This article has been
cited by other articles in ScienceCentral.
Abstract
A nosocomial outbreak of severe acute respiratory syndrome-coronavirus-2 occurred in two general wards. One outbreak had pre-symptomatic transmission and was linked epidemiologically with an index case. The other outbreak was associated with early detection failure in a crowded room. Notably, adherence to appropriate mask wearing was not confirmed in the hospital outbreak. Confirmed cases were moved into isolation rooms, and contacts were quarantined. Quarantined cases were tested regularly and facilitated early termination of the hospital outbreak.
Go to :

Graphical Abstract
Go to :

Keywords: Nosocomial Outbreak, SARS-CoV-2
A coronavirus disease 2019 (COVID-19) outbreak in a hospital setting could lead to fatal outcomes. Further, the size and duration of hospital outbreaks could be affected by variations, such as super-spreading events, timing of interventions implemented, and improved infection prevention and control measures.
1 Asymptomatic and pre-symptomatic transmission of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) present challenges for preventing transmission.
23 Herein, we report a case of simultaneous hospital outbreaks with different patterns of occurrence in two general wards.
On November 18, 2020, a nurse (index case) acutely developed fever and was diagnosed with COVID-19. She worked in a general ward (denoted as the A ward). She had worked for about 18 hours without symptoms during the expected infectious period. Close contact was defined using the COVID-19 guideline of the Korea Disease Control and Prevention Agency
4: 1) anyone with exposure > 15 minutes within 1 meter of a person with confirmed COVID-19, 2) healthcare personnel who had unprotected direct contact with a person with confirmed COVID-19, or 3) any patient hospitalized in the same room or sharing the same bathroom as a person with confirmed COVID-19. Contact tracing was performed through interview with confirmed persons, medical record review, and review of CCTV recording.
Contact tracing evaluation revealed that she had 31 close contacts, including assigned patients, their guardians, and healthcare personnel. They were all tested for SARS-CoV-2. In our hospital, polymerase chain reaction (PCR) test was used to diagnose SARS-CoV-2 infection. PCR testing was performed using STANDARD™ M nCoV Real-Time Detection kit (SD Biosensor, Suwon, Korea). Among them, four individuals tested positive. They were all asymptomatic and patients of the index case. The remaining hospitalized patients and their guardians in the A ward were considered close contacts, and were tested for SARS-CoV-2 as soon as possible. As a result, 3 individuals also were positive, 1 patient and 2 guardians, and all of whom had been staying in the same room (three-person room). The patient was not assigned to the index case, but it was determined that the index case had inserted a peripheral venous catheter into the patient during a work shift. On the 2nd day of the outbreak investigation (November 20, 2020) in the A ward, 2 patients who were staying in another general ward (B ward) tested positive for SARS-CoV-2. They had stayed in the same room (5-person room, noted as the B1 room) and were confirmed to have COVID-19 during evaluation due to a symptomatic fever. All patients, guardians, and healthcare workers in B ward were temporarily restricted from moving outside B ward and were tested for SARS-CoV-2. As a result, 4 individuals were confirmed to be positive, 2 healthcare personnel, 1 patient, and 1 guardian; all of whom were epidemiologically associated with the 2 confirmed positive patients in the B ward.
Management of Confirmed Cases and Close Contacts
The confirmed cases moved to isolation rooms in our hospital or transferred to other hospitals for isolation. The close contacts quarantined at home or in our hospital. In the hospital, a maximum of 2 persons, either the patient alone or with a guardian, were quarantined in separate rooms. The quarantined persons were tested for SARS-CoV-2 when symptoms occurred or at regular intervals (every 2 or 3 days) until quarantine restrictions were lifted.
Go to :

Confirmed Cases Identified during the Quarantine Period
A ward
Three healthcare personnel (nurses) and 1 individual who quarantined at home developed symptoms of COVID-19 and were positive for SARS-CoV-2. Two asymptomatic cases that quarantined in the hospital were confirmed to be positive based on the first regular tests. During the outbreak in the A ward, 72 close contacts were notified, and 13 confirmed cases occurred. Thirteen confirmed cases were epidemiologically related to the index case based on contact tracing.
B ward
Three asymptomatic cases that quarantined in the hospital were confirmed to be positive based on regular tests (2 cases were confirmed on the 1
st regular test, and 1 person was confirmed on the 2
nd regular test). Additionally, 2 cases, including a patient and her guardian who had stayed in the B1 room, were diagnosed with COVID-19 outside of the hospital. During the outbreak in the B ward, 114 close contacts were notified, and 11 confirmed cases occurred. Based on contact tracing, most of the confirmed patients were epidemiologically related to a case from the B1 room. There was no epidemiological relationship between the A ward outbreak and the B ward outbreak (
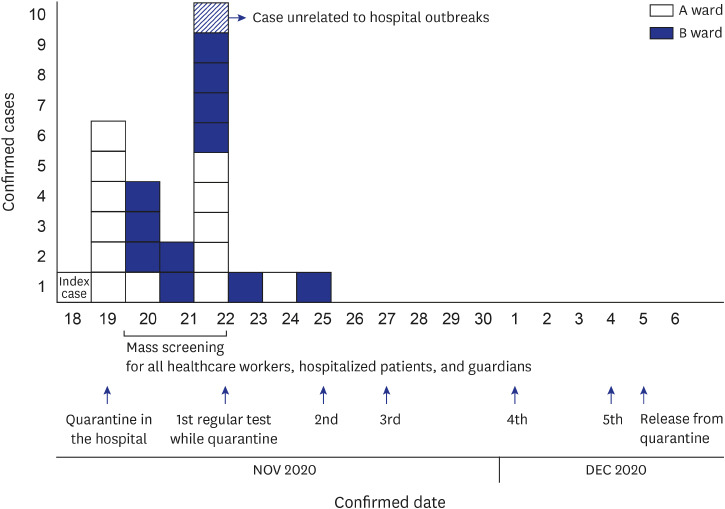
Table 1). All healthcare workers, hospitalized patients, and guardians in the hospital, were tested for SARS-CoV-2 within 3 days, from November 20, 2020. Among them, one person was positive for SARS-CoV-2. She had been working in an administrative role and was not epidemiologically connected with the hospital outbreak. She had COVID-19 symptoms 5 days before testing, and her husband was positive for SARS-CoV-2. She had 5 close contacts in the hospital, none of whom tested positive. Twenty-five cases were confirmed to have SARS-CoV-2 infections in a hospital setting within 7 days of index case diagnosis (
Fig. 1). A total of 186 close contacts for these cases was notified, and all of them were quarantined. The incidence rate of COVID-19 in the community was very low before the index case was identified (0.3 per 100,000 persons in the community; 6.25 per 100,000 persons in Seoul). Although, the incidence rate in the community increased to 15.7 per 100,000 persons during hospital outbreaks, there was no COVID-19 influx from the community into our hospital. The hospital outbreaks occurred in 2 general wards; however, no epidemiological relationship between the A ward outbreak and B ward outbreak was confirmed, and patterns of occurrence were different between the wards. In the A ward, almost all COVID-19 transmissions were epidemiologically linked with the index case. The index case wore a surgical mask while working, but often pulled it down to her chin or removed it. Additionally, review of adherence indicated that most of the confirmed cases did not wear masks while staying in the rooms. To date, substantial evidence has indicated that hospital transmission of SARS-CoV-2 could be reduced by universal use of masks by healthcare personnel and patients.
567 The B ward outbreak mainly occurred in a single 5-person room (B-1 room). About 80% (9/11) of confirmed cases in the B ward were closely related with the B-1 room. Because the guardians stayed in the room with the patients, which was based on the hospital policy for patient care, this room capacity caused spatial crowding that resulted in increased risk for COVID-19 transmission.
8 The B ward outbreak began with 2 patients diagnosed with COVID-19 based on evaluation of acute fever. Based on hospital policy, all patients who stayed in the B-1 room had been tested for SARS-CoV-2 before admission to mitigate risk and detection of asymptomatic patients. Consequently, a negative COVID-19 test result on admission could provide false assurance and delay retesting for onset of acute fever. We considered that failure of early detection could have impacted the B-1 cases and increased the possibility for COVID-19. In this outbreak, about 30% (7/25) of confirmed cases were guardians. Most of the confirmed guardians did not adhere to appropriate use of masks and were usually unmasked during their stay in a room. Thirty percent of confirmed guardian cases occurred without an incidence of COVID-19 infection in their corresponding patients. This finding strongly suggests that guardians staying in the hospital should adhere to masking guidelines. During hospital outbreak, confirmed patients were expeditiously moved into isolation rooms, and close contacts were quarantined at home or in the hospital. This approach was important to minimize the number of quarantined persons in the hospital and to disperse them in separate rooms as soon as possible. Regular testing of close contacts quarantined in the hospital facilitated early detection of COVID-19.
 | Fig. 1Epidemiological characteristics of nosocomial outbreaks.
|
Table 1
Demographic and clinical characteristics of nosocomial outbreaks in 2 general wards

|
Variables |
A ward |
B ward |
|
Type of ward |
General ward: 27 beds in 16 rooms, including single, 2-person, and 3-person rooms. |
General ward: 38 beds in 10 rooms, including and 2-person and 5-person rooms. |
|
First confirmed cases |
Index case |
Two patients staying in B-1 room |
|
Ward outbreak factors |
Epidemiologically linked with index case |
Failure to recognize early onset in COVID-19 patient(s) |
|
Confirmed cases/close contacts, No. (%) |
|
|
|
Total |
13/72 (18) |
11/114 (9.6) |
|
Patients |
6/34 (16.6) |
6/52 (11.5) |
|
Guardians |
3/22 (13.6) |
3/43 (7.0) |
|
Healthcare workersa
|
4/16 (25) |
2/19 (10.5) |
|
COVID-19 confirmation, No. (%) |
|
|
|
During contact tracing |
7 (53.8) |
6 (77.8) |
|
Developed symptoms while quarantined |
4 (30.8) |
0 |
|
Regular tests while quarantined |
2 (15.4) |
3 (22.2) |

This study has several limitations. First, there was no analysis of the genome sequence of SARS-CoV-2 virus from the confirmed cases. COVID-19 environmental tests of surfaces, especially in the B-1 room, were not performed. Finally, it was difficult to perform epidemiological investigations in the hospital. There were several distinctive factors for this hospital outbreak, such as pre-symptomatic transmission, early detection failure in a crowded room, and unmasking or inappropriate adherence to masking guidelines. Therefore, to minimize the risk of transmission, all individuals in a hospital setting should adhere to appropriate masking protocols, and physicians and healthcare workers should be vigilant in their endeavors to identify cases of COVID-19 as soon as possible.
Go to :