This article has been
cited by other articles in ScienceCentral.
Abstract
Background
To facilitate evidence-based policy-making on safe reopening of higher education facilities, there is an urgent need to assess baseline profile of coronavirus disease 2019 (COVID-19) incidents within the university/college settings. We aimed to describe the epidemiology of COVID-19 in universities/colleges in Seoul Metropolitan Area during COVID-19 pandemic period.
Methods
Among the 38 universities in Seoul, 23 have agreed to participate in the study. Confirmed COVID-19 cases were identified from individual-level case reports submitted to the universities and to the health authorities from February 1, 2020, to June 30, 2021. Through the linkage with the Central Disease Control Headquarters' database, number of secondary infected cases (both within and outside of the campus) were counted.
Results
Between February 2020 and June 2021, a total of 827 COVID-19 cases were confirmed and reported in the universities across Seoul Metropolitan City. Generally, the community-associated cases had peaks preceding the university/college-associated. Of those with the documented clinical parameters, 38.6% of the cases were asymptomatic. Among them, 93% were potentially exposed off-campus, and 87.7% of the cases had not produced the secondary infection cases.
Conclusion
In the setting of rigorous infection prevention measures in combination with on- and off- hybrid classes, COVID-19 incidences and outbreaks were limited in university and college campus area across Seoul Metropolitan Area. The evidence around the infection preventive measures in higher education facilities in Seoul Metropolitan Area, suggest insignificant impact on community transmission.
Keywords: Coronavirus, COVID-19, University, College, Epidemiology
INTRODUCTION
Closing of educational facilities due to coronavirus disease 2019 (COVID-19) pandemic have resulted significant disruptions to higher educations across the globe.
12 Young adults, although have shown least amount of concern on severe COVID-19 compared to elderly population, are among the most affected by the societal impact and economic crisis as a result of COVID-19 responding measures.
3 While there is evidence that young adults are effective at transmitting the severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), many outbreaks have occurred at locations without protective measures in place, outside of the educational settings.
45
Since mid-March 2020, many universities and colleges in South Korea have shifted to online learning environment.
6 Unfortunately, initial reports show that the core competencies and academic achievements of students were significantly lower in 2020 than before the COVID-19 pandemic.
78 Without clear and consistent public health leadership and guidance on COVID-19 preventive measures in universities/colleges, individual campuses are left with non-standardized, uncoordinated responses which then result in risk of transmission to the community.
910
To facilitate evidence-based policy-making on safe reopening of higher education facilities, there is an urgent need to assess baseline profile of COVID-19 incidents within the university/college settings. In such view, we aimed to describe the epidemiology of COVID-19 in universities/colleges in Seoul Metropolitan Area during COVID-19 pandemic period, therefore to have better understanding on transmission risks and to inform policy-making in regard to on-campus preventive measures.
METHODS
As the COVID-19 outbreak trend and the population size of universities vary for each region, the government allowed autonomy to local governments and universities when deciding the specifics of managing response scheme, operating online and offline classes in parallel, splitting each class into morning and afternoon groups, and implementing flexible class hours. In specific, the methods include: 1) government's on-site support offered to colleges and universities as part of COVID-19 pandemic (February-March 2020); 2) postponement of school openings and providing online classes (February 2020-); 3) plan to provide financial support for disadvantaged college students developed (April 2020); 4) stepwise reopening of the classes (May 2020); 5) disinfection guidelines (May 2020); 6) physical spacing and density managements (May 2020); and 7), tracked international students from the point of their arrival (February 2020-).
11
Among the 38 universities in Seoul, 23 have agreed to participate in the study (
Supplementary Fig. 1). The background population include: 234,891 undergraduate students, 83,067 graduate students, 42,712 professors/lecturers and 10,624 staffs. Individual university/college's COVID-19 surveillance set linked to the Central Disease Control Headquarters' database was used to identify the epidemiologic trend of COVID-19 in universities in Seoul. The linked database was derived from epidemiologic investigation files, collected through a legally mandated public health investigation under the authority of the Korean Infectious Diseases Control and Prevention Act (No. 12444 and No. 13392).
12 Confirmed COVID-19 cases were identified from individual-level case reports submitted to the universities and to the health authorities from February 1, 2020, to June 30, 2021. The incidence density on new cases from corresponding age group during each epidemiologic week was calculated. Following the merging of datasets, personal identifiable data were deleted and were not included in the analyses.
Demographics including age, gender, nationality, and status (undergrad student, grad student, professor/lecturer, staffs) were assessed. For those available, clinical parameters were collected during the encounter of the cases during COVID-19 laboratory testing. The routes of testing (symptom-based, contact-based, random screening, inbound travelers screening) were assessed. School seasons during the encounter of the cases were classified as: online class, offline class, and summer/winter break. Potential routes of transmission were classified as: off-campus vs. on-campus (large lecture hall, midsize/small lecture room, lab spaces, restaurant/cafeteria) based on the epidemiological investigation. Self-reported mean daily time of stay at the university/college was assessed, and was stratified into: < 3 hours, 3–6 hours, and > 6 hours. Through the linkage with the Central Disease Control Headquarters' database, number of secondary infected cases (both within and outside of the campus) were counted.
Ethics statement
This study was approved by the Korea University Institutional Review Board (IRB No. 2021AN0421).
RESULTS
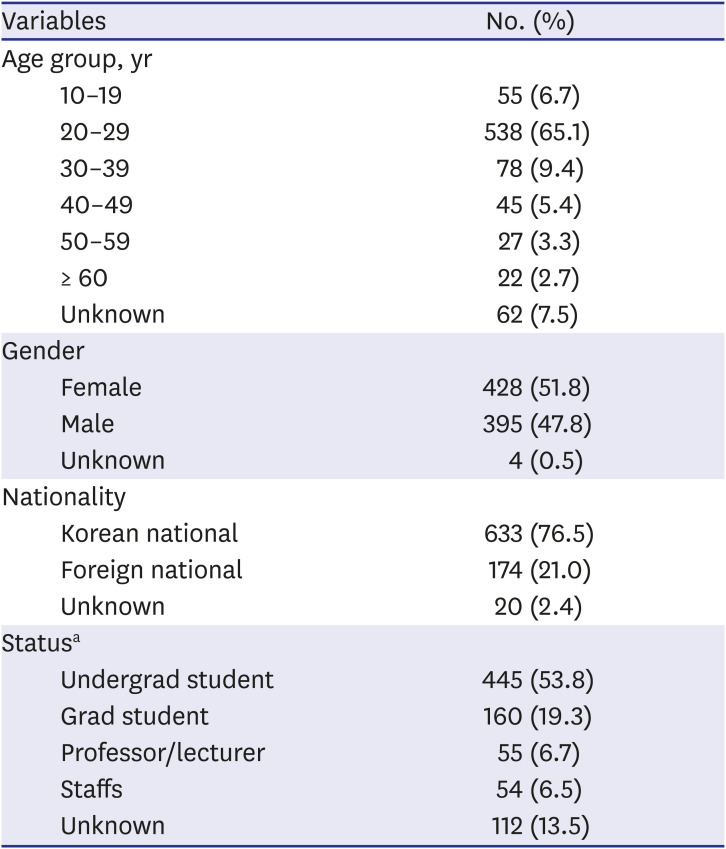
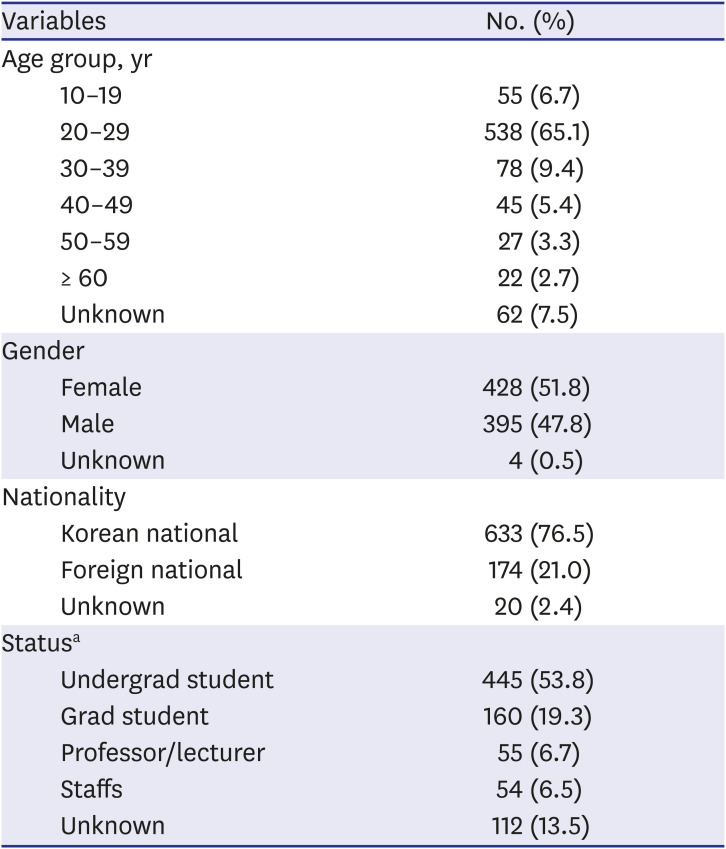
Between February 2020 and June 2021, a total of 827 COVID-19 cases were confirmed and reported in the universities across Seoul Metropolitan City. The age group of 20–29 years comprised 65.1% of the cases, with 21% foreign nationals and 53.8% of undergrad students (
Table 1).
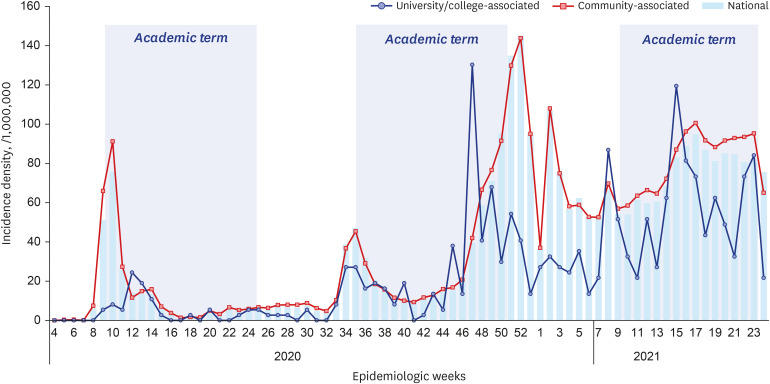
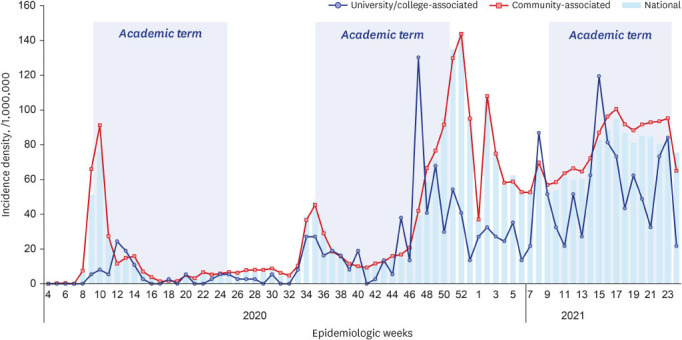
Fig. 1 depicts the epidemic curve for community-associated versus university/college-associated COVID-19 cases in Seoul Metropolitan Area, during the surveillance weeks. Generally, the community-associated cases had peaks preceding the university/college-associated cases; however, with exception during the 46-52nd surveillance week of the year 2020. Between 4th epidemiologic week of 2020 and 24th epidemiologic week of 2021, the average incidence density for community-associated student cases was 41 per 1 million; university-associated student cases was 25 per 1 million; and national 20–29 years cases was 47 per 1 million.
Fig. 1
Epidemic curve for community-associated vs. university/college-associated severe acute respiratory syndrome-coronavirus-2 laboratory-confirmed cases, Seoul Metropolitan Area, Feb. 2020–Jun. 2021.
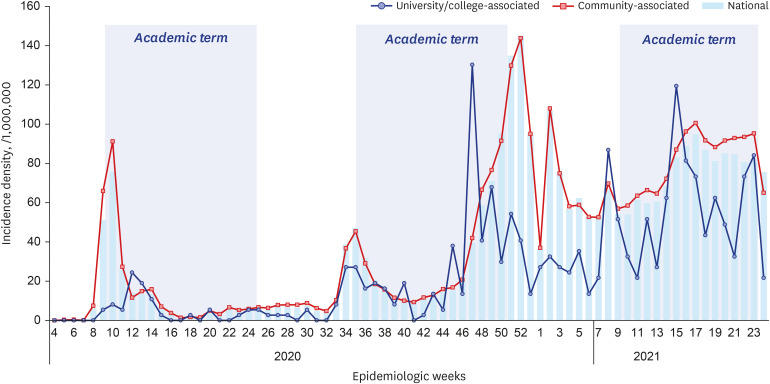

Table 1
Demographic characteristics of university/college-associated coronavirus disease 2019 laboratory-confirmed cases, Seoul Metropolitan Area, Feb. 2020–Jun. 2021
|
Variables |
No. (%) |
|
Age group, yr |
|
|
10–19 |
55 (6.7) |
|
20–29 |
538 (65.1) |
|
30–39 |
78 (9.4) |
|
40–49 |
45 (5.4) |
|
50–59 |
27 (3.3) |
|
≥ 60 |
22 (2.7) |
|
Unknown |
62 (7.5) |
|
Gender |
|
|
Female |
428 (51.8) |
|
Male |
395 (47.8) |
|
Unknown |
4 (0.5) |
|
Nationality |
|
|
Korean national |
633 (76.5) |
|
Foreign national |
174 (21.0) |
|
Unknown |
20 (2.4) |
|
Statusa
|
|
|
Undergrad student |
445 (53.8) |
|
Grad student |
160 (19.3) |
|
Professor/lecturer |
55 (6.7) |
|
Staffs |
54 (6.5) |
|
Unknown |
112 (13.5) |

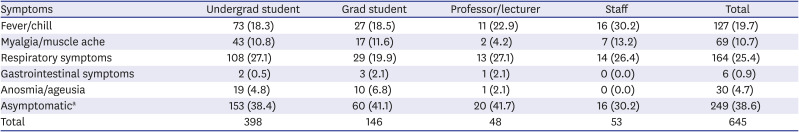
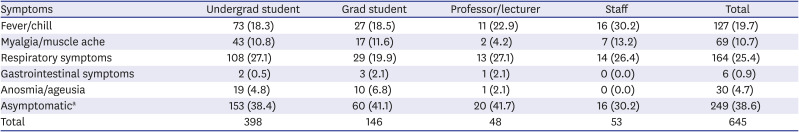
Of those with the documented clinical parameters, respiratory symptom (25.4%) was the most common symptom, followed by fever/chill (19.7%), and myalgia/muscle ache (10.7%) (
Table 2). Of note, 38.6% of the cases were confirmed with COVID-19 while they had no symptoms ascribed to the infections.
Table 2
Clinical parameters of university/college-associated severe acute respiratory syndrome-coronavirus-2 laboratory-confirmed cases, Seoul Metropolitan Area, Feb. 2020–Jun. 2021
|
Symptoms |
Undergrad student |
Grad student |
Professor/lecturer |
Staff |
Total |
|
Fever/chill |
73 (18.3) |
27 (18.5) |
11 (22.9) |
16 (30.2) |
127 (19.7) |
|
Myalgia/muscle ache |
43 (10.8) |
17 (11.6) |
2 (4.2) |
7 (13.2) |
69 (10.7) |
|
Respiratory symptoms |
108 (27.1) |
29 (19.9) |
13 (27.1) |
14 (26.4) |
164 (25.4) |
|
Gastrointestinal symptoms |
2 (0.5) |
3 (2.1) |
1 (2.1) |
0 (0.0) |
6 (0.9) |
|
Anosmia/ageusia |
19 (4.8) |
10 (6.8) |
1 (2.1) |
0 (0.0) |
30 (4.7) |
|
Asymptomatica
|
153 (38.4) |
60 (41.1) |
20 (41.7) |
16 (30.2) |
249 (38.6) |
|
Total |
398 |
146 |
48 |
53 |
645 |

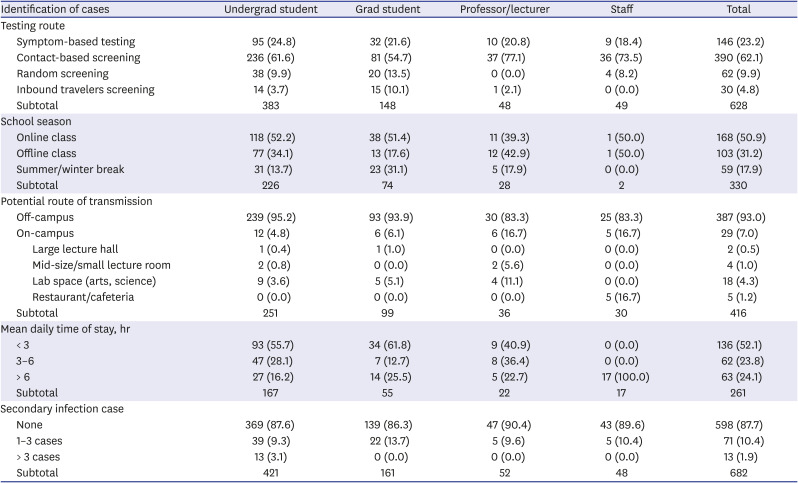
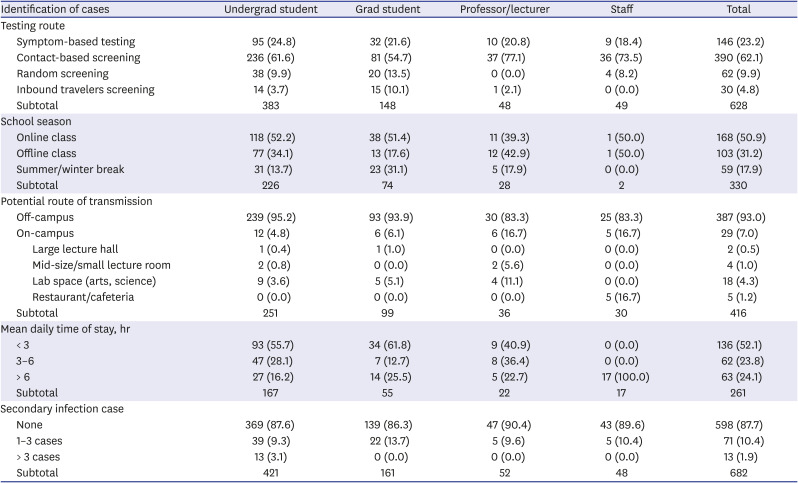
A total of 62.1% of the cases were identified through contact-based screening, followed by 23.2% with symptom-based testing and 9.9% of random screened cases (
Table 3). Of them, 50.9% were infected during the online class season, followed by 31.2% during offline class season. A total of 93% of the cases were potentially exposed off-campus, while lab spaces (arts, sciences) comprised largest portion of the on-campus transmissions (4.3% of all). 52.1% of infected cases had spent less than 3 hours per day on average at the campus. 87.7% of the cases had not produced the secondary infection cases, while 10.4% had resulted 1–3 cases of secondary cases. Among 144 cases identified to have linkage with off-campus clusters, 58 cases were associated with community-based clusters, seven cases were with imported cluster, and four cases were associated with healthcare-associated transmission.
Table 3
Transmission of university/college-associated severe acute respiratory syndrome-coronavirus-2 laboratory-confirmed cases, Seoul Metropolitan Area, Feb. 2020–Jun. 2021
|
Identification of cases |
Undergrad student |
Grad student |
Professor/lecturer |
Staff |
Total |
|
Testing route |
|
|
|
|
|
|
Symptom-based testing |
95 (24.8) |
32 (21.6) |
10 (20.8) |
9 (18.4) |
146 (23.2) |
|
Contact-based screening |
236 (61.6) |
81 (54.7) |
37 (77.1) |
36 (73.5) |
390 (62.1) |
|
Random screening |
38 (9.9) |
20 (13.5) |
0 (0.0) |
4 (8.2) |
62 (9.9) |
|
Inbound travelers screening |
14 (3.7) |
15 (10.1) |
1 (2.1) |
0 (0.0) |
30 (4.8) |
|
Subtotal |
383 |
148 |
48 |
49 |
628 |
|
School season |
|
|
|
|
|
|
Online class |
118 (52.2) |
38 (51.4) |
11 (39.3) |
1 (50.0) |
168 (50.9) |
|
Offline class |
77 (34.1) |
13 (17.6) |
12 (42.9) |
1 (50.0) |
103 (31.2) |
|
Summer/winter break |
31 (13.7) |
23 (31.1) |
5 (17.9) |
0 (0.0) |
59 (17.9) |
|
Subtotal |
226 |
74 |
28 |
2 |
330 |
|
Potential route of transmission |
|
|
|
|
|
|
Off-campus |
239 (95.2) |
93 (93.9) |
30 (83.3) |
25 (83.3) |
387 (93.0) |
|
On-campus |
12 (4.8) |
6 (6.1) |
6 (16.7) |
5 (16.7) |
29 (7.0) |
|
|
Large lecture hall |
1 (0.4) |
1 (1.0) |
0 (0.0) |
0 (0.0) |
2 (0.5) |
|
|
Mid-size/small lecture room |
2 (0.8) |
0 (0.0) |
2 (5.6) |
0 (0.0) |
4 (1.0) |
|
|
Lab space (arts, science) |
9 (3.6) |
5 (5.1) |
4 (11.1) |
0 (0.0) |
18 (4.3) |
|
|
Restaurant/cafeteria |
0 (0.0) |
0 (0.0) |
0 (0.0) |
5 (16.7) |
5 (1.2) |
|
Subtotal |
251 |
99 |
36 |
30 |
416 |
|
Mean daily time of stay, hr |
|
|
|
|
|
|
< 3 |
93 (55.7) |
34 (61.8) |
9 (40.9) |
0 (0.0) |
136 (52.1) |
|
3–6 |
47 (28.1) |
7 (12.7) |
8 (36.4) |
0 (0.0) |
62 (23.8) |
|
> 6 |
27 (16.2) |
14 (25.5) |
5 (22.7) |
17 (100.0) |
63 (24.1) |
|
Subtotal |
167 |
55 |
22 |
17 |
261 |
|
Secondary infection case |
|
|
|
|
|
|
None |
369 (87.6) |
139 (86.3) |
47 (90.4) |
43 (89.6) |
598 (87.7) |
|
1–3 cases |
39 (9.3) |
22 (13.7) |
5 (9.6) |
5 (10.4) |
71 (10.4) |
|
> 3 cases |
13 (3.1) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
13 (1.9) |
|
Subtotal |
421 |
161 |
52 |
48 |
682 |

DISCUSSION
In the setting of rigorous infection prevention measures in combination with on- and off- hybrid classes, COVID-19 incidences and outbreaks were limited in university and college campus area across Seoul Metropolitan Area. Most on-campus outbreaks had few cases per outbreak, with less than 2% affecting more than three cases on campus. More than 90% of the identified transmissions have occurred outside of the campus, and more so, 50% of the infections indeed, had happened during online class seasons. This finding is in line with studies from other countries. In Cambridge, UK, a study has found that the transmission from the university to local community was limited, and that only a small number of lineages of the virus accounted for the outbreaks, reflecting the efficacy of the university's screening policy.
13 Indeed, the findings may not be replicable in the settings without stringent on-campus infection prevention policies. A modelling study from the US suggested that the college/university outbreaks have affected neighboring communities, however, the outbreak dynamics remained manageable in the campuses with test-trace-isolate strategies.
14 An analysis using the US university/college mobile phone data have shown that re-opening a college have increased the incidence of COVID-19 in the community, however the policies limiting daily mobility interactions would prevent such spillovers.
14 Our finding showing the epidemic curve for community-transmission generally preceded the campus-transmission, albeit setting of heterogeneity in campus policy on infection preventions, may not be applicable in the setting of distant-travelling college students. A modelling estimates from the US shows that university students travelling from states to states have provided a significant contribution on inter-state transmission.
15 Continued research and data are needed to document the varying infection prevention policy relative to effects on university/college opening on community-transmissions.
Our findings suggest that nearly 40% of the identified cases did not exhibit any symptoms during the course of investigation. The hall-mark of infection prevention strategies in South Korea has been the rigorous case management through Testing-Tracing-Treatment Strategy in response to local outbreaks.
16 Although more than 60% of the cases were identified through contact-based screening, only 20% have exhibited fevers and/or chills during the time of encounter, suggesting limited value of fever-based screening, on campus. As a complimentary surveillance measure, the wastewater-based epidemiology (WBE) has been suggested a potential as an early-warning tool for determining the presence on the campus.
17 In the US, there had been case studies utilizing WBE that resulted an efficient resource for COVID-19 prevention in the universities.
18 Such WBE have shown to detect small clusters within the university campuses (dorms, buildings), suggesting a possible applicable measure to mitigate the pandemic in universities and colleges.
19
There are number limitations to this study. First, given the retrospective nature of surveillance data, this study is prone to selection bias on both directions; possible under-detection due to insensitive surveillance scheme; or potentially overestimated cases from campus visitors. Second, there was substantial variability between universities and colleges on their infection preventive measure policies, prohibiting quantitative analyses through data synthesis. Third, given the limited data on college-specific policy (on/offline, hybrid classes) and demographic profile, our data does not provide the exact rate based on the baseline population and the college-specific context. Lastly, our investigation did not distinguish the linked cases to assess the exact exposure history especially among the asymptomatic cases. It should, therefore, be interpreted with caution. Despite these limitations, our study highlights several interesting public health findings, reporting the incidence of university/collage-based cases in comparison to the incidence of community-based cases.
Collectively, the evidence around the infection preventive measures in higher education facilities in Seoul Metropolitan Area, suggest insignificant impact on community transmission. Our investigation suggests that transmission within the universities and colleges was uncommon and was not the primary cause of COVID-19 outbreak in the community. Our finding suggests that it may be possible for colleges to operate offline classes safely while controlling the transmission of COVID-19 to the community. Successful offline classes may be dependent on limiting the introduction of the SARS-CoV-2 virus to the campus, rigorous testing and tracing, and reactive closure, when needed. Further epidemiological evidence is needed to document the impact of university/college opening during the age of delta variant and vaccines, to better understand the current gap of knowledge to mitigate from COVID-19 pandemic.
ACKNOWLEDGMENTS
We thank administrative staffs and public health workers who have dedicated to collect the information, conducted epidemiologic investigation, and performed infection prevention measures in the college and university settings. Aforementioned group authors are from the Seoul Regional Universities COVID-19 Response Working Group and Korea Disease Control and Prevention Agency.
Sang-Hoon Bae, PhD (Sungkyunkwan University), Seung-Ho Cho, PhD (Soongsil University), Hong-Bum Cho (Seokyeong University), Cheon Geun Choi (Hansung University), Jee Yong Chung, PhD (Duksung Women's University), Sung Hoon Jeh, PhD (Hankuk University of Foreign Studies), Sang Wook Kang, PhD (Sangmyung University), Yu-Won Kang, PhD (Sejong University), Jayong Koo, PhD (University of Seoul), Min Gyo Koo, PhD (Seoul National University), Jae Joong Oh, PhD (Konkuk University), Kwanghyoun Park, PhD (Dongguk University), Kwi-Cheon Park, PhD (Ewha Womans University), Yeol Park, PhD (Kwangwoon University), Doh-hyung Riu, PhD (Seoul National University of Science and Technology), Soo-Hyun Ryu, PhD (Sahmyook University), In-Bo Shim, PhD (Kookmin University), Hyun Han Shin, PhD (Yonsei University), Hyeonjin Soh, PhD (Sungshin Women's University), Yun Seon Song, PhD (Sookmyung Women's University), Kang-Oh Yi, PhD (Sogang University), Soohyun Cho (Korea Disease Control and Prevention Agency), Young-Joon Park, MD, MPH (Korea Disease Control and Prevention Agency), Seonju Yi, PhD (Korea Disease Control and Prevention Agency).
References
1. Birmingham WC, Wadsworth LL, Lassetter JH, Graff TC, Lauren E, Hung M. COVID-19 lockdown: impact on college students' lives. J Am Coll Health. Forthcoming. 2021; DOI:
10.1080/07448481.2021.1909041.

2. Nurunnabi M, Almusharraf N. Social distancing and reopening universities after the COVID-19 pandemic: policy complexity in G20 countries. J Public Health Res. 2021; 9(Suppl 1):1957. PMID:
33575228.

3. Cunningham JW, Vaduganathan M, Claggett BL, Jering KS, Bhatt AS, Rosenthal N, et al. Clinical outcomes in young US adults hospitalized with COVID-19. JAMA Intern Med. 2020; 181(3):379–381.

4. COVID-19 outbreak among college students after a spring break trip to Mexico - Austin, Texas, March 26-April 5, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(26):830–835. PMID:
32614814.
5. Wilson E, Donovan CV, Campbell M, Chai T, Pittman K, Seña AC, et al. Multiple COVID-19 clusters on a university campus - North Carolina, August 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(39):1416–1418. PMID:
33001871.

6. Chen WL, Song SY, Yap KH. The unintended consequences of the pandemic: the new normal for college students in South Korea and Taiwan. Front Public Health. 2021; 9:598302. PMID:
34046381.

7. Jang S, Lee H. Changes in core competencies among Korean university students due to remote learning during the COVID-19 Pandemic. Int J Environ Res Public Health. 2021; 18(14):7476. PMID:
34299922.

8. Shim TE, Lee SY. College students' experience of emergency remote teaching due to COVID-19. Child Youth Serv Rev. 2020; 119:105578. PMID:
33071405.

9. Jun M, Lee S, Shim T. First-year college student life experiences during COVID-19 in South Korea. Int J Environ Res Public Health. 2021; 18(18):9895. PMID:
34574818.

10. Kim DH, Lee HJ, Lin Y, Kang YJ. Changes in academic performance in the online, integrated system-based curriculum implemented due to the COVID-19 pandemic in a medical school in Korea. J Educ Eval Health Prof. 2021; 18:24. PMID:
34551511.

12. Park M. Infectious disease-related laws: prevention and control measures. Epidemiol Health. 2017; 39:e2017033. PMID:
28774161.

14. Lu H, Weintz C, Pace J, Indana D, Linka K, Kuhl E. Are college campuses superspreaders? A data-driven modeling study. Comput Methods Biomech Biomed Engin. 2021; 24(10):1136–1145. PMID:
33439055.

15. Mangrum D, Niekamp P. JUE insight: college student travel contributed to local COVID-19 spread. J Urban Econ. Forthcoming. 2020; DOI:
10.1080/07448481.2021.1909041.

16. Park Y, Huh IS, Lee J, Kang CR, Cho SI, Ham HJ, et al. Application of testing-tracing-treatment strategy in response to the COVID-19 outbreak in Seoul, Korea. J Korean Med Sci. 2020; 35(45):e396. PMID:
33230987.

17. Aguiar-Oliveira ML, Campos A, R Matos A, Rigotto C, Sotero-Martins A, Teixeira PF, et al. Wastewater-based epidemiology (WBE) and viral detection in polluted surface water: a valuable tool for COVID-19 surveillance-a brief review. Int J Environ Res Public Health. 2020; 17(24):E9251. PMID:
33321987.

18. Betancourt WQ, Schmitz BW, Innes GK, Prasek SM, Pogreba Brown KM, Stark ER, et al. COVID-19 containment on a college campus via wastewater-based epidemiology, targeted clinical testing and an intervention. Sci Total Environ. 2021; 779:146408. PMID:
33743467.

19. Gibas C, Lambirth K, Mittal N, Juel MA, Barua VB, Roppolo Brazell L, et al. Implementing building-level SARS-CoV-2 wastewater surveillance on a university campus. Sci Total Environ. 2021; 782:146749. PMID:
33838367.

SUPPLEMENTARY MATERIAL
Supplementary Fig. 1
Locations of university/college campus participated in the investigation, Seoul Metropolitan Area, 2020–2021.
jkms-36-e302-s001.doc




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download