1. Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021; 143:e254–e743. PMID:
33501848.
2. Berry JD, Dyer A, Cai X, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012; 366:321–329. PMID:
22276822.

3. Khot UN, Khot MB, Bajzer CT, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003; 290:898–904. PMID:
12928466.

4. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002; 360:1903–1913. PMID:
12493255.
5. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016; 387:957–967. PMID:
26724178.

6. SPRINT Research Group. Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103–2116. PMID:
26551272.

7. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39:3021–3104. PMID:
30165516.
8. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018; 71:2199–2269. PMID:
29146533.
9. Safar ME, Levy BI, Struijker-Boudier H. Current perspectives on arterial stiffness and pulse pressure in hypertension and cardiovascular diseases. Circulation. 2003; 107:2864–2869. PMID:
12796414.

10. Weber T, Chirinos JA. Pulsatile arterial haemodynamics in heart failure. Eur Heart J. 2018; 39:3847–3854. PMID:
29947746.

11. Zhao L, Song Y, Dong P, Li Z, Yang X, Wang S. Brachial pulse pressure and cardiovascular or all-cause mortality in the general population: a meta-analysis of prospective observational studies. J Clin Hypertens (Greenwich). 2014; 16:678–685. PMID:
25052820.

12. Chae CU, Pfeffer MA, Glynn RJ, Mitchell GF, Taylor JO, Hennekens CH. Increased pulse pressure and risk of heart failure in the elderly. JAMA. 1999; 281:634–639. PMID:
10029125.

13. Domanski MJ, Davis BR, Pfeffer MA, Kastantin M, Mitchell GF. Isolated systolic hypertension : prognostic information provided by pulse pressure. Hypertension. 1999; 34:375–380. PMID:
10489379.
14. Mitchell GF, Moyé LA, Braunwald E, et al. Sphygmomanometrically determined pulse pressure is a powerful independent predictor of recurrent events after myocardial infarction in patients with impaired left ventricular function. SAVE investigators. Survival and Ventricular Enlargement. Circulation. 1997; 96:4254–4260. PMID:
9416890.
15. Mitchell GF, Vita JA, Larson MG, et al. Cross-sectional relations of peripheral microvascular function, cardiovascular disease risk factors, and aortic stiffness: the Framingham Heart Study. Circulation. 2005; 112:3722–3728. PMID:
16330686.
16. Rosenbaum D, Giral P, Chapman J, et al. Radial augmentation index is a surrogate marker of atherosclerotic burden in a primary prevention cohort. Atherosclerosis. 2013; 231:436–441. PMID:
24267263.

17. Nürnberger J, Keflioglu-Scheiber A, Opazo Saez AM, Wenzel RR, Philipp T, Schäfers RF. Augmentation index is associated with cardiovascular risk. J Hypertens. 2002; 20:2407–2414. PMID:
12473865.

18. Ohkuma T, Ninomiya T, Tomiyama H, et al. Brachial-ankle pulse wave velocity and the risk prediction of cardiovascular disease: an individual participant data meta-analysis. Hypertension. 2017; 69:1045–1052. PMID:
28438905.
19. Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010; 55:1318–1327. PMID:
20338492.
20. Chirinos JA, Segers P, Hughes T, Townsend R. Large-artery stiffness in health and disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019; 74:1237–1263. PMID:
31466622.
21. Dart AM, Kingwell BA. Pulse pressure--a review of mechanisms and clinical relevance. J Am Coll Cardiol. 2001; 37:975–984. PMID:
11263624.

22. McEniery CM, Cockcroft JR, Roman MJ, Franklin SS, Wilkinson IB. Central blood pressure: current evidence and clinical importance. Eur Heart J. 2014; 35:1719–1725. PMID:
24459197.

23. Safar ME. Pulse pressure, arterial stiffness and wave reflections (augmentation index) as cardiovascular risk factors in hypertension. Ther Adv Cardiovasc Dis. 2008; 2:13–24. PMID:
19124404.
24. Agabiti-Rosei E, Mancia G, O’Rourke MF, et al. Central blood pressure measurements and antihypertensive therapy: a consensus document. Hypertension. 2007; 50:154–160. PMID:
17562972.
25. O’Rourke MF, Nichols WW. Aortic diameter, aortic stiffness, and wave reflection increase with age and isolated systolic hypertension. Hypertension. 2005; 45:652–658. PMID:
15699456.

26. Van Bortel LM, Balkestein EJ, van der Heijden-Spek JJ, et al. Non-invasive assessment of local arterial pulse pressure: comparison of applanation tonometry and echo-tracking. J Hypertens. 2001; 19:1037–1044. PMID:
11403351.

27. Chen CH, Nevo E, Fetics B, et al. Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure. Validation of generalized transfer function. Circulation. 1997; 95:1827–1836. PMID:
9107170.
28. Sharman JE, Lim R, Qasem AM, et al. Validation of a generalized transfer function to noninvasively derive central blood pressure during exercise. Hypertension. 2006; 47:1203–1208. PMID:
16651459.

29. Mitchell GF, Parise H, Benjamin EJ, et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham Heart Study. Hypertension. 2004; 43:1239–1245. PMID:
15123572.
30. McEniery CM, Yasmin , Hall IR, et al. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol. 2005; 46:1753–1760. PMID:
16256881.
31. Shimizu M, Kario K. Role of the augmentation index in hypertension. Ther Adv Cardiovasc Dis. 2008; 2:25–35. PMID:
19124405.
32. Kim HL, Koo BK, Joo SK, Kim W. Association of arterial stiffness with the histological severity of nonalcoholic fatty liver disease. Hepatol Int. 2020; 14:1048–1056. PMID:
33269420.

33. Stamatelopoulos KS, Kalpakos D, Protogerou AD, et al. The combined effect of augmentation index and carotid intima-media thickness on cardiovascular risk in young and middle-aged men without cardiovascular disease. J Hum Hypertens. 2006; 20:273–279. PMID:
16397513.

34. Weber T, Auer J, O’rourke MF, et al. Increased arterial wave reflections predict severe cardiovascular events in patients undergoing percutaneous coronary interventions. Eur Heart J. 2005; 26:2657–2663. PMID:
16183688.

35. Weber T, Auer J, Lamm G, O’Rourke MF, Eber B. Arterial stiffness, central blood pressures, and wave reflections in cardiomyopathy-implications for risk stratification. J Card Fail. 2007; 13:353–359. PMID:
17602981.

36. Hughes AD, Park C, Davies J, et al. Limitations of augmentation index in the assessment of wave reflection in normotensive healthy individuals. PLoS One. 2013; 8:e59371. PMID:
23544061.

37. Cavalcante JL, Lima JA, Redheuil A, Al-Mallah MH. Aortic stiffness: current understanding and future directions. J Am Coll Cardiol. 2011; 57:1511–1522. PMID:
21453829.
38. Safar ME. Arterial aging--hemodynamic changes and therapeutic options. Nat Rev Cardiol. 2010; 7:442–449. PMID:
20657613.

39. Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006; 27:2588–2605. PMID:
17000623.

40. Munakata M. Brachial-ankle pulse wave velocity in the measurement of arterial stiffness: recent evidence and clinical applications. Curr Hypertens Rev. 2014; 10:49–57. PMID:
25392144.

41. Kim HL, Kim SH. Pulse wave velocity in atherosclerosis. Front Cardiovasc Med. 2019; 6:41. PMID:
31024934.

42. Reference Values for Arterial Stiffness' Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur Heart J. 2010; 31:2338–2350. PMID:
20530030.
43. Lee HY, Oh BH. Aging and arterial stiffness. Circ J. 2010; 74:2257–2262. PMID:
20962429.

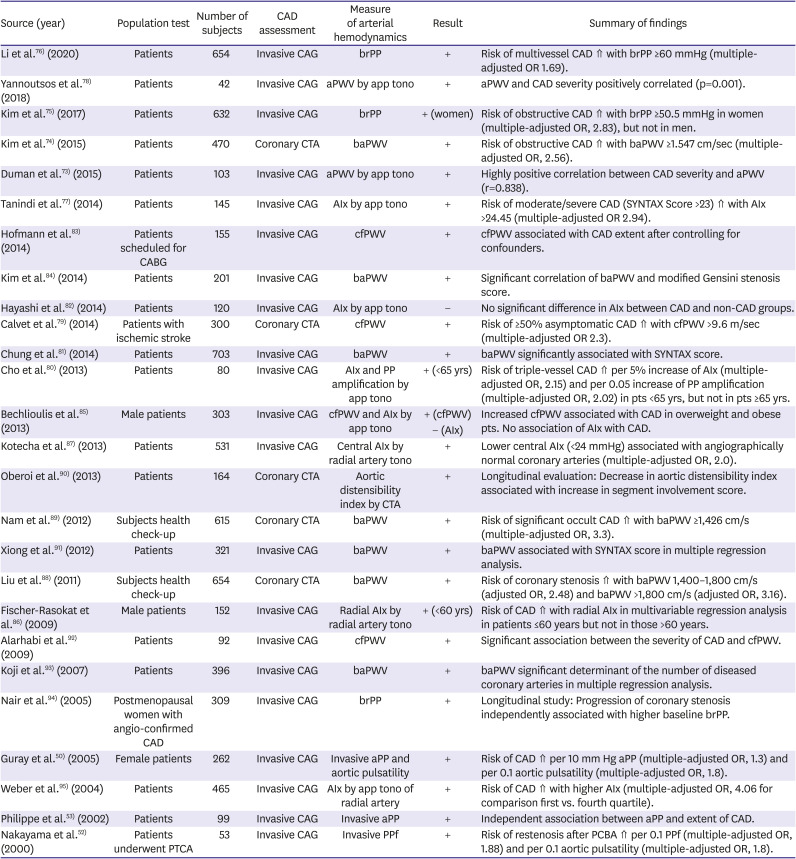
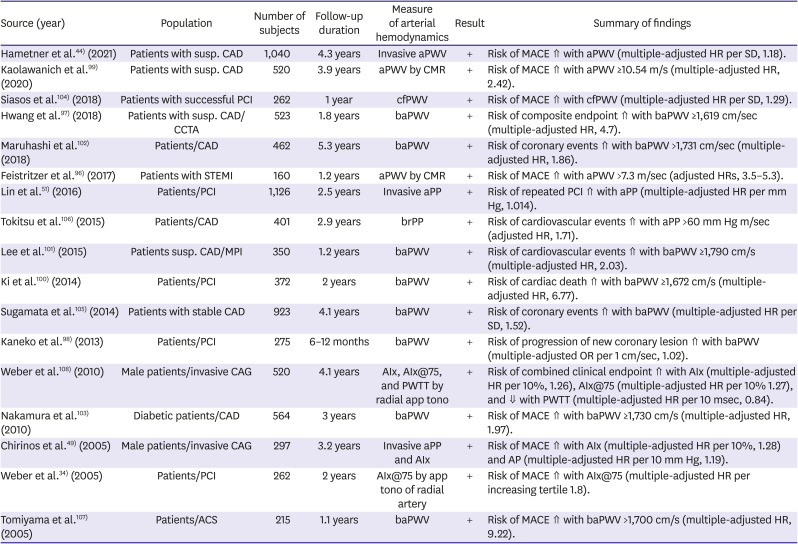
44. Hametner B, Wassertheurer S, Mayer CC, Danninger K, Binder RK, Weber T. Aortic pulse wave velocity predicts cardiovascular events and mortality in patients undergoing coronary angiography: a comparison of invasive measurements and noninvasive estimates. Hypertension. 2021; 77:571–581. PMID:
33390046.
45. Kim HL, Seo JB, Chung WY, Kim SH, Kim MA, Zo JH. Association between invasively measured central aortic pressure and left ventricular diastolic function in patients undergoing coronary angiography. Am J Hypertens. 2015; 28:393–400. PMID:
25125636.

46. Weber T, Wassertheurer S, Hametner B, Parragh S, Eber B. Noninvasive methods to assess pulse wave velocity: comparison with the invasive gold standard and relationship with organ damage. J Hypertens. 2015; 33:1023–1031. PMID:
25668350.
47. Kang J, Kim HL, Lim WH, et al. Relationship between brachial-ankle pulse wave velocity and invasively measured aortic pulse pressure. J Clin Hypertens (Greenwich). 2018; 20:462–468. PMID:
29370481.

48. Yamashina A, Tomiyama H, Takeda K, et al. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res. 2002; 25:359–364. PMID:
12135313.

49. Chirinos JA, Zambrano JP, Chakko S, et al. Aortic pressure augmentation predicts adverse cardiovascular events in patients with established coronary artery disease. Hypertension. 2005; 45:980–985. PMID:
15837821.

50. Guray Y, Guray U, Altay H, et al. Aortic pulse pressure and aortic pulsatility are associated with angiographic coronary artery disease in women. Blood Press. 2005; 14:293–297. PMID:
16257875.

51. Lin MJ, Chen CY, Lin HD, Lin CS, Wu HP. Prognostic significance of central pulse pressure for mortality in patients with coronary artery disease receiving repeated percutaneous coronary intervention. Medicine (Baltimore). 2016; 95:e3218. PMID:
27043689.

52. Nakayama Y, Tsumura K, Yamashita N, Yoshimaru K, Hayashi T. Pulsatility of ascending aortic pressure waveform is a powerful predictor of restenosis after percutaneous transluminal coronary angioplasty. Circulation. 2000; 101:470–472. PMID:
10662741.

53. Philippe F, Chemaly E, Blacher J, et al. Aortic pulse pressure and extent of coronary artery disease in percutaneous transluminal coronary angioplasty candidates. Am J Hypertens. 2002; 15:672–677. PMID:
12160188.

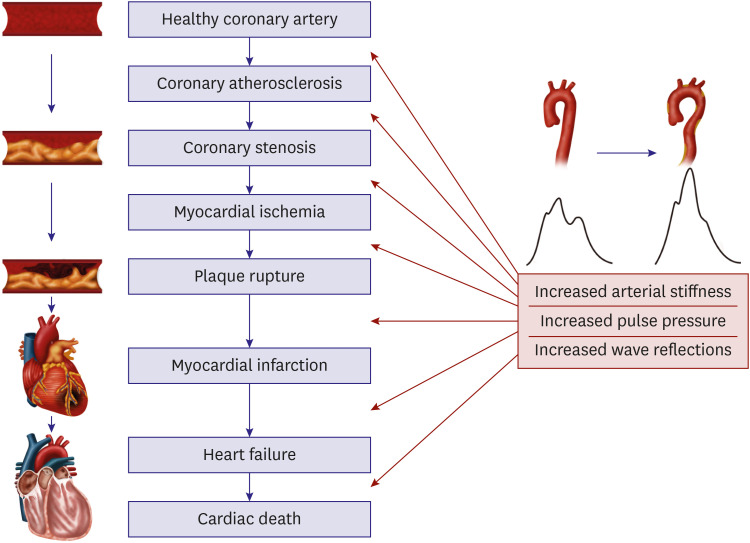
54. Al-Mashhadi RH, Al-Mashhadi AL, Nasr ZP, et al. Local pressure drives low-density lipoprotein accumulation and coronary atherosclerosis in hypertensive minipigs. J Am Coll Cardiol. 2021; 77:575–589. PMID:
33538256.

55. Safar ME, Blacher J, Jankowski P. Arterial stiffness, pulse pressure, and cardiovascular disease-is it possible to break the vicious circle? Atherosclerosis. 2011; 218:263–271. PMID:
21621778.

56. Kiefer CR, McKenney JB, Trainor JF, Snyder LM. Pulse-pressure-driven neutral lipid accumulation and correlative proinflammatory markers of accelerated atherogenesis. Atherosclerosis. 2005; 183:17–24. PMID:
16216588.
57. Sakamoto H, Aikawa M, Hill CC, et al. Biomechanical strain induces class a scavenger receptor expression in human monocyte/macrophages and THP-1 cells: a potential mechanism of increased atherosclerosis in hypertension. Circulation. 2001; 104:109–114. PMID:
11435347.
58. Lee RT, Schoen FJ, Loree HM, Lark MW, Libby P. Circumferential stress and matrix metalloproteinase 1 in human coronary atherosclerosis. Implications for plaque rupture. Arterioscler Thromb Vasc Biol. 1996; 16:1070–1073. PMID:
8696948.
59. Gould KL, Lipscomb K, Hamilton GW. Physiologic basis for assessing critical coronary stenosis. Instantaneous flow response and regional distribution during coronary hyperemia as measures of coronary flow reserve. Am J Cardiol. 1974; 33:87–94. PMID:
4808557.
60. Pijls NH, van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. 1993; 87:1354–1367. PMID:
8462157.

61. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020; 41:407–477. PMID:
31504439.
62. O’Rourke MF, Hashimoto J. Mechanical factors in arterial aging: a clinical perspective. J Am Coll Cardiol. 2007; 50:1–13. PMID:
17601538.
63. Hoffman JI, Buckberg GD. The myocardial oxygen supply:demand index revisited. J Am Heart Assoc. 2014; 3:e000285. PMID:
24449802.

64. Watanabe H, Ohtsuka S, Kakihana M, Sugishita Y. Decreased aortic compliance aggravates subendocardial ischaemia in dogs with stenosed coronary artery. Cardiovasc Res. 1992; 26:1212–1218. PMID:
1288867.

65. Leung MC, Meredith IT, Cameron JD. Aortic stiffness affects the coronary blood flow response to percutaneous coronary intervention. Am J Physiol Heart Circ Physiol. 2006; 290:H624–H630. PMID:
16143654.

66. Ikonomidis I, Lekakis J, Papadopoulos C, et al. Incremental value of pulse wave velocity in the determination of coronary microcirculatory dysfunction in never-treated patients with essential hypertension. Am J Hypertens. 2008; 21:806–813. PMID:
18497732.

67. Fukuda D, Yoshiyama M, Shimada K, et al. Relation between aortic stiffness and coronary flow reserve in patients with coronary artery disease. Heart. 2006; 92:759–762. PMID:
16216858.

68. Saito M, Okayama H, Nishimura K, et al. Possible link between large artery stiffness and coronary flow velocity reserve. Heart. 2008; 94:e20. PMID:
17947361.

69. Kingwell BA, Waddell TK, Medley TL, Cameron JD, Dart AM. Large artery stiffness predicts ischemic threshold in patients with coronary artery disease. J Am Coll Cardiol. 2002; 40:773–779. PMID:
12204510.

70. Weber T, Auer J, O'Rourke MF, Punzengruber C, Kvas E, Eber B. Prolonged mechanical systole and increased arterial wave reflections in diastolic dysfunction. Heart. 2006; 92:1616–1622. PMID:
16709696.

71. Weber T. The role of arterial stiffness and central hemodynamics in heart failure. Int J Heart Fail. 2020; 2:209–230.

72. Weber T, Wassertheurer S, O'Rourke MF, et al. Pulsatile hemodynamics in patients with exertional dyspnea: potentially of value in the diagnostic evaluation of suspected heart failure with preserved ejection fraction. J Am Coll Cardiol. 2013; 61:1874–1883. PMID:
23500307.
73. Duman OO, Goldeli O, Gursul E, Baris N, Ozpelit E, Simsek MA. The value of aortic pulse wave velocity in predicting coronary artery disease diagnosis and severity. Acta Cardiol. 2015; 70:315–322. PMID:
26226705.
74. Kim HL, Jin KN, Seo JB, et al. The association of brachial-ankle pulse wave velocity with coronary artery disease evaluated by coronary computed tomography angiography. PLoS One. 2015; 10:e0123164. PMID:
25875036.

75. Kim HL, Kim MA, Shim WJ, et al. Sex difference in the association between brachial pulse pressure and coronary artery disease: the Korean Women's Chest Pain Registry (KoROSE). J Clin Hypertens (Greenwich). 2017; 19:38–44. PMID:
27364854.

76. Li J, Peng Y, Ji K. Brachial pulse pressure is associated with the presence and extent of coronary artery disease in stable angina patients: a cross-sectional study. BMC Cardiovasc Disord. 2020; 20:143. PMID:
32197578.

77. Tanindi A, Erkan AF, Alhan A, Töre HF. Central pulse pressure amplification is associated with more extensive and severe coronary artery disease. Scand Cardiovasc J. 2014; 48:167–175. PMID:
24568590.

78. Yannoutsos A, Ahouah M, Dreyfuss Tubiana C, Topouchian J, Safar ME, Blacher J. Aortic stiffness improves the prediction of both diagnosis and severity of coronary artery disease. Hypertens Res. 2018; 41:118–125. PMID:
29118329.

79. Calvet D, Touzé E, Laurent S, et al. Aortic stiffness measurement improves the prediction of asymptomatic coronary artery disease in stroke/transient ischemic attack patients. Int J Stroke. 2014; 9:291–296. PMID:
23855884.

80. Cho SW, Kim BK, Kim JH, et al. Non-invasively measured aortic wave reflection and pulse pressure amplification are related to the severity of coronary artery disease. J Cardiol. 2013; 62:131–137. PMID:
23731925.

81. Chung CM, Yang TY, Lin YS, et al. Relation of arterial stiffness assessed by brachial-ankle pulse wave velocity to complexity of coronary artery disease. Am J Med Sci. 2014; 348:294–299. PMID:
24845468.

82. Hayashi S, Yamada H, Bando M, et al. Augmentation index does not reflect risk of coronary artery disease in elderly patients. Circ J. 2014; 78:1176–1182. PMID:
24562676.

83. Hofmann B, Riemer M, Erbs C, et al. Carotid to femoral pulse wave velocity reflects the extent of coronary artery disease. J Clin Hypertens (Greenwich). 2014; 16:629–633. PMID:
25080855.

84. Kim JH, Rhee MY, Kim YS, et al. Brachial-ankle pulse wave velocity for the prediction of the presence and severity of coronary artery disease. Clin Exp Hypertens. 2014; 36:404–409. PMID:
24164335.

85. Bechlioulis A, Vakalis K, Naka KK, et al. Increased aortic pulse wave velocity is associated with the presence of angiographic coronary artery disease in overweight and obese patients. Am J Hypertens. 2013; 26:265–270. PMID:
23382412.

86. Fischer-Rasokat U, Brenck F, Zeiher AM, Spyridopoulos I. Radial augmentation index unmasks premature coronary artery disease in younger males. Blood Press Monit. 2009; 14:59–67. PMID:
19295416.

87. Kotecha D, New G, Collins P, et al. Radial artery pulse wave analysis for non-invasive assessment of coronary artery disease. Int J Cardiol. 2013; 167:917–924. PMID:
22483418.

88. Liu CS, Li CI, Shih CM, et al. Arterial stiffness measured as pulse wave velocity is highly correlated with coronary atherosclerosis in asymptomatic patients. J Atheroscler Thromb. 2011; 18:652–658. PMID:
21467807.

89. Nam HJ, Jung IH, Kim J, et al. Association between brachial-ankle pulse wave velocity and occult coronary artery disease detected by multi-detector computed tomography. Int J Cardiol. 2012; 157:227–232. PMID:
21315465.

90. Oberoi S, Schoepf UJ, Meyer M, et al. Progression of arterial stiffness and coronary atherosclerosis: longitudinal evaluation by cardiac CT. AJR Am J Roentgenol. 2013; 200:798–804. PMID:
23521451.

91. Xiong Z, Zhu C, Zheng Z, et al. Relationship between arterial stiffness assessed by brachial-ankle pulse wave velocity and coronary artery disease severity assessed by the SYNTAX score. J Atheroscler Thromb. 2012; 19:970–976. PMID:
22785141.

92. Alarhabi AY, Mohamed MS, Ibrahim S, Hun TM, Musa KI, Yusof Z. Pulse wave velocity as a marker of severity of coronary artery disease. J Clin Hypertens (Greenwich). 2009; 11:17–21. PMID:
19125854.

93. Koji Y, Tomiyama H, Yamada J, et al. Relationship between arterial stiffness and the risk of coronary artery disease in subjects with and without metabolic syndrome. Hypertens Res. 2007; 30:243–247. PMID:
17510506.

94. Nair GV, Waters D, Rogers W, Kowalchuk GJ, Stuckey TD, Herrington DM. Pulse pressure and coronary atherosclerosis progression in postmenopausal women. Hypertension. 2005; 45:53–57. PMID:
15545509.

95. Weber T, Auer J, O’Rourke MF, et al. Arterial stiffness, wave reflections, and the risk of coronary artery disease. Circulation. 2004; 109:184–189. PMID:
14662706.

96. Feistritzer HJ, Klug G, Reinstadler SJ, et al. Prognostic value of aortic stiffness in patients after ST-elevation myocardial infarction. J Am Heart Assoc. 2017; 6:6.
97. Hwang IC, Jin KN, Kim HL, et al. Additional prognostic value of brachial-ankle pulse wave velocity to coronary computed tomography angiography in patients with suspected coronary artery disease. Atherosclerosis. 2018; 268:127–137. PMID:
29216483.

98. Kaneko H, Yajima J, Oikawa Y, et al. Role of arterial stiffness and impaired renal function in the progression of new coronary lesions after percutaneous coronary intervention. Cardiovasc Interv Ther. 2013; 28:56–62. PMID:
23011752.

99. Kaolawanich Y, Boonyasirinant T. Incremental prognostic value of aortic stiffness in addition to myocardial ischemia by cardiac magnetic resonance imaging. BMC Cardiovasc Disord. 2020; 20:287. PMID:
32527291.

100. Ki YJ, Choi DH, Lee YM, Lim L, Song H, Koh YY. Predictive value of brachial-ankle pulse wave velocity for long-term clinical outcomes after percutaneous coronary intervention in a Korean cohort. Int J Cardiol. 2014; 175:554–559. PMID:
25015023.

101. Lee HS, Kim HL, Kim H, et al. Incremental prognostic value of brachial-ankle pulse wave velocity to single-photon emission computed tomography in patients with suspected coronary artery disease. J Atheroscler Thromb. 2015; 22:1040–1050. PMID:
26235347.

102. Maruhashi T, Soga J, Fujimura N, et al. Endothelial dysfunction, increased arterial stiffness, and cardiovascular risk prediction in patients with coronary artery disease: FMD-J (Flow-Mediated Dilation Japan) Study A. J Am Heart Assoc. 2018; 7:e008588. PMID:
30005558.

103. Nakamura M, Yamashita T, Yajima J, et al. Brachial-ankle pulse wave velocity as a risk stratification index for the short-term prognosis of type 2 diabetic patients with coronary artery disease. Hypertens Res. 2010; 33:1018–1024. PMID:
20703233.

104. Siasos G, Oikonomou E, Maniatis K, et al. Prognostic significance of arterial stiffness and osteoprotegerin in patients with stable coronary artery disease. Eur J Clin Invest. 2018; 48:e12890.

105. Sugamata W, Nakamura T, Uematsu M, et al. Combined assessment of flow-mediated dilation of the brachial artery and brachial-ankle pulse wave velocity improves the prediction of future coronary events in patients with chronic coronary artery disease. J Cardiol. 2014; 64:179–184. PMID:
24556367.
106. Tokitsu T, Yamamoto E, Hirata Y, et al. Clinical significance of pulse pressure in patients with coronary artery disease. Int J Cardiol. 2015; 190:299–301. PMID:
25935616.

107. Tomiyama H, Koji Y, Yambe M, et al. Brachial -- ankle pulse wave velocity is a simple and independent predictor of prognosis in patients with acute coronary syndrome. Circ J. 2005; 69:815–822. PMID:
15988107.

108. Weber T, O’Rourke MF, Lassnig E, et al. Pulse waveform characteristics predict cardiovascular events and mortality in patients undergoing coronary angiography. J Hypertens. 2010; 28:797–805. PMID:
20164805.

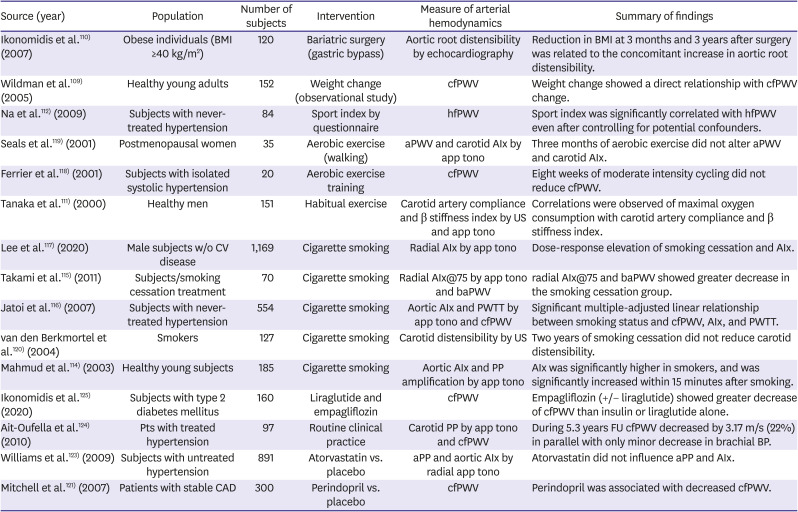
109. Wildman RP, Farhat GN, Patel AS, et al. Weight change is associated with change in arterial stiffness among healthy young adults. Hypertension. 2005; 45:187–192. PMID:
15596570.

110. Ikonomidis I, Mazarakis A, Papadopoulos C, et al. Weight loss after bariatric surgery improves aortic elastic properties and left ventricular function in individuals with morbid obesity: a 3-year follow-up study. J Hypertens. 2007; 25:439–447. PMID:
17211252.

111. Tanaka H, Dinenno FA, Monahan KD, Clevenger CM, DeSouza CA, Seals DR. Aging, habitual exercise, and dynamic arterial compliance. Circulation. 2000; 102:1270–1275. PMID:
10982542.

112. Na SH, Kim YS, Bae JH, et al. Effects of physical activity and aerobic exercise capacity on aortic stiffness in patients with untreated hypertension. Korean Circ J. 2009; 39:52–56.

113. Oliveira NL, Ribeiro F, Alves AJ, Campos L, Oliveira J. The effects of exercise training on arterial stiffness in coronary artery disease patients: a state-of-the-art review. Clin Physiol Funct Imaging. 2014; 34:254–262. PMID:
24138480.

114. Mahmud A, Feely J. Effect of smoking on arterial stiffness and pulse pressure amplification. Hypertension. 2003; 41:183–187. PMID:
12511550.

115. Takami T, Saito Y. Effects of smoking cessation on central blood pressure and arterial stiffness. Vasc Health Risk Manag. 2011; 7:633–638. PMID:
22102787.

116. Jatoi NA, Jerrard-Dunne P, Feely J, Mahmud A. Impact of smoking and smoking cessation on arterial stiffness and aortic wave reflection in hypertension. Hypertension. 2007; 49:981–985. PMID:
17372029.

117. Lee GB, Shim JS, Kim HC. Dose-response association between smoking cessation and arterial stiffness: the Cardiovascular and Metabolic Diseases Etiology Research Center (CMERC) cohort. Korean Circ J. 2020; 50:361–369. PMID:
31960641.

118. Ferrier KE, Waddell TK, Gatzka CD, Cameron JD, Dart AM, Kingwell BA. Aerobic exercise training does not modify large-artery compliance in isolated systolic hypertension. Hypertension. 2001; 38:222–226. PMID:
11509480.

119. Seals DR, Tanaka H, Clevenger CM, et al. Blood pressure reductions with exercise and sodium restriction in postmenopausal women with elevated systolic pressure: role of arterial stiffness. J Am Coll Cardiol. 2001; 38:506–513. PMID:
11499745.

120. van den Berkmortel FW, Wollersheim H, van Langen H, Smilde TJ, den Arend J, Thien T. Two years of smoking cessation does not reduce arterial wall thickness and stiffness. Neth J Med. 2004; 62:235–241. PMID:
15554598.
121. Mitchell GF, Dunlap ME, Warnica W, et al. Long-term trandolapril treatment is associated with reduced aortic stiffness: the prevention of events with angiotensin-converting enzyme inhibition hemodynamic substudy. Hypertension. 2007; 49:1271–1277. PMID:
17452505.
122. Asmar R. Effect of antihypertensive agents on arterial stiffness as evaluated by pulse wave velocity: clinical implications. Am J Cardiovasc Drugs. 2001; 1:387–397. PMID:
14728020.
123. Williams B, Lacy PS, Cruickshank JK, et al. Impact of statin therapy on central aortic pressures and hemodynamics: principal results of the Conduit Artery Function Evaluation-Lipid-Lowering Arm (CAFE-LLA) Study. Circulation. 2009; 119:53–61. PMID:
19103995.
124. Ait-Oufella H, Collin C, Bozec E, et al. Long-term reduction in aortic stiffness: a 5.3-year follow-up in routine clinical practice. J Hypertens. 2010; 28:2336–2341. PMID:
20683338.

125. Ikonomidis I, Pavlidis G, Thymis J, et al. Effects of glucagon-like peptide-1 receptor agonists, sodium-glucose cotransporter-2 inhibitors, and their combination on endothelial glycocalyx, arterial function, and myocardial work index in patients with type 2 diabetes mellitus after 12-month treatment. J Am Heart Assoc. 2020; 9:e015716. PMID:
32326806.

126. Batzias K, Antonopoulos AS, Oikonomou E, et al. Effects of newer antidiabetic drugs on endothelial function and arterial stiffness: a systematic review and meta-analysis. J Diabetes Res. 2018; 2018:1232583. PMID:
30622967.

127. Kato ET, Kimura T. Sodium-glucose co-transporters-2 inhibitors and heart failure: state of the art review and future potentials. Int J Heart Fail. 2020; 2:12–22.

128. Lin X, Chen G, Qi J, Chen X, Zhao J, Lin Q. Effect of continuous positive airway pressure on arterial stiffness in patients with obstructive sleep apnea and hypertension: a meta-analysis. Eur Arch Otorhinolaryngol. 2016; 273:4081–4088. PMID:
26861547.

129. Stary HC. Macrophages, macrophage foam cells, and eccentric intimal thickening in the coronary arteries of young children. Atherosclerosis. 1987; 64:91–108. PMID:
3606726.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download