Abstract
Immune thrombocytopenia (ITP) is an autoimmune condition characterized by platelet destruction through antibody-mediated mechanism. ITP is one of the manifestations of a coronavirus disease, as well as an adverse event occurring after vaccination against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Several cases of ITP have been described after vaccination with two mRNA-based vaccines—BTN162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna)—against SARS-CoV-2. Herein, we report a case of ITP occurring after vaccination with ChAdOx1 adenovirus vector nCoV-19 (AstraZeneca) vaccine in Korea. A 66-year-old woman presented with multiple ecchymoses on both upper and lower extremities and gingival bleeding, appearing 3 days after receiving the first dose of ChAdOx1 nCoV-19. Her laboratory results showed isolated severe thrombocytopenia without evidence of combined coagulopathy. She was diagnosed with ITP and successfully treated with high-dose dexamethasone and intravenous immunoglobulin. Clinical suspicion to identify vaccine-related ITP is important to promptly initiate appropriate treatment.
Graphical Abstract
Immune thrombocytopenia (ITP) is an autoimmune condition characterized by platelet destruction and impaired platelet production through antibody-mediated mechanism which can be triggered by stimuli including infection and vaccination.1 Although ITP can be presented with coronavirus disease 2019 (COVID-19) infection which develops secondary to the disease,2 vaccination against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can also be followed by ITP. Post-vaccination ITP has been observed with other vaccines including measles, mumps, and rubella (MMR) with an estimated incidence of 1 in 40,000 doses.3 Several cases of ITP, regardless of probable association with the vaccination, have been reported following SARS-CoV-2 immunization, mostly in the United Kingdom and the United States.456789 We present a case of ITP occurring after ChAdOx1 nCoV-19 vaccination.
A 66-year-old woman presented with multiple bruises on her extremities and gum bleeding. She was immunized against SARS-CoV-2 with the first dose of ChAdOx1 nCoV-19 vaccine 3 days before the visit. Shortly after the vaccination, she had a febrile sensation with mild myalgia which resolved after taking acetaminophen. Two days after vaccination, she experienced gingival bleeding after toothbrushing. The next day, she noticed an oval-shaped mass on the lateral side of her left thigh and multiple spontaneous bruises on both legs. The lesions were not associated with pain, sense of heat, or limitation of limb movement. She had no prior history of bone marrow disorder or bleeding diathesis, and her platelet counts from 5 and 2 years prior to the admission were 202,000 and 213,000/μL, respectively. She has been taking no medications other than calcium carbonate/cholecalciferol supplement.
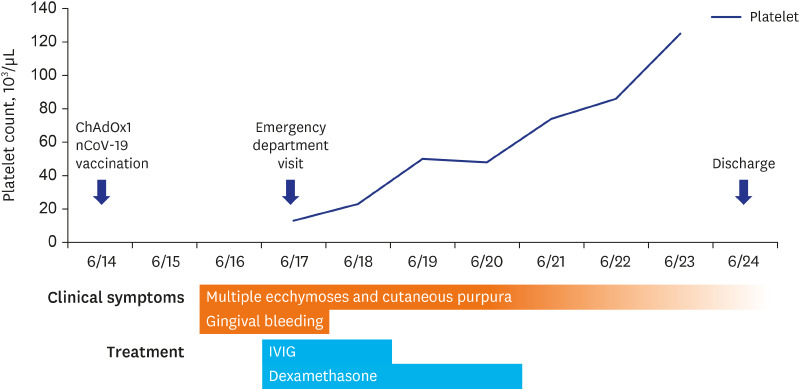
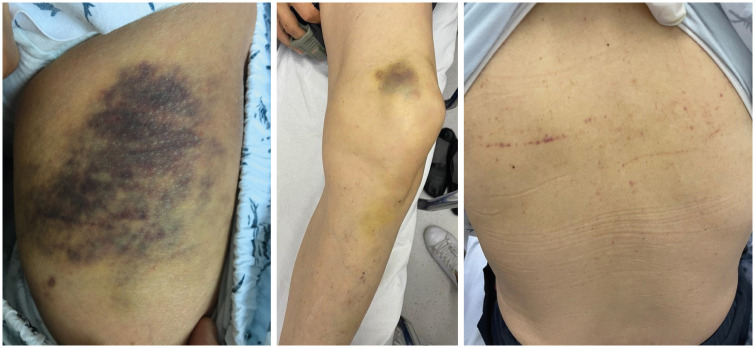
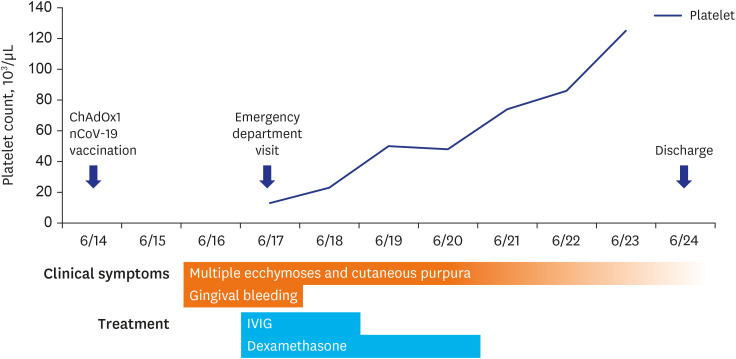
Her vital signs were stable without fever, and she had about 10- and 15-cm-wide ecchymoses on the left knee and left thigh each, and multiple smaller purpuras on other parts of extremities and back (Fig. 1). Gingival bleeding was observed from the maxilla. There were no other remarkable findings except decreased breathing sound on her left lung due to tuberculous destroyed lung. Splenomegaly or hepatomegaly was not noted. The initial laboratory data showed hemoglobin of 14.0 g/dL, white blood cell count of 7,500/μL, and platelet count of 4,000/μL. Peripheral blood smear revealed isolated marked thrombocytopenia without schistocytes. The prothrombin time (11.3 seconds) and activated partial thromboplastin time (29.6 seconds) were not prolonged. D-dimer was lower than the institution's detection limits (< 0.19 μg/mL fibrinogen-equivalent units), and fibrinogen was 312 mg/dL. There were no abnormal findings regarding secondary causes of ITP, in hepatitis B virus surface antigen, anti-hepatitis C virus antibody, human immunodeficiency virus antibody, antinuclear antibody, anti-double stranded DNA, and urea breath test. SARS-CoV-2 reverse transcription polymerase chain reaction test and anti-heparin/platelet factor 4 (PF4) immunoglobulin G showed negative results. Based on her medical history and laboratory findings, she was diagnosed with ITP secondary to vaccination. She was treated with high-dose dexamethasone (40 mg daily for 4 days) and intravenous immunoglobulin (IVIG, 1 g/kg for 2 days) immediately and her platelet counts recovered to over 100,000 platelets/μL 6 days after the commencement of treatment (Fig. 2). Her ecchymoses gradually improved and she discharged without complications.
We introduced a case of de novo ITP following ChAdOx1 nCoV-19 vaccine in Korea. A 66-year-old woman was diagnosed with post-vaccination ITP which occurred 3 days after immunization with the first dose of ChAdOx1 nCoV-19 vaccine. Her platelet count and symptoms gradually improved after high-dose dexamethasone and IVIG. ITP is one of the adverse events of SARS-CoV-2 vaccines. To date, over 200 reports were documented on the Vaccine Adverse Event Reporting System10 as having “immune thrombocytopenia” after SARS-CoV-2 vaccination. Several cases of SARS-CoV-2 vaccine-related ITP within a week of receiving the mRNA vaccines have been reported.45678 Regarding adenovirus vector vaccine, a recent study of a national prospective cohort in Scotland reported ITP development in 1.13 cases per 100,000 doses of ChAdOx1 nCoV-19 vaccines during a 27-day period after vaccination.9 Increased risk of vaccine-related ITP first occurs 7 days post-vaccination, with the highest relative risk during 21–27 days.
Thrombocytopenia rarely occurs following SARS-CoV-2 vaccination.9 Encountering the vaccinated individuals with severe thrombocytopenia, clinicians should consider several causes including ITP and vaccine-induced immune thrombotic thrombocytopenia (VITT). ITP is diagnosed through a process of exclusion, and usually exhibit isolated thrombocytopenia without D-dimer elevation.11 On the contrary, VITT is clinically similar to autoimmune heparin-induced thrombocytopenia and often causes thrombosis and shows lesser degree of thrombocytopenia compared to ITP.12 Positive anti-heparin/PF4 antibody test can help the diagnosis of VITT. The patient in this case showed severe thrombocytopenia of 4,000/μL, negative result for anti-heparin/PF4 IgG, and unelevated D-dimer level, suggesting ITP over VITT.
Vaccines protect the host from the target virus via induction of antibody generation against viral peptides. Autoimmunity can develop due to cross-reactivity of the generated antibodies.13 The epitopes used for induction of the host immune system may mimic the structure of self-peptides, and the antibodies developed after vaccination may cause cross-reactivity directed to self. In post-vaccination ITP, platelets and megakaryocytes can be both targeted by the antibodies produced through stimulation of vaccines such as MMR or SARS-CoV-2 vaccine.113 The interaction leads to opsonization, complement activation or apoptosis of the bound platelets, and antibody-coated platelets are later removed from the spleen.1314 A few cases of vaccine-associated ITP are known to develop autoantibodies against the platelet peptide GPIIb/IIIa similar to primary ITP.15
Post-vaccination ITP is treated as ITP from other causes and usually responsive to IVIG and corticosteroids.15 Similar to the present case, most of the reported cases of SARS-CoV-2 vaccine-related ITP responded to high-dose steroid and IVIG therapy.568 A refractory case of ITP was also reported, with additional rituximab, plasma exchange, and eltrombopag being unsuccessful, but thrombocytopenia finally improved with the administration of romiplostim.4
ITP is one of the rare adverse events induced after SARS-CoV-2 immunization which can lead to a life-threatening hemorrhage.13 The incidence, severity, and treatment of ITP following SARS-CoV-2 vaccination in the absence of VITT are yet to be fully understood. Nevertheless, cases of post-vaccination ITP can be successfully treated with corticosteroids and IVIG like primary or secondary ITP of other causes. Cautious measures are required to identify ITP occurring secondary to SARS-CoV-2 vaccination and appropriate treatment should be initiated without a delay.
References
1. Audia S, Mahévas M, Samson M, Godeau B, Bonnotte B. Pathogenesis of immune thrombocytopenia. Autoimmun Rev. 2017; 16(6):620–632. PMID: 28428120.

2. Bhattacharjee S, Banerjee M. Immune thrombocytopenia secondary to COVID-19: a systematic review. SN Compr Clin Med. Forthcoming. 2020.

3. Saudagar V, Patil S, Goh S, Pothiawala S. Vigilance regarding immune thrombocytopenic purpura after COVID-19 vaccine. Ir J Med Sci. Forthcoming. 2021.

4. Helms JM, Ansteatt KT, Roberts JC, Kamatam S, Foong KS, Labayog JS, et al. Severe, refractory immune thrombocytopenia occurring after SARS-CoV-2 vaccine. J Blood Med. 2021; 12:221–224. PMID: 33854395.

5. David P, Dotan A, Mahroum N, Shoenfeld Y. Immune thrombocytopenic purpura (ITP) triggered by COVID-19 infection and vaccination. Isr Med Assoc J. 2021; 23(6):378–380. PMID: 34155853.
6. Idogun PO, Ward MC, Teklie Y, Wiese-Rometsch W, Baker J. Newly diagnosed idiopathic thrombocytopenia post COVID-19 vaccine administration. Cureus. 2021; 13(5):e14853. PMID: 34113494.

7. Malayala SV, Mohan G, Vasireddy D, Atluri P. Purpuric rash and thrombocytopenia after the mRNA-1273 (Moderna) COVID-19 vaccine. Cureus. 2021; 13(3):e14099. PMID: 33786251.

8. Fueyo-Rodriguez O, Valente-Acosta B, Jimenez-Soto R, Neme-Yunes Y, Inclán-Alarcón SI, Trejo-Gonzalez R, et al. Secondary immune thrombocytopenia supposedly attributable to COVID-19 vaccination. BMJ Case Rep. 2021; 14(5):e242220.

9. Simpson CR, Shi T, Vasileiou E, Katikireddi SV, Kerr S, Moore E, et al. First-dose ChAdOx1 and BNT162b2 COVID-19 vaccines and thrombocytopenic, thromboembolic and hemorrhagic events in Scotland. Nat Med. 2021; 27(7):1290–1297. PMID: 34108714.

10. Chen RT, Rastogi SC, Mullen JR, Hayes SW, Cochi SL, Donlon JA, et al. The vaccine adverse event reporting system (VAERS). Vaccine. 1994; 12(6):542–550. PMID: 8036829.

11. Iraqi M, Perdomo J, Yan F, Choi PY, Chong BH. Immune thrombocytopenia: antiplatelet autoantibodies inhibit proplatelet formation by megakaryocytes and impair platelet production in vitro. Haematologica. 2015; 100(5):623–632. PMID: 25682608.

12. Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med. 2021; 384(22):2092–2101. PMID: 33835769.

13. Perricone C, Ceccarelli F, Nesher G, Borella E, Odeh Q, Conti F, et al. Immune thrombocytopenic purpura (ITP) associated with vaccinations: a review of reported cases. Immunol Res. 2014; 60(2-3):226–235. PMID: 25427992.

14. Cines DB, Bussel JB, Liebman HA, Luning Prak ET. The ITP syndrome: pathogenic and clinical diversity. Blood. 2009; 113(26):6511–6521. PMID: 19395674.

15. Cines DB, Blanchette VS. Immune thrombocytopenic purpura. N Engl J Med. 2002; 346(13):995–1008. PMID: 11919310.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download