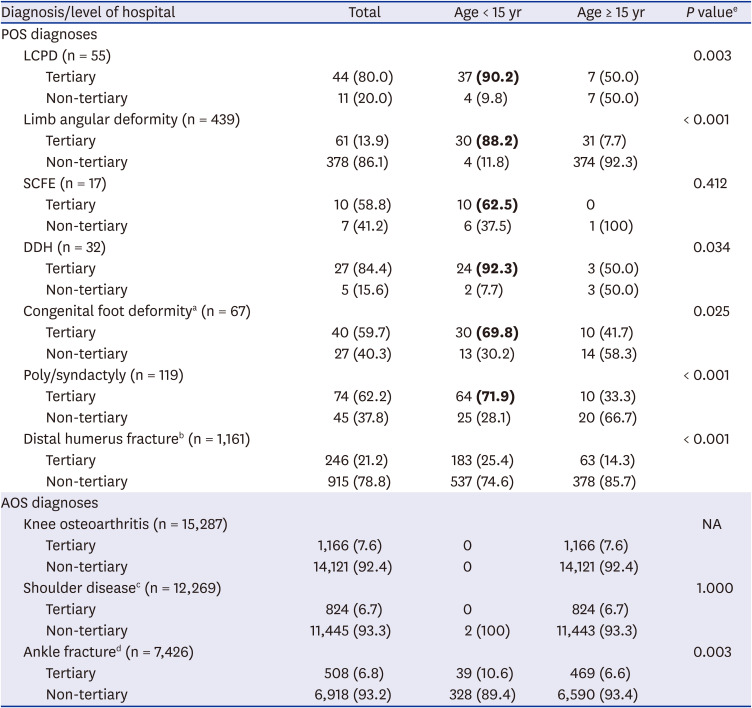
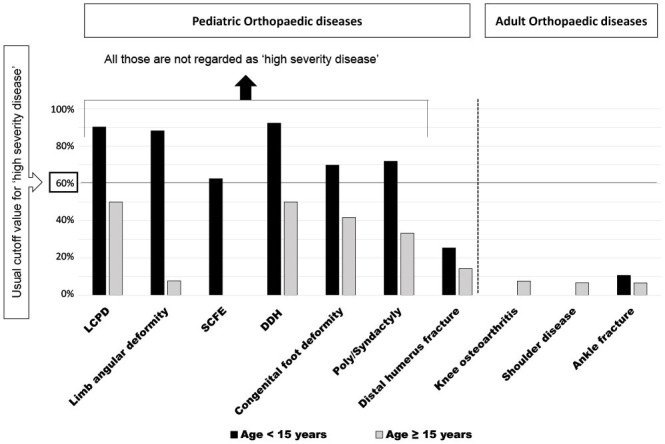
4 The authors have referred to these as ‘severe diseases’ or the ‘severe disease group’ and others as ‘non-severe diseases’ or the ‘non-severe disease group’ throughout the manuscript. There are various criteria for establishing hospital designations; however, the main factor determining disease severity is the nationwide admission rate. A high rate (usually > 60%) of admissions to tertiary hospitals indicates a disease of high severity. Such diseases are prone to be included in the severe disease group.
5 For example, if 100 people were hospitalized for a specific disease and 60 of them were hospitalized at a tertiary hospital, the admission rate for tertiary hospitals would be 60%.
Pediatric orthopaedic surgery (POS) is a subspecialty of orthopaedic surgery, treating various orthopaedic diseases in children. Many of these diseases are rare and often difficult to diagnose appropriately.
6 If these diseases are not treated properly, serious complications could occur.
7 This is consistent with the definition of diseases included in the severe disease group. However, in the Korean medical system, the current criteria for the POS disease grouping do not significantly consider factors relevant to growing children such as the patient's age.
48 It does not account for differences between pediatric and general orthopaedic diseases, and most POS diseases are also classified into the ‘non-severe disease’ as general orthopaedic diseases.
9
Thus, investigating the admission rates to tertiary hospitals for POS diseases will assist in determining whether POS diseases are underestimated in the current criteria for this disease grouping, because it is one of the important selection criteria for the severe disease group.
5 However, it would be difficult to obtain generalizable results if individual hospital-based data were used for analysis as medical situations differ among hospitals. To obtain more reliable and accurate results, the use of data from a nationwide database of claim records is appropriate.
This study aimed to investigate the rates of admission to tertiary and non-tertiary hospitals for POS diseases and to compare these admission rates with those of adult orthopaedic surgery (AOS) diseases. For this, we determined the most frequent POS and AOS diagnoses. Nationwide sample data were used for analysis.
Go to :

DISCUSSION
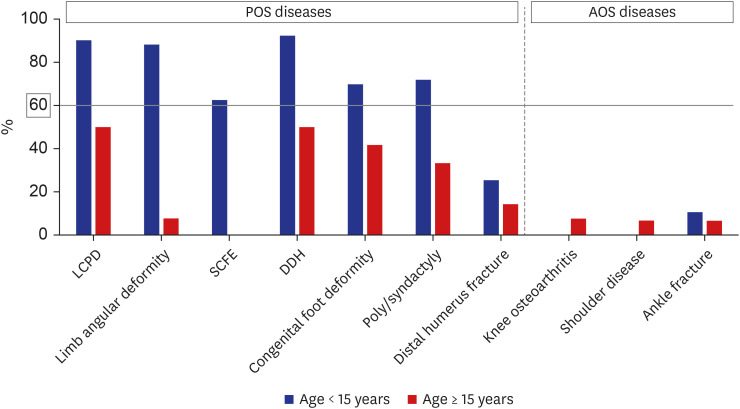
This study investigated the admission rates for representative POS diseases using national sampling data. Seven frequent POS diagnoses were chosen as representatives. An additional three frequent AOS diagnoses were selected for comparison. Most frequent POS diagnoses involved high rates of admission to tertiary hospitals among patients aged < 15 years. Conversely, for patients aged ≥ 15 years with frequent AOS diagnoses, the tertiary hospital admission rates were lower than 10%. In summary, frequent POS diagnoses were associated with a higher tertiary hospital admission rate than frequent AOS diagnoses (general orthopaedic diagnoses).
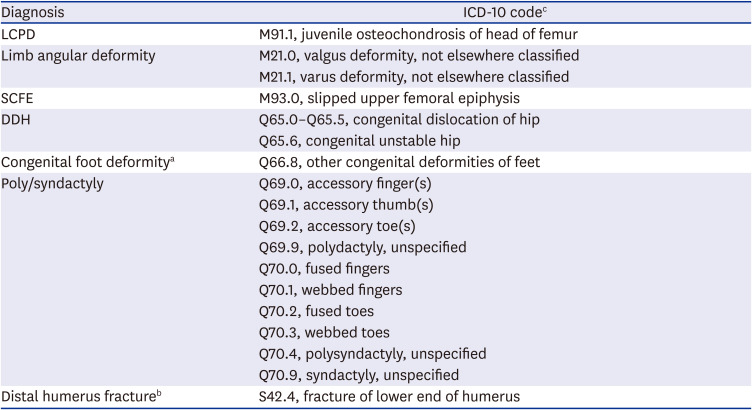
One of the important determinants in this study was the selection of representative POS diseases. This process was based on a report by the Korean Pediatric Orthopaedic Society, which examined pediatric orthopaedic patients admitted to four tertiary hospitals in Korea between 2018 and 2019 (not published). This report sought to identify the frequent POS diagnoses that were associated with a high probability of surgical intervention. The authors reviewed these diagnoses to identify those that were pediatric orthopaedic-specific, occurred frequently, and required surgical intervention. We also used published literature.
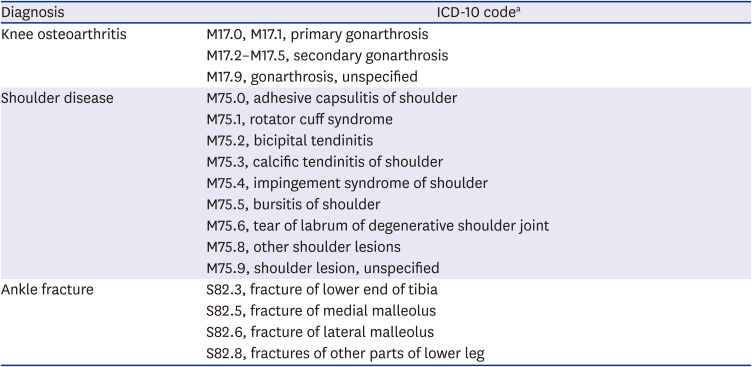
71112 Moreover, it was also important to select representative general orthopaedic diseases that could be compared with frequent POS diagnoses. Therefore, the three most common general orthopaedic diagnoses, i.e., knee osteoarthritis (8th), shoulder disease (10th), and ankle fracture (25th), that are routinely managed in orthopaedic departments for adults were selected. These were deemed as AOS diagnoses using national data of all hospitalized patients in Korea between 2018 and 2019.
16 Based on the previous literature, it was confirmed that these diagnoses could serve as representative general orthopaedic diseases.
131415 These POS and AOS diagnoses were similar in that they were the most frequently observed diseases and were selected using data of Korean patients hospitalized between 2018 and 2019.
Tertiary hospital admission rates for frequent POS diagnoses, except for distal humerus fractures, were 62.5–92.3% among patients aged < 15 years. Among those diagnoses, only some of distal humerus fractures are currently classified as the ‘severe disease’ if the fractures involve the articular surface or accompanying neurovascular compromise. All the other diagnoses are classified as the ‘non-severe disease’. Considering that tertiary hospital admission rates for the severe disease group are usually 60–70%,
521 these rates are quite high. This suggests that the severity of POS diseases is underestimated and that these diseases should be uniquely assessed using different criteria from those for general orthopaedic diseases.
The numbers of patients aged < 15 years with frequent AOS diagnoses were very small. In particular, the M code, which indicates musculoskeletal system or connective tissue disease, was extremely rare among pediatric patients (0 out of 15,287 cases of knee osteoarthritis and 2 out of 12,269 cases of shoulder disease). In addition, less than 5% of ankle fracture cases were observed among pediatric patients (367/7,426, 4.9%). Owing to this small proportion of children, most orthopaedic diseases are not distinguished between children and adults for administrative convenience. However, as there are obvious differences in the admission rates to tertiary hospitals, the ‘age’ factor is necessary to uniquely assess POS diseases on a different basis from adult orthopaedic diseases.
Most POS diseases are diverse, relatively rare, and occasionally accompanied by congenital diseases. These conditions may require consultations from other departments.
672223 Moreover, it is occasionally difficult to differentiate between the normal physiologic changes and pathologic presentations in children. This is because their musculoskeletal characteristics change continuously.
2425 In addition, the growth in children is associated with the possibility of limb length discrepancy or angular deformity during follow-up.
26 Thus, more specialized knowledge and judgment from practitioners are required in dealing with POS diseases. Further, the aforementioned characteristics of POS diseases are consistent with those of the ‘disease group requiring specialized management.’ These are defined as rare diseases, those with high complication and mortality rates, those that are difficult to diagnosis, or those that require research. Currently, it is recommended that surgical treatment for POS diseases is carried out at a tertiary hospital with professional medical personnel in attendance to prepare for potential risks during surgery.
27 In addition, the total pediatric orthopaedic cases in very large hospitals that primarily deal with severe diseases is increasing worldwide.
28 This trend also suggests that POS diseases require treatment at tertiary hospitals.
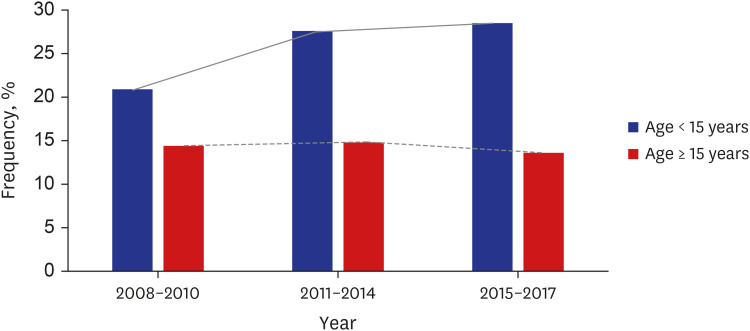
The distal humerus fracture, one of the most common fractures in children, was the only POS diagnosis that had an S code (a diagnostic code for traumatic diseases). In the present results, the tertiary hospital admission rate for distal humerus fractures in patients aged < 15 years was 25.4%. This was significantly lower than those for other POS diagnoses. Therefore, we also analyzed the change in the trend of tertiary hospital admission rates for distal humerus fractures. The tertiary hospital admission rates for patients aged < 15 years have continued to increase over the past 10 years. That is, though the admission rate for traumatic POS diseases in patients aged < 15 years was relatively low, it has been increasing continuously.
The authors also suggested possible explanations for the low admission rate of pediatric distal humerus fractures. The data used in this study are diagnostic codes for admission only, not for surgery. The data cannot distinguish whether a patient was admitted to a hospital for surgery or for conservative management. Usually in the orthopaedic field, hospitalization for conservative management is much more common in non-tertiary hospitals than in tertiary hospitals. Therefore, the authors believe that the admission rate in tertiary hospitals will be higher when using exclusive data for surgical admissions. This would be also evident for traumatic cases such as distal humerus fractures. Another explanation could be that the current diagnostic code does not indicate whether the articular surface or growth plate is involved. If there was a distinctive indication for articular or physeal involvement, the admission rates in tertiary hospitals for these injuries may have been higher owing to their diagnostic difficulty
2930 and poor prognosis.
3031 Further research with more detailed information are surely needed.
Frequent POS diagnoses resulted in a high admission rate at tertiary hospitals. Nevertheless, there are no classification criteria according to patient age.
8 Most POS diseases are not included in the severe disease group,
49 all the frequent POS diagnoses are currently classified into the ‘non-severe disease’ except the distal humerus fractures specifically involving the joint or neurovascular structure. In the current Korean medical reimbursement system, tertiary hospitals are penalized if the number of admitted cases of POS diseases are high. This is because most of these cases are classified as non-severe diseases. This fact forces tertiary hospital administrators to decrease the proportion of POS patients for the benefit of the hospital's financial survival. Eventually, this may negatively affect patients who require high-level professional treatment. Ultimately, this may result in great social loss.
32
There are some limitations to this study. First, NHISS nationwide samples are randomized data obtained from 1 million people per year. It is a large-scale survey and is representative of the population. However, it includes only a segment of the entire population. This leads to the possibility of sampling errors. The second consideration involves the method for selecting the representative diseases of POS and AOS. We assessed frequent admissions for pediatric and orthopaedic diagnoses between 2018 and 2019. Three pediatric orthopaedic surgeons selected the representative diseases after reviewing the literature. However, this involves the subjective judgment of the authors. Therefore, attention should be paid to selection bias when interpreting the results. Finally, this study was conducted only based on data from Republic of Korea. Thus, it may not be generalized to patients in countries with different socioeconomic medical conditions.
Conclusively, for patients aged < 15 years, most POS diagnoses had higher tertiary hospital admission rates (> 60%). Though pediatric orthopaedic fracture is associated with a high non-tertiary hospital admission rate, tertiary hospital admission rates of children with this fracture are steadily increasing. Considering that the tertiary hospital admission rate is the most important factor in the classification of disease severity, POS diseases seem to be underestimated in terms of severity. Unfortunately, this may lead to a tendency toward an intentional reduction in the treatment of patients with POS diseases at tertiary hospitals. Therefore, POS diseases should be classified using different criteria from those used to classify general AOS diseases.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download