This article has been
cited by other articles in ScienceCentral.
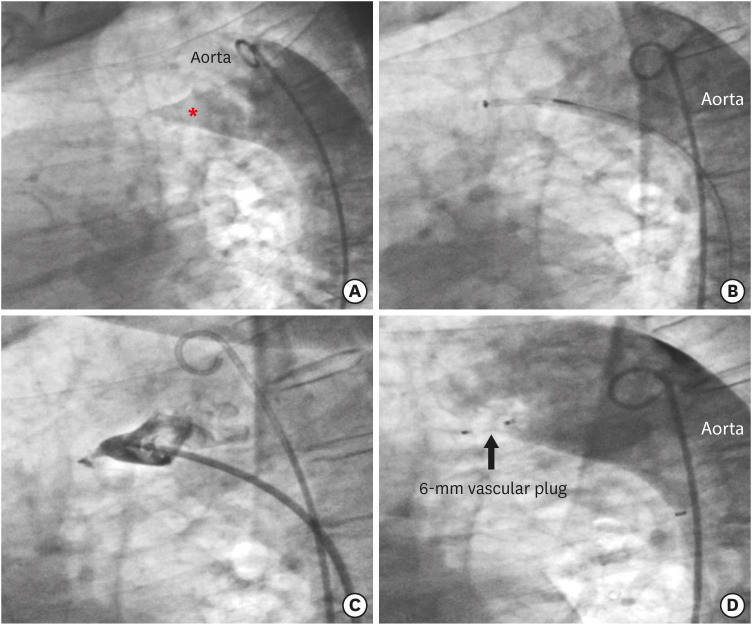
A 58-year-old woman presented with progressive dyspnea. When she was 8 years old, a surgical ligation of her hypertensive patent ductus arteriosus (PDA) was performed by left lateral thoracotomy in the 4th intercostal space under general anesthesia. On this admission, 2-dimensional transthoracic echocardiography/transesophageal echocardiography (TTE/TEE) color Doppler showed dilated left atrium, mildly hypertrophied left ventricle with an ejection fraction of 58% with impaired relaxation; parasternal short axis and suprasternal views showed an enlarged main pulmonary artery and a mild left-to-right shunt via a distorted PDA. Right heart catheterization demonstrated a systolic pulmonary artery pressure of 35 mmHg and a pulmonary flow/systemic flow of 1.1:1. After heart team discussion, a catheter-based treatment was confirmed. Percutaneous closure was performed under local anesthesia and fluoroscopic guidance. Aortic arch angiograms showed an elongated ductus with constriction on the left pulmonary artery opening (type E according to classification of Krichenko) (
Figure 1,
Supplementary Video 1).
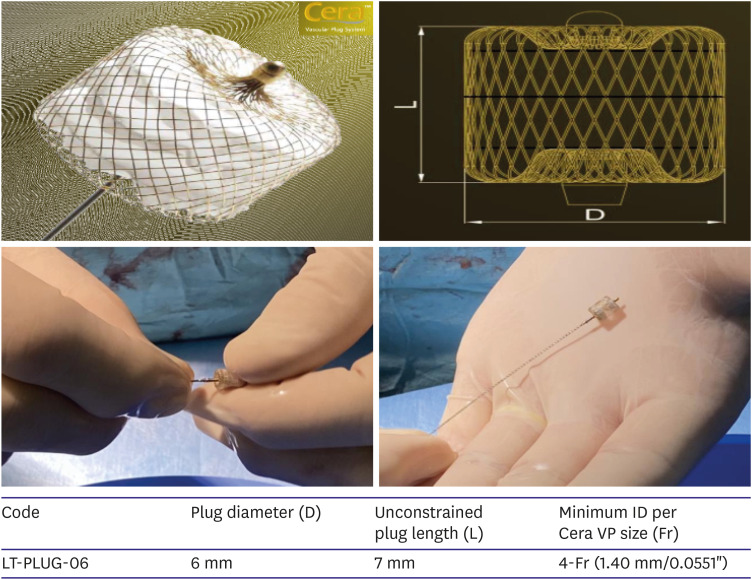
1) A retrograde approach for crossing the residual PDA was chosen. A 4-Fr compatible 6-mm vascular plug system (Cera; Lifetech Scientific, Shenzhen, China) (
Figure 2) was selected for implantation and successfully deployed with abolition of residual shunting (
Supplementary Videos 2,
3). The patient was discharged without complications the following day. At 1-month follow-up she remained symptom free and TTE did not demonstrate any residual shunt flow.
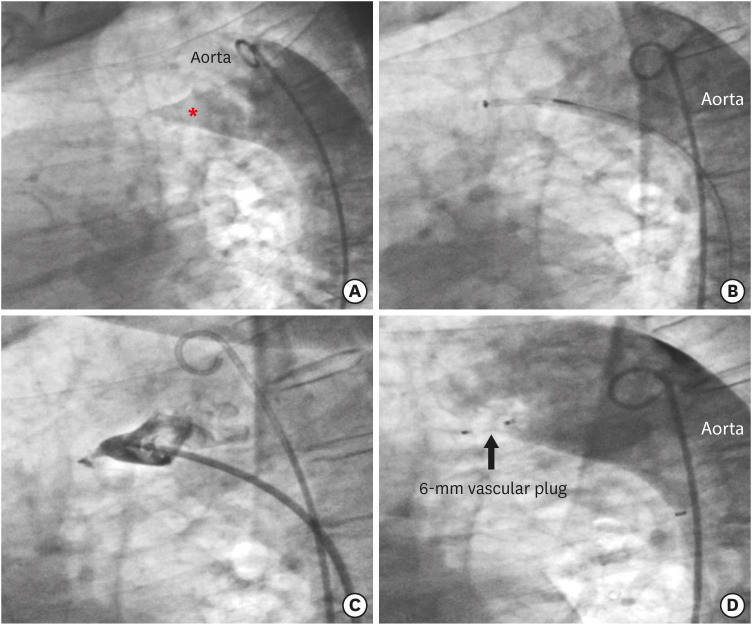 | Figure 1Fluoro-angiographic procedural steps in latero-lateral projection. (A) Baseline aortic arch angiogram showing an elongated patent ductus (red asterisk) with marked narrowing towards the pulmonary artery side (type E, according to angiographic classification of Krichenko). (B) The 5-Fr delivery system passed retrogradely through the patent ductus arteriosus from the aorta and the 6-mm vascular plug system (Cera; Lifetech Scientific, Shenzhen, China) is being advanced inside it. (C) A selective angiogram through the 5-Fr delivery system confirming the position of the 6-mm vascular plug with a tiny residual shunt. (D) Final aortic arch angiogram showing abolition of the left-to-right shunt and the correct position of the occluding device.
|
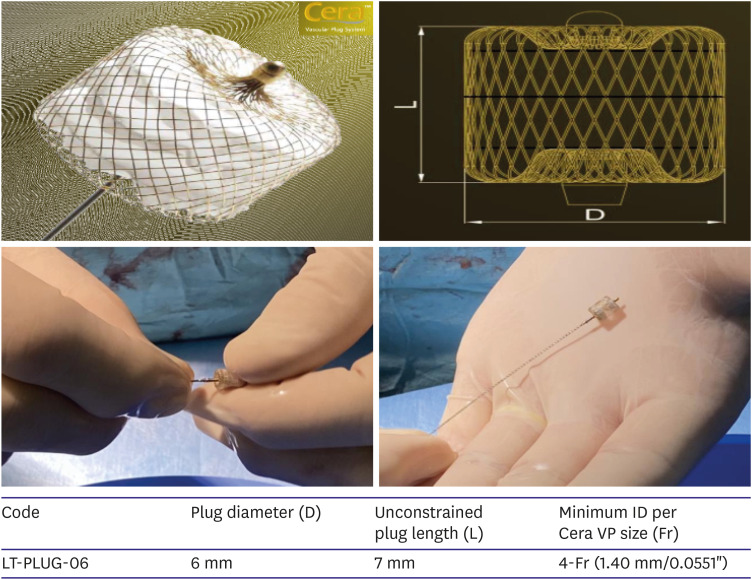 | Figure 2The vascular plug system (Cera; Lifetech Scientific, Shenzhen, China) is a self-expandable, cylindrical device coated with proprietary titanium nitride and available in various sizes range. Polytetrafluoroethylene membranes are dense and securely sewn into device to fill up the hole and block blood flow. In particular LT-PLUG-06 is 4-Fr compatible with an unconstrained plug length of 7 mm.
|
Purse-string sutures, PDA ligation and clip, double clip application or ligation and division are safe and more effective procedures than PDA ligation only. Actually, recanalization after simple ligation may cause residual shunts, whose reported frequency is not negligible and varies from 6% to 23%.
2)3)4)5) In summary, routine transcatheter closure of any residual PDA appears to be the most reasonable choice, given the great feasibility and very low morbidity of this standard of care treatment.
Written informed consent was obtained from the patient.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download