INTRODUCTION
Hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) are major nosocomial infections that increase mortality and morbidity in hospitals despite improvement in antibiotic treatment and supportive care, and dissemination of preventive measures.
1234 The occurrence of HAP/VAP, especially if its pathogen is multidrug resistant, is associated with an increase in medical expenses,
56 and the suffering of patients and their families also increases. Moreover, poorly-treated HAP/VAP is a major cause of increased mortality.
1 Therefore, it is important to properly treat HAP/VAP. To do so, it is essential to determine the distribution of the causative microorganisms in the region and the status of local antibiotics resistance.
78 However, there are still insufficient data on this in Korea.
910
The purpose of this study was to investigate the occurrence and causative strains of HAP/VAP, the distribution of resistant bacteria, the use of antibiotics, and the ensuing outcomes of patients in tertiary medical institutions in Korea.
METHODS
Study design
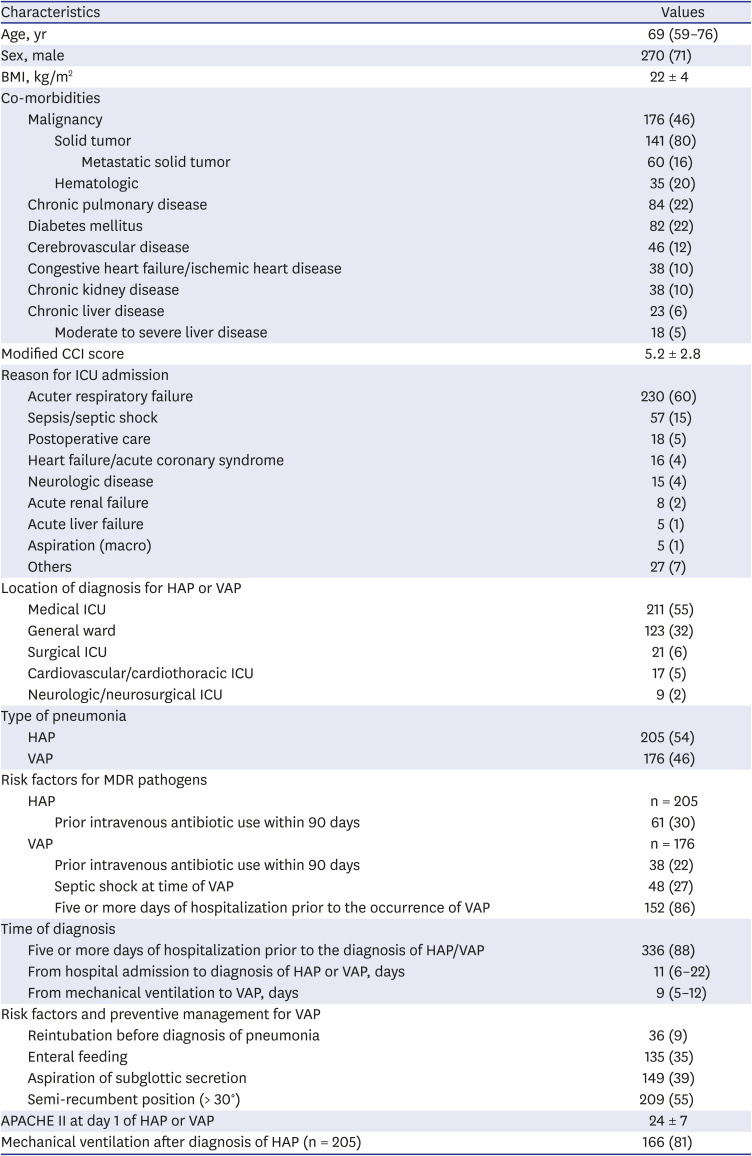
This was a multicenter prospective cohort study conducted with patients with HAP/VAP admitted to the intensive care units (ICUs) in five tertiary referral centers. The demographic and clinical data of the patients were collected.
Subjects
Patients were eligible if they were admitted to the ICU between August 2012 and June 2015 and if they met all of the following criteria: 1) Admission to the adult ICU, 2) Age > 18 years old, 3) New-onset HAP or VAP, and 4) If more than one HAP or VAP was present during hospitalization, only the first event was included.
The exclusion criteria were as follows: 1) Terminal illness with patient consent for ‘Do Not Resuscitate (DNR)’, 2) Terminal solid and hematologic malignancy without an active treatment plan, 3) A history of solid organ transplantation or bone marrow transplantation, 4) Pregnancy or less than 4 weeks postpartum, 5) Ongoing treatment for acquired immune deficiency syndrome, 6) Reception of antibiotics for more than 72 hours from another hospital, and 7) Transfer from other hospitals and subsequent development of new-onset pneumonia within 48 hours.
Data collection
Data on the following demographic and clinical parameters were prospectively collected: age, gender, body mass index (BMI), co-morbidities, reason for ICU admission, place of diagnosis for HAP/VAP, type of pneumonia, risk factors for multidrug-resistant (MDR) pathogens, time of diagnosis, severity scores as Acute Physiology and Chronic Health Evaluation (APACHE) II and Sequential Organ Failure Assessment (SOFA) score, clinical response as Clinical Pulmonary Infection Score (CPIS), pathogens, the presence of colonization for pathogens and antibiotic treatment. The following clinical outcome data were collected: day 3 improvement, day 7 failure, day 28 resolution, day 60 relapse, and 28-day and 60-day mortality.
Definitions
HAP was defined as pneumonia that occurred 48 hours or more after admission, which was not incubating at the time of admission.
1 VAP was defined as pneumonia that occurred more than 48–72 hours after endotracheal intubation.
1 Pneumonia was defined as new and persistent pulmonary infiltration plus at least two of following items: 1) A core body temperature ≥ 38.0°C or ≤ 36°C, 2) leukocytosis with a white blood cell count of ≥ 11,000/mm
3 or leukopenia with a white blood cell count of ≤ 4,000/mm
3, and 3) purulent sputum or endotracheal aspirate. As clinical response indicators, Day 3 improvement was defined as day 3 CPIS reaching ≤ 6 or decreased by ≥ 2 points with respect to day 1 CPIS. Day 7 failure was defined as day 7 CPIS not being lower than 6 or failing to decrease ≥ 2 points with respect to day 1 CPIS, or if the PaO
2/FiO
2 ratio was not improving between day 1 and day 7. Day 28 resolution was defined as complete patient recovery and the stoppage of all antibiotics for pneumonia within 28 days. Day 60 relapse was defined pneumonia caused by the same pathogen occurring again within 4 weeks after antibiotics were stopped due to clinical improvement. The antibiotic therapy was judged as appropriate when the causative microorganism was susceptible to one or more of the prescribed antibiotics based on the in vitro antibiotic susceptibility testing. Bacteremia was defined as at least one positive blood culture for the causative organism of pneumonia. The isolated strain was recognized as the pathogen, only in the following cases; 1) quantitative culture of bronchoalveolar lavage samples (≥ 10
4 colony-forming unit [CFU]/mL), 2) quantitative culture of bronchoscopic aspirates (≥ 10
5 CFU/mL), 3) quantitative culture of endotracheal aspirates (≥ 10
5 CFU/mL), 4) semi-quantitative culture of endotracheal aspirates (moderate [or 3+] or higher), or 5) a strain cultured in adequate sputum (less than 10 epithelial cells in a low power field).
Statistical analysis
Continuous variables are reported as medians (interquartile range [IQR], 25–75%) or means ± standard deviation (SD), and categorical variables are reported as frequencies (percentages). To assess the differences between the groups, data were compared using the t-test or Mann-Whitney U test for continuous variables, while the χ2 or Fisher's exact test was used to compare categorical variables. In the serial analysis of the severity score, each period was analyzed using paired t-test. For all analyses, a two-tailed P value < 0.05 was considered statistically significant. To determine the prognostic factors for 28-day mortality, univariate analysis, and multivariate analysis were performed using logistic regression. Statistical analysis was performed using IBM SPSS version 24.0 (SPSS Inc., Chicago, IL, USA).
Ethics statement
This study was approved by the Asan Medical Center Institutional Review Board (study number 2012-0595). The need for informed consent was waived by the board.
DISCUSSION
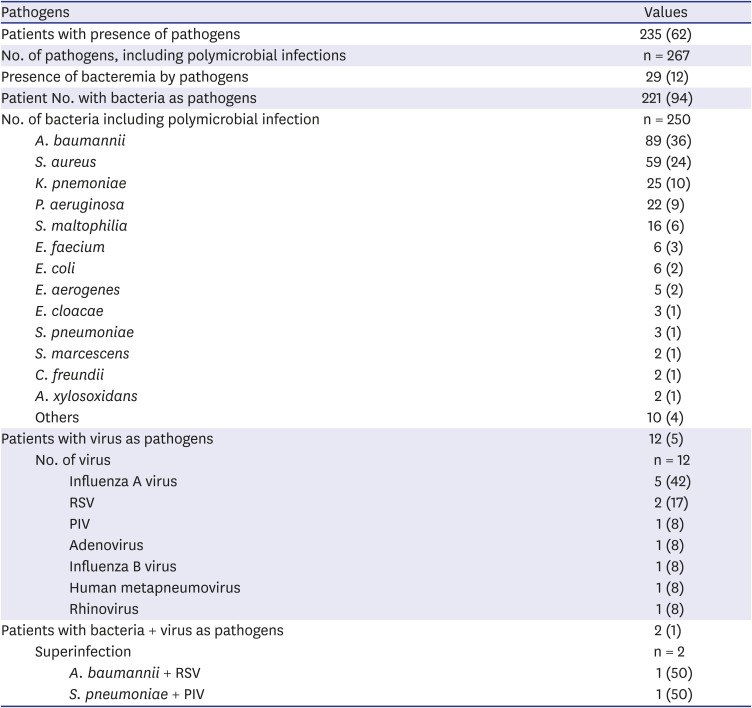
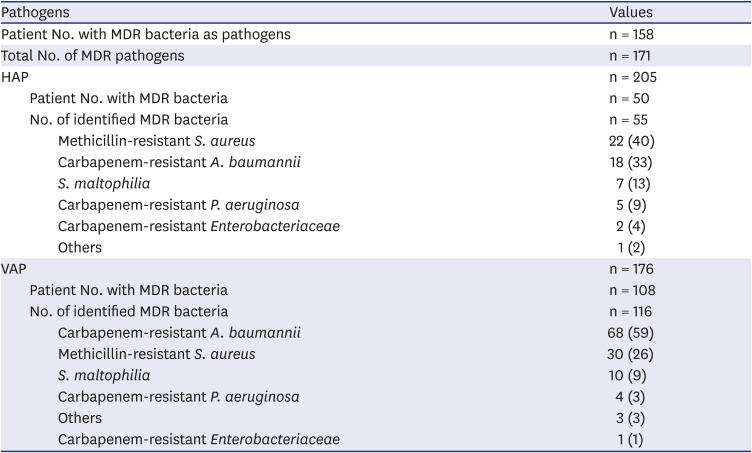
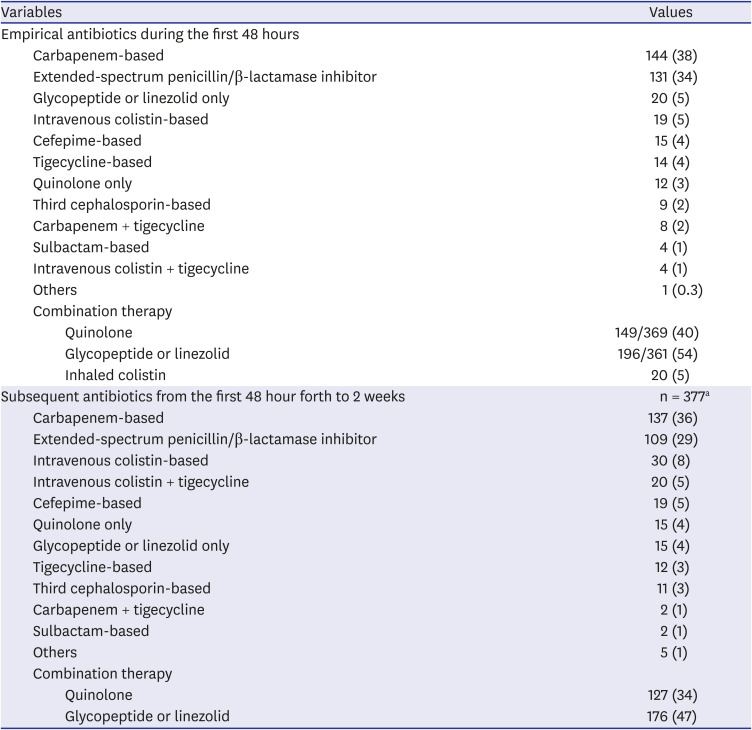
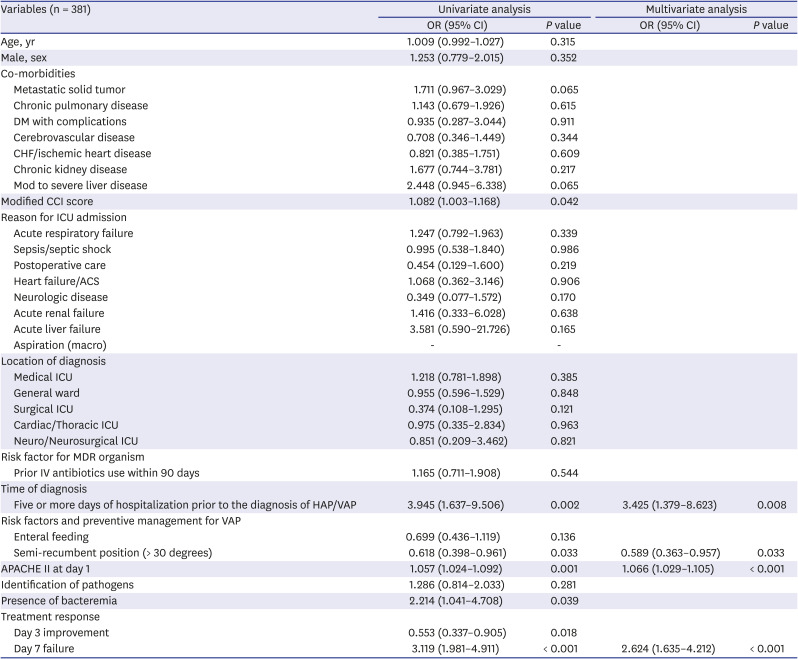
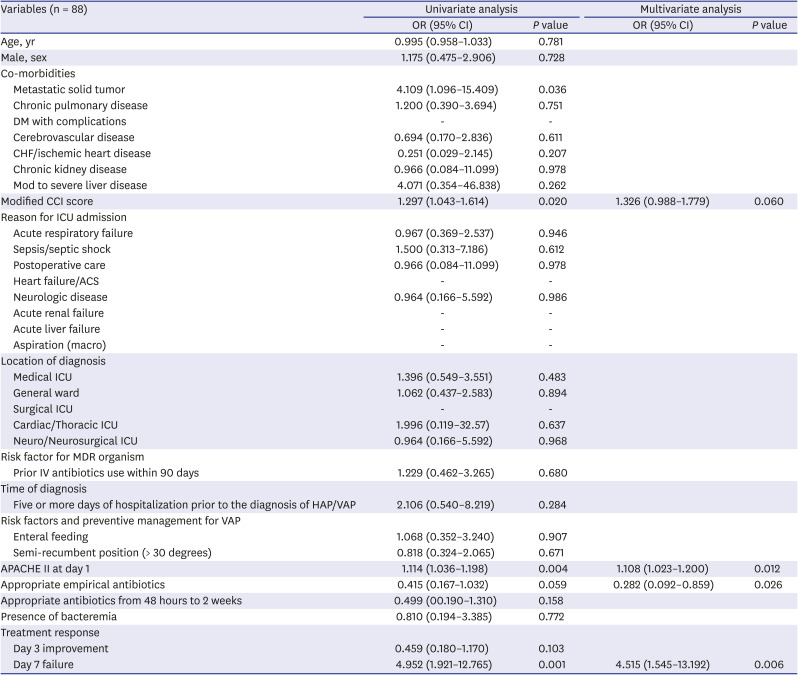
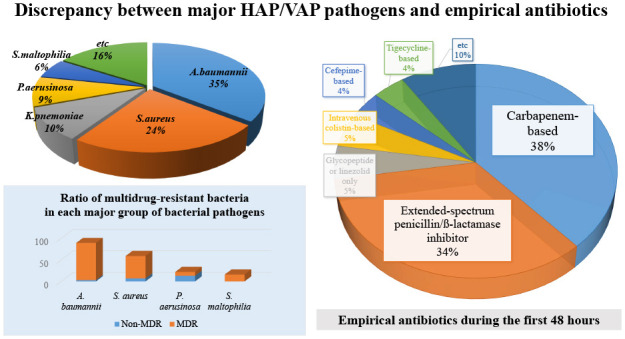
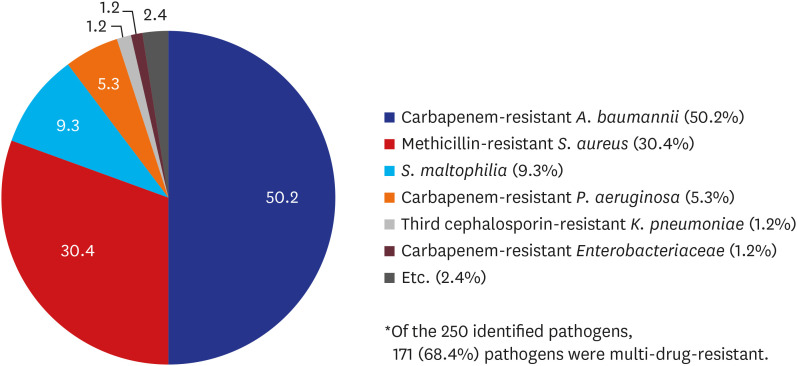
This study aimed to identify the strain distribution and antibiotic selection of HAP/VAP patients in medical ICUs in Korea. The 28-day mortality rate of the patients with HAP/VAP was as high as 30%. The main pathogens responsible for HAP/VAP were A. baumannii and S. aureus, and most strains of A. baumannii and S. aureus were multidrug resistant. On the other hand, the empirical antibiotics, which were started within the first 48 hours of pneumonia, were mainly selected as carbapenem-based or extended-spectrum penicillin/β-lactamase inhibitor-based regimens, showing a discordance between the selection of antibiotics and the main strains. This suggests that a different standard is needed for empirical antibiotic selection in patients with HAP/VAP in domestic medical institutions.
The most commonly encountered strains in our study were
A. baumannii and
S. aureus. In HAP,
S. aureus (22%),
A. baumannii (19%),
K. pneumoniae (15%), and
P. aeruginosa (8%) were in that order, and in VAP,
A. baumannii (46%),
S. aureus (22%),
P. aeruginosa (8%), and
S. maltophilia (7%). In a prior study conducted in the 1990s, a multicenter surveillance of nosocomial infections was carried out in tertiary referral centers in Korea,
S. aureus (45%) and
P. aeruginosa (23%) were the two main strains identified in patients with nosocomial pneumonia.
11 Whereas, 10 years later, in a study conducted in Asian countries (including Korea),
A. baumannii emerged as a major strain responsible for nosocomial pneumonia, especially VAP.
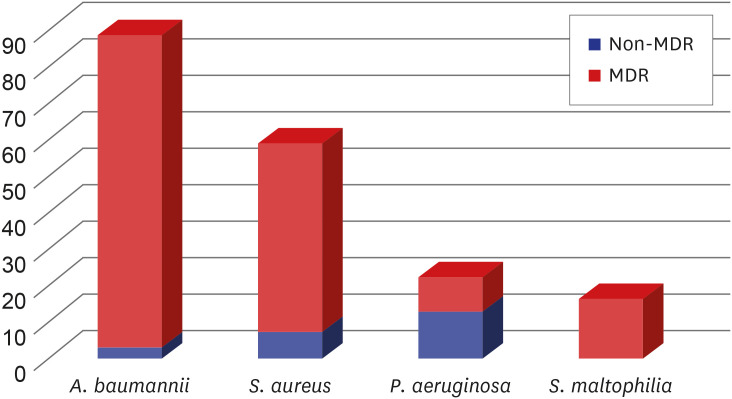
12 In terms of the distribution of MDR microorganisms, our study showed that the MDR rates of
A. baumannii,
S. aureus, and
P. aeruginosa were 97%, 88%, and 41%, respectively. Compared to the data from the Asian countries whose rates were 82%, 82%, and 43%, respectively, the overall trends were in line with our results, although it was a little higher.
12 At the same time, the distribution of these strains in the European countries or the U.S was different.
413 In a previous study of 27 ICUs in nine countries in Europe,
13 the most common bacteria in nosocomial pneumonia patients who underwent mechanical ventilation were
S. aureus (32%),
P. aeruginosa (23%), and
A. baumannii (19%). However, when comparing the three most common strains in each participating country,
A. baumannii was not included in seven western European countries, which results were in line with U.S data.
4 On the other hand, in Greece and Turkey, the two remaining countries of the European study, the burden of
A. baumannii was highest, in line with our results.
A. baumannii is usually classified as a pathogen with low virulence.
214 The problem is that when antibiotic resistance is acquired, the range of alternative treatment options becomes limited. In the end, it is important to prevent
A. baumannii from gaining drug resistance and to prevent further spread of strains that are already resistant to antibiotics.
1516 In this regard, the role of infection control and antimicrobial stewardship in each country and each hospital is important. It could be the reason why the proportion of
A. baumannii is lower in high-income countries than in middle and low-income countries. This suggests that the need for more thorough infection control should be further emphasized in Korea.
The present study demonstrated a significant difference in survival rate depending on whether the causative organisms were susceptible to the empirical antibiotics used within 48 hours of HAP/VAP. The results of this study are similar to those of previous ones.
17181920 In particular, in our study, the administration of adequate empirical antibiotics was a major determinant of the 28-day survival in HAP patients. The appropriate use of empirical antibiotics could help improve patients' prognosis; however, in reality, antibiotics are usually not administered properly as intravenous colistin was used as an empirical antibiotic in only about 5% of patients. If we look at the reasons, in the ICU setting, potentially-resistant microorganisms were the main strains responsible for HAP/VAP in the present study. Considering the previously known local microbiological epidemiology,
12 it is appropriate to use empirical antibiotics targeting these multidrug resistant bacteria; however, the main reason for not doing so is the lack of investigation or understanding of local epidemiologic data, and, more importantly, the concerns about the unnecessary adverse effect and potential toxicity of antibiotics and the emergence of resistance.
21 In particular, for critically-ill patients who often suffer from renal insufficiency, physicians could hesitate to use potentially nephrotoxic antibiotics before the identification of the culprit microorganisms. Third, there is the issue of insurance. In Korea, insurance coverage for colistin is difficult if carbapenem-resistant microorganisms are not isolated. This will also be another reason why medical staff are hesitant to use it as an empirical antibiotic. Considering these aspects, this might be a difficult problem to solve, at least until drugs that can cover these bacteria without adversely affecting organs will be readily available.
Treatment response was evaluated on day 3, day 7, and day 28 in this study. Two-thirds of patients did not show a decrease in CPIS within 72 hours after the start of treatment, while 41% of patients had treatment failure after 1 week of treatment. Only 41% of all the patients completed treatment for pneumonia within 28 days; the remaining 59% either died or are still receiving antibiotics. We investigated whether the treatment response on day 3 and day 7 was associated with patients' 28-day mortality and found that day 3 improvement and day 7 failure were significantly associated with 28-day mortality in univariate analysis; however, in multivariate analysis, only day 7 treatment failure was significantly associated with 28-day mortality (
P < 0.001). Of the 157 patients with treatment failure on day 7 (i.e., no decrease in CPIS or no improvement in the P/F ratio), pneumonia was not completely resolved in 124 (79%) on day 28; their 28-day mortality was 54%, while their 60-day mortality was 73%. Considering the previous literature that looked at the treatment response up to day 5 as an indicator of late treatment failure,
22 day 7 treatment failure was sufficient to evaluate the treatment response, and this study confirmed that it has a significant correlation with the patient's prognosis. Thus, when the patients do not improve within 7 days, taking into account the possibility of continuing deterioration, more careful attention should be paid to whether antibiotics are appropriately selected, whether sufficient supportive care is provided, and to prevent additional VAP. This study revealed that the implementation of the semi-recumbent position (> 30 degrees) was an important factor associated with a lower 28-day mortality. The semi-recumbent position has already been identified as a method of preventing VAP in several studies.
232425 Our results suggested that the sufficient application of this method reduces the risk of additional pneumonia in mechanically-ventilated HAP/VAP patients, which led to better outcomes.
Although this was a prospective multicenter study, it had some limitations. First, the five medical centers that participated in the study consisted of only tertiary hospitals, which is not representative of all patients with HAP/VAP in Korea. Second, in patients who started empirical therapy with broad-spectrum antibiotics, there is a possibility that the adverse effects of the antibiotics used might have affected the patients; however, this has not been specifically investigated. Third, since we only recruited HAP/VAP patients who were admitted to the ICU, not all HAPs that occurred in the hospitals were recruited, as HAPs that occurred and improved in the general ward were not investigated.
In this study, the strains of bacteria responsible for HAP/VAP in tertiary referral hospitals in Korea were associated with a huge burden of MDR bacteria. Proper selection of empirical antibiotics was significantly associated with an improvement the patient's prognosis. In contrast, it was demonstrated that there was a discrepancy between initial empirical antibiotic selection and major strains. In selecting antibiotics, the adverse effects of drugs should be considered important. Future studies based on these domestic microbiologic data are needed to establish criteria for selecting appropriate antibiotics considering all of these factors. In addition, a prompt judgment of the treatment response and prevention of additional pneumonia should not be neglected.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download