1. Seo HS, Lee IH, Song YW, et al. A case of congenital hypertrophic cardiomyopathy. Korean Circ J. 2013; 43:54–56. PMID:
23407623.

2. Lipshultz SE, Law YM, Asante-Korang A, et al. Cardiomyopathy in children: classification and diagnosis: a scientific statement from the American Heart Association. Circulation. 2019; 140:e9–68. PMID:
31132865.

3. Oh JH, Hong YM, Choi JY, et al. Idiopathic cardiomyopathies in Korean children: 9-year Korean multicenter study. Circ J. 2011; 75:2228–2234. PMID:
21747192.
4. Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2020; 76:3022–3055. PMID:
33229115.
5. Bamborschke D, Özdemir Ö, Kreutzer M, et al. Ultra-rapid emergency genomic diagnosis of Donahue syndrome in a preterm infant within 17 hours. Am J Med Genet A. 2021; 185:90–96. PMID:
33048476.

6. Lafreniere-Roula M, Bolkier Y, Zahavich L, et al. Family screening for hypertrophic cardiomyopathy: is it time to change practice guidelines? Eur Heart J. 2019; 40:3672–3681. PMID:
31170284.

7. Helms AS, Tang VT, O'Leary TS, et al. Effects of
MYBPC3 loss-of-function mutations preceding hypertrophic cardiomyopathy. JCI Insight. 2020; 5:e133782.

8. Kolokotronis K, Kühnisch J, Klopocki E, et al. Biallelic mutation in
MYH7 and
MYBPC3 leads to severe cardiomyopathy with left ventricular noncompaction phenotype. Hum Mutat. 2019; 40:1101–1114. PMID:
30924982.
9. Xin B, Puffenberger E, Tumbush J, Bockoven JR, Wang H. Homozygosity for a novel splice site mutation in the cardiac myosin-binding protein C gene causes severe neonatal hypertrophic cardiomyopathy. Am J Med Genet A. 2007; 143A:2662–2667. PMID:
17937428.

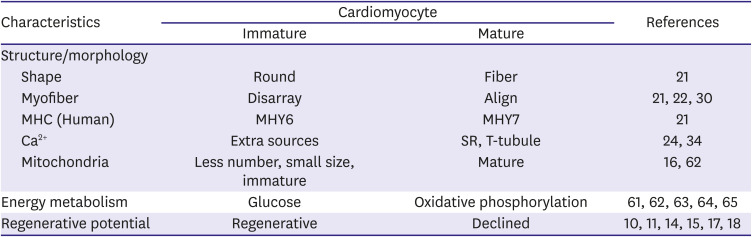
10. Bergmann O, Zdunek S, Felker A, et al. Dynamics of cell generation and turnover in the human heart. Cell. 2015; 161:1566–1575. PMID:
26073943.

11. Zhu W, Zhang E, Zhao M, et al. Regenerative potential of neonatal porcine hearts. Circulation. 2018; 138:2809–2816. PMID:
30030418.

12. Galdos FX, Guo Y, Paige SL, VanDusen NJ, Wu SM, Pu WT. Cardiac regeneration: lessons from development. Circ Res. 2017; 120:941–959. PMID:
28302741.
13. Bergmann O, Bhardwaj RD, Bernard S, et al. Evidence for cardiomyocyte renewal in humans. Science. 2009; 324:98–102. PMID:
19342590.

14. Porrello ER, Mahmoud AI, Simpson E, et al. Transient regenerative potential of the neonatal mouse heart. Science. 2011; 331:1078–1080. PMID:
21350179.

15. Mollova M, Bersell K, Walsh S, et al. Cardiomyocyte proliferation contributes to heart growth in young humans. Proc Natl Acad Sci U S A. 2013; 110:1446–1451. PMID:
23302686.

16. Garbern JC, Lee RT. Mitochondria and metabolic transitions in cardiomyocytes: lessons from development for stem cell-derived cardiomyocytes. Stem Cell Res Ther. 2021; 12:177. PMID:
33712058.

17. Soonpaa MH, Kim KK, Pajak L, Franklin M, Field LJ. Cardiomyocyte DNA synthesis and binucleation during murine development. Am J Physiol. 1996; 271:H2183–9. PMID:
8945939.

18. Naqvi N, Li M, Calvert JW, et al. A proliferative burst during preadolescence establishes the final cardiomyocyte number. Cell. 2014; 157:795–807. PMID:
24813607.

19. Senyo SE, Lee RT, Kühn B. Cardiac regeneration based on mechanisms of cardiomyocyte proliferation and differentiation. Stem Cell Res (Amst). 2014; 13:532–541.

20. Bishop SP, Zhou Y, Nakada Y, Zhang J. Changes in cardiomyocyte cell cycle and hypertrophic growth during fetal to adult in mammals. J Am Heart Assoc. 2021; 10:e017839. PMID:
33399005.

21. Guo Y, Pu WT. Cardiomyocyte maturation: new phase in development. Circ Res. 2020; 126:1086–1106. PMID:
32271675.
22. Guo Y, Cao Y, Jardin BD, et al. Sarcomeres regulate murine cardiomyocyte maturation through MRTF-SRF signaling. Proc Natl Acad Sci U S A. 2021; 118:e2008861118. PMID:
33361330.

23. Seok H, Deng R, Cowan DB, Wang DZ. Application of CRISPR-Cas9 gene editing for congenital heart disease. Clin Exp Pediatr. 2021; 64:269–279. PMID:
33677855.

24. Guo Y, Jardin BD, Zhou P, et al. Hierarchical and stage-specific regulation of murine cardiomyocyte maturation by serum response factor. Nat Commun. 2018; 9:3837. PMID:
30242271.

25. Guo Y, VanDusen NJ, Zhang L, et al. Analysis of cardiac myocyte maturation using CASAAV, a platform for rapid dissection of cardiac myocyte gene function in vivo. Circ Res. 2017; 120:1874–1888. PMID:
28356340.

26. Pierpont ME, Brueckner M, Chung WK, et al. Genetic basis for congenital heart disease: revisited: a scientific statement from the American Heart Association. Circulation. 2018; 138:e653–711. PMID:
30571578.

27. Akerberg BN, Pu WT. Genetic and epigenetic control of heart development. Cold Spring Harb Perspect Biol. 2020; 12:a036756. PMID:
31818853.

28. Cutie S, Huang GN. Vertebrate cardiac regeneration: evolutionary and developmental perspectives. Cell Regen (Lond). 2021; 10:6.

29. Taber LA. Biomechanics of cardiovascular development. Annu Rev Biomed Eng. 2001; 3:1–25. PMID:
11447055.

30. Fukuda R, Gunawan F, Ramadass R, et al. Mechanical forces regulate cardiomyocyte myofilament maturation via the VCL-SSH1-CFL axis. Dev Cell. 2019; 51:62–77.e5. PMID:
31495694.

31. Hines MH. Neonatal cardiovascular physiology. Semin Pediatr Surg. 2013; 22:174–178. PMID:
24331090.

32. Bubb KJ, Cock ML, Black MJ, et al. Intrauterine growth restriction delays cardiomyocyte maturation and alters coronary artery function in the fetal sheep. J Physiol. 2007; 578:871–881. PMID:
17124269.

33. Helms AS, Alvarado FJ, Yob J, et al. Genotype-dependent and -independent calcium signaling dysregulation in human hypertrophic cardiomyopathy. Circulation. 2016; 134:1738–1748. PMID:
27688314.

34. Hamaguchi S, Kawakami Y, Honda Y, et al. Developmental changes in excitation-contraction mechanisms of the mouse ventricular myocardium as revealed by functional and confocal imaging analyses. J Pharmacol Sci. 2013; 123:167–175. PMID:
24096881.

35. Piquereau J, Novotova M, Fortin D, et al. Postnatal development of mouse heart: formation of energetic microdomains. J Physiol. 2010; 588:2443–2454. PMID:
20478976.

36. Atkison P, Joubert G, Barron A, et al. Hypertrophic cardiomyopathy associated with tacrolimus in paediatric transplant patients. Lancet. 1995; 345:894–896. PMID:
7535875.

37. Turska-Kmieć A, Jankowska I, Pawłowska J, et al. Reversal of tacrolimus-related hypertrophic cardiomyopathy after conversion to rapamycin in a pediatric liver transplant recipient. Pediatr Transplant. 2007; 11:319–323. PMID:
17430490.

38. Davis J, Davis LC, Correll RN, et al. A tension-based model distinguishes hypertrophic versus dilated cardiomyopathy. Cell. 2016; 165:1147–1159. PMID:
27114035.

39. Robinson P, Liu X, Sparrow A, et al. Hypertrophic cardiomyopathy mutations increase myofilament Ca
2+ buffering, alter intracellular Ca
2+ handling, and stimulate Ca
2+-dependent signaling. J Biol Chem. 2018; 293:10487–10499. PMID:
29760186.
40. Bensley JG, Moore L, De Matteo R, Harding R, Black MJ. Impact of preterm birth on the developing myocardium of the neonate. Pediatr Res. 2018; 83:880–888. PMID:
29278645.

41. Aye CY, Lewandowski AJ, Lamata P, et al. Disproportionate cardiac hypertrophy during early postnatal development in infants born preterm. Pediatr Res. 2017; 82:36–46. PMID:
28399117.

42. Kannan S, Kwon C. Regulation of cardiomyocyte maturation during critical perinatal window. J Physiol. 2020; 598:2941–2956. PMID:
30571853.

43. Aiyengar A, Howarth C, Pereira S. Hypertrophic cardiomyopathy in an extremely preterm infant. BMJ Case Rep. 2021; 14:14.

44. Doyle LW, Cheong JL, Ehrenkranz RA, Halliday HL. Early (< 8 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2017; 10:CD001146. PMID:
29063585.
45. Halliday HL. Update on postnatal steroids. Neonatology. 2017; 111:415–422. PMID:
28538237.

46. Jiang J, Zhang J, Kang M, Yang J. Transient hypertrophic cardiomyopathy and hypertension associated with hydrocortisone in preterm infant: a case report. Medicine (Baltimore). 2019; 98:e16838. PMID:
31415406.
47. Ramaswamy VV, Bandyopadhyay T, Nanda D, et al. Assessment of postnatal corticosteroids for the prevention of bronchopulmonary dysplasia in preterm neonates: a systematic review and network meta-analysis. JAMA Pediatr. 2021; 175:e206826. PMID:
33720274.
48. Vimala J, Prabhu A, Pavithran S, Kumar RN. Hydrocortisone induced hypertrophic cardiomyopathy. Int J Cardiol. 2011; 150:e94–5. PMID:
20045574.

49. Kale Y, Aydemir O, Ceylan O, Bas AY, Demirel N. Hypertrophic cardiomyopathy after a single dose of dexamethasone in a preterm infant. Pediatr Neonatol. 2015; 56:268–270. PMID:
23639746.
50. Phad NS, de Waal K, Holder C, Oldmeadow C. Dilated hypertrophy: a distinct pattern of cardiac remodeling in preterm infants. Pediatr Res. 2020; 87:146–152. PMID:
31493773.

51. Puente BN, Kimura W, Muralidhar SA, et al. The oxygen-rich postnatal environment induces cardiomyocyte cell-cycle arrest through DNA damage response. Cell. 2014; 157:565–579. PMID:
24766806.

52. Burgoyne JR, Mongue-Din H, Eaton P, Shah AM. Redox signaling in cardiac physiology and pathology. Circ Res. 2012; 111:1091–1106. PMID:
23023511.

53. Seok H, Lee H, Lee S, et al. Position-specific oxidation of miR-1 encodes cardiac hypertrophy. Nature. 2020; 584:279–285. PMID:
32760005.

54. de Salvi Guimarães F, de Moraes WM, Bozi LH, et al. Dexamethasone-induced cardiac deterioration is associated with both calcium handling abnormalities and calcineurin signaling pathway activation. Mol Cell Biochem. 2017; 424:87–98. PMID:
27761848.

55. Sakurai K, Osada Y, Takeba Y, et al. Exposure of immature rat heart to antenatal glucocorticoid results in cardiac proliferation. Pediatr Int. 2019; 61:31–42. PMID:
30387893.

56. Li F, Wang X, Capasso JM, Gerdes AM. Rapid transition of cardiac myocytes from hyperplasia to hypertrophy during postnatal development. J Mol Cell Cardiol. 1996; 28:1737–1746. PMID:
8877783.

57. Velayutham N, Alfieri CM, Agnew EJ, et al. Cardiomyocyte cell cycling, maturation, and growth by multinucleation in postnatal swine. J Mol Cell Cardiol. 2020; 146:95–108. PMID:
32710980.

58. Paech C, Wolf N, Thome UH, Knüpfer M. Hypertrophic intraventricular flow obstruction after very-low-dose dexamethasone (Minidex) in preterm infants: case presentation and review of the literature. J Perinatol. 2014; 34:244–246. PMID:
24573211.

59. Wong IH, Digby AM, Warren AE, Pepelassis D, Vincer M, Chen RP. Dexamethasone given to premature infants and cardiac diastolic function in early childhood. J Pediatr. 2011; 159:227–231. PMID:
21397911.

60. Sperl W, Sengers RC, Trijbels JM, et al. Enzyme activities of the mitochondrial energy generating system in skeletal muscle tissue of preterm and fullterm neonates. Ann Clin Biochem. 1992; 29:638–645. PMID:
1489160.

61. Lai L, Leone TC, Zechner C, et al. Transcriptional coactivators PGC-1alpha and PGC-lbeta control overlapping programs required for perinatal maturation of the heart. Genes Dev. 2008; 22:1948–1961. PMID:
18628400.
62. Dorn GW 2nd, Vega RB, Kelly DP. Mitochondrial biogenesis and dynamics in the developing and diseased heart. Genes Dev. 2015; 29:1981–1991. PMID:
26443844.

63. Gibb AA, Hill BG. Metabolic coordination of physiological and pathological cardiac remodeling. Circ Res. 2018; 123:107–128. PMID:
29929976.

64. Haack TB, Danhauser K, Haberberger B, et al. Exome sequencing identifies
ACAD9 mutations as a cause of complex I deficiency. Nat Genet. 2010; 42:1131–1134. PMID:
21057504.
65. Dewulf JP, Barrea C, Vincent MF, et al. Evidence of a wide spectrum of cardiac involvement due to
ACAD9 mutations: report on nine patients. Mol Genet Metab. 2016; 118:185–189. PMID:
27233227.
66. Wang G, McCain ML, Yang L, et al. Modeling the mitochondrial cardiomyopathy of Barth syndrome with induced pluripotent stem cell and heart-on-chip technologies. Nat Med. 2014; 20:616–623. PMID:
24813252.

67. Ullmo S, Vial Y, Di Bernardo S, et al. Pathologic ventricular hypertrophy in the offspring of diabetic mothers: a retrospective study. Eur Heart J. 2007; 28:1319–1325. PMID:
17158827.

68. Huang T, Kelly A, Becker SA, Cohen MS, Stanley CA. Hypertrophic cardiomyopathy in neonates with congenital hyperinsulinism. Arch Dis Child Fetal Neonatal Ed. 2013; 98:F351–4. PMID:
23377780.

69. Paauw ND, Stegeman R, de Vroede MA, Termote JU, Freund MW, Breur JM. Neonatal cardiac hypertrophy: the role of hyperinsulinism-a review of literature. Eur J Pediatr. 2020; 179:39–50. PMID:
31840185.

70. Bartelds B, Gratama JW, Knoester H, et al. Perinatal changes in myocardial supply and flux of fatty acids, carbohydrates, and ketone bodies in lambs. Am J Physiol. 1998; 274:H1962–9. PMID:
9841523.
71. DeBosch BJ, Muslin AJ. Insulin signaling pathways and cardiac growth. J Mol Cell Cardiol. 2008; 44:855–864. PMID:
18423486.

72. Perge K, Massoud M, Gauthier-Moulinier H, et al. Intrauterine growth restriction and hypertrophic cardiomyopathy as prenatal ultrasound findings in a case of leprechaunism. Mol Syndromol. 2020; 11:223–227. PMID:
33224016.

73. Hayati AR, Cheah FC, Yong JF, Tan AE, Norizah WM. The role of serum insulin-like growth factor I (IGF-I) in neonatal outcome. J Clin Pathol. 2004; 57:1299–1301. PMID:
15563671.

74. Gonzalez AB, Young L, Doll JA, Morgan GM, Crawford SE, Plunkett BA. Elevated neonatal insulin-like growth factor I is associated with fetal hypertrophic cardiomyopathy in diabetic women. Am J Obstet Gynecol. 2014; 211:290.e1–290.e7. PMID:
24813596.

75. Nakano H, Minami I, Braas D, et al. Glucose inhibits cardiac muscle maturation through nucleotide biosynthesis. eLife. 2017; 6:e29330. PMID:
29231167.

76. Gordon EE, Reinking BE, Hu S, et al. Maternal hyperglycemia directly and rapidly induces cardiac septal overgrowth in fetal rats. J Diabetes Res. 2015; 2015:479565. PMID:
26064981.

77. Basu M, Garg V. Maternal hyperglycemia and fetal cardiac development: clinical impact and underlying mechanisms. Birth Defects Res. 2018; 110:1504–1516. PMID:
30576094.

78. Alemu A, Terefe B, Abebe M, Biadgo B. Thyroid hormone dysfunction during pregnancy: a review. Int J Reprod Biomed. 2016; 14:677–686. PMID:
27981252.

79. Männistö T, Mendola P, Reddy U, Laughon SK. Neonatal outcomes and birth weight in pregnancies complicated by maternal thyroid disease. Am J Epidemiol. 2013; 178:731–740. PMID:
23666815.

80. Chattergoon NN. Thyroid hormone signaling and consequences for cardiac development. J Endocrinol. 2019; 242:T145–60. PMID:
31117055.

81. Chattergoon NN, Giraud GD, Louey S, Stork P, Fowden AL, Thornburg KL. Thyroid hormone drives fetal cardiomyocyte maturation. FASEB J. 2012; 26:397–408. PMID:
21974928.

82. Polk DH. Thyroid hormone metabolism during development. Reprod Fertil Dev. 1995; 7:469–477. PMID:
8606958.

83. Williams FL, Simpson J, Delahunty C, et al. Developmental trends in cord and postpartum serum thyroid hormones in preterm infants. J Clin Endocrinol Metab. 2004; 89:5314–5320. PMID:
15531476.

84. Rauen KA. The RASopathies. Annu Rev Genomics Hum Genet. 2013; 14:355–369. PMID:
23875798.

85. Karnik R, Geiger M. Cardiac manifestations of Noonan syndrome. Pediatr Endocrinol Rev. 2019; 16:471–476. PMID:
31115199.
86. Tartaglia M, Mehler EL, Goldberg R, et al. Mutations in
PTPN11, encoding the protein tyrosine phosphatase SHP-2, cause Noonan syndrome. Nat Genet. 2001; 29:465–468. PMID:
11704759.
87. Wilkinson JD, Lowe AM, Salbert BA, et al. Outcomes in children with Noonan syndrome and hypertrophic cardiomyopathy: a study from the Pediatric Cardiomyopathy Registry. Am Heart J. 2012; 164:442–448. PMID:
22980313.

88. Aoki Y, Niihori T, Banjo T, et al. Gain-of-function mutations in
RIT1 cause Noonan syndrome, a RAS/MAPK pathway syndrome. Am J Hum Genet. 2013; 93:173–180. PMID:
23791108.
89. Jaffré F, Miller CL, Schänzer A, et al. Inducible pluripotent stem cell-derived cardiomyocytes reveal aberrant extracellular regulated kinase 5 and mitogen-activated protein kinase kinase 1/2 signaling concomitantly promote hypertrophic cardiomyopathy in
RAF1-associated Noonan syndrome. Circulation. 2019; 140:207–224. PMID:
31163979.
90. Koda M, Takemura G, Okada H, et al. Nuclear hypertrophy reflects increased biosynthetic activities in myocytes of human hypertrophic hearts. Circ J. 2006; 70:710–718. PMID:
16723792.

91. Haubner BJ, Adamowicz-Brice M, Khadayate S, et al. Complete cardiac regeneration in a mouse model of myocardial infarction. Aging (Albany NY). 2012; 4:966–977. PMID:
23425860.

92. D'Uva G, Aharonov A, Lauriola M, et al. ERBB2 triggers mammalian heart regeneration by promoting cardiomyocyte dedifferentiation and proliferation. Nat Cell Biol. 2015; 17:627–638. PMID:
25848746.
93. Basso C, Thiene G, Corrado D, Buja G, Melacini P, Nava A. Hypertrophic cardiomyopathy and sudden death in the young: pathologic evidence of myocardial ischemia. Hum Pathol. 2000; 31:988–998. PMID:
10987261.

94. Nishikawa T, Uto K, Kanai S, et al. Histopathological aspects of cardiac biopsy in pediatric patients with dilated cardiomyopathy. Pediatr Int. 2011; 53:350–353. PMID:
20854285.

95. Hahn A, Lauriol J, Thul J, et al. Rapidly progressive hypertrophic cardiomyopathy in an infant with Noonan syndrome with multiple lentigines: palliative treatment with a rapamycin analog. Am J Med Genet A. 2015; 167A:744–751. PMID:
25708222.

96. Halliday HL. Hypertrophic cardiomyopathy in infants of poorly-controlled diabetic mothers. Arch Dis Child. 1981; 56:258–263. PMID:
7195689.

97. Bui TV, Hwang JW, Lee JH, Park HJ, Ban K. Challenges and limitations of strategies to promote therapeutic potential of human mesenchymal stem cells for cell-based cardiac repair. Korean Circ J. 2021; 51:97–113. PMID:
33525065.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download