1. GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392:1923–1994. PMID:
30496105.
2. Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020; 75:285–292. PMID:
31865786.

3. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020; 16:223–237. PMID:
32024986.

4. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016; 387:957–967. PMID:
26724178.

5. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289:2560–2572. PMID:
12748199.

6. Neal B, MacMahon S, Chapman N. Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists' Collaboration. Lancet. 2000; 356:1955–1964. PMID:
11130523.
7. Psaty BM, Smith NL, Siscovick DS, et al. Health outcomes associated with antihypertensive therapies used as first-line agents. A systematic review and meta-analysis. JAMA. 1997; 277:739–745. PMID:
9042847.

8. SPRINT Research Group. Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103–2116. PMID:
26551272.

9. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39:3021–3104. PMID:
30165516.
10. Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020; 75:1334–1357. PMID:
32370572.

11. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018; 71:e127–248. PMID:
29146535.
12. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016; 134:441–450. PMID:
27502908.
13. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017; 389:37–55. PMID:
27863813.
14. Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008; 336:1114–1117. PMID:
18480115.

15. Tajeu GS, Kent ST, Huang L, et al. Antihypertensive medication nonpersistence and low adherence for adults <65 years initiating treatment in 2007–2014. Hypertension. 2019; 74:35–46. PMID:
31132956.
16. Chowdhury R, Khan H, Heydon E, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013; 34:2940–2948. PMID:
23907142.

17. Corrao G, Parodi A, Nicotra F, et al. Better compliance to antihypertensive medications reduces cardiovascular risk. J Hypertens. 2011; 29:610–618. PMID:
21157368.

18. Mazzaglia G, Ambrosioni E, Alacqua M, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009; 120:1598–1605. PMID:
19805653.

19. Yang Q, Chang A, Ritchey MD, Loustalot F. Antihypertensive medication adherence and risk of cardiovascular disease among older adults: a population-based cohort study. J Am Heart Assoc. 2017; 6:e006056. PMID:
28647688.

20. Lauder L, Böhm M, Mahfoud F. The current status of renal denervation for the treatment of arterial hypertension. Prog Cardiovasc Dis. 2021; 65:76–83. PMID:
33587963.

21. Weber MA, Mahfoud F, Schmieder RE, et al. Renal denervation for treating hypertension: current scientific and clinical evidence. JACC Cardiovasc Interv. 2019; 12:1095–1105. PMID:
31221299.
22. Akinseye OA, Ralston WF, Johnson KC, Ketron LL, Womack CR, Ibebuogu UN. Renal sympathetic denervation: a comprehensive review. Curr Probl Cardiol. 2021; 46:100598. PMID:
32448758.

23. Grassi G, Mark A, Esler M. The sympathetic nervous system alterations in human hypertension. Circ Res. 2015; 116:976–990. PMID:
25767284.

24. DiBona GF. Neural control of the kidney: functionally specific renal sympathetic nerve fibers. Am J Physiol Regul Integr Comp Physiol. 2000; 279:R1517–24. PMID:
11049831.

25. Ciriello J, de Oliveira CV. Renal afferents and hypertension. Curr Hypertens Rep. 2002; 4:136–142. PMID:
11884269.

26. Krum H, Schlaich M, Whitbourn R, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet. 2009; 373:1275–1281. PMID:
19332353.

27. Symplicity HTN-2 Investigators. Esler MD, Krum H, et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet. 2010; 376:1903–1909. PMID:
21093036.
28. Mahfoud F, Ukena C, Schmieder RE, et al. Ambulatory blood pressure changes after renal sympathetic denervation in patients with resistant hypertension. Circulation. 2013; 128:132–140. PMID:
23780578.

29. Vogel B, Kirchberger M, Zeier M, et al. Renal sympathetic denervation therapy in the real world: results from the Heidelberg registry. Clin Res Cardiol. 2014; 103:117–124. PMID:
24126436.

30. Kaiser L, Beister T, Wiese A, et al. Results of the ALSTER BP real-world registry on renal denervation employing the Symplicity system. EuroIntervention. 2014; 10:157–165. PMID:
24472799.

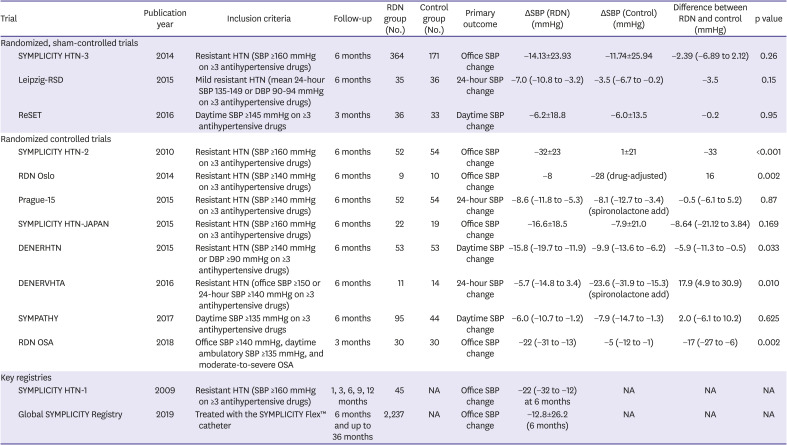
31. Bhatt DL, Kandzari DE, O'Neill WW, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014; 370:1393–1401. PMID:
24678939.

32. Mahfoud F, Bakris G, Bhatt DL, et al. Reduced blood pressure-lowering effect of catheter-based renal denervation in patients with isolated systolic hypertension: data from SYMPLICITY HTN-3 and the Global SYMPLICITY Registry. Eur Heart J. 2017; 38:93–100. PMID:
28158510.

33. Kandzari DE, Bhatt DL, Brar S, et al. Predictors of blood pressure response in the SYMPLICITY HTN-3 trial. Eur Heart J. 2015; 36:219–227. PMID:
25400162.

34. Desch S, Okon T, Heinemann D, et al. Randomized sham-controlled trial of renal sympathetic denervation in mild resistant hypertension. Hypertension. 2015; 65:1202–1208. PMID:
25824248.

35. Mathiassen ON, Vase H, Bech JN, et al. Renal denervation in treatment-resistant essential hypertension. A randomized, SHAM-controlled, double-blinded 24-h blood pressure-based trial. J Hypertens. 2016; 34:1639–1647. PMID:
27228432.

36. Fadl Elmula FE, Hoffmann P, Larstorp AC, et al. Adjusted drug treatment is superior to renal sympathetic denervation in patients with true treatment-resistant hypertension. Hypertension. 2014; 63:991–999. PMID:
24591332.

37. Rosa J, Widimský P, Toušek P, et al. Randomized comparison of renal denervation versus intensified pharmacotherapy including spironolactone in true-resistant hypertension: six-month results from the Prague-15 study. Hypertension. 2015; 65:407–413. PMID:
25421981.
38. Kario K, Ogawa H, Okumura K, et al. SYMPLICITY HTN-Japan: First randomized controlled trial of catheter-based renal denervation in Asian patients. Circ J. 2015; 79:1222–1229. PMID:
25912693.
39. Azizi M, Sapoval M, Gosse P, et al. Optimum and stepped care standardised antihypertensive treatment with or without renal denervation for resistant hypertension (DENERHTN): a multicentre, open-label, randomised controlled trial. Lancet. 2015; 385:1957–1965. PMID:
25631070.

40. Oliveras A, Armario P, Clarà A, et al. Spironolactone versus sympathetic renal denervation to treat true resistant hypertension: results from the DENERVHTA study - a randomized controlled trial. J Hypertens. 2016; 34:1863–1871. PMID:
27327441.
41. de Jager RL, de Beus E, Beeftink MM, et al. Impact of medication adherence on the effect of renal denervation: the SYMPATHY trial. Hypertension. 2017; 69:678–684. PMID:
28264922.
42. Warchol-Celinska E, Prejbisz A, Kadziela J, et al. Renal denervation in resistant hypertension and obstructive sleep apnea: randomized proof-of-concept phase II trial. Hypertension. 2018; 72:381–390. PMID:
29941516.
43. Mahfoud F, Böhm M, Schmieder R, et al. Effects of renal denervation on kidney function and long-term outcomes: 3-year follow-up from the Global SYMPLICITY Registry. Eur Heart J. 2019; 40:3474–3482. PMID:
30907413.

44. Azizi M, Pereira H, Hamdidouche I, et al. Adherence to antihypertensive treatment and the blood pressure-lowering effects of Renal Denervation in the Renal Denervation for Hypertension (DENERHTN) trial. Circulation. 2016; 134:847–857. PMID:
27576780.
45. Hamdidouche I, Gosse P, Cremer A, et al. Clinic versus ambulatory blood pressure in resistant hypertension: impact of antihypertensive medication nonadherence: a post hoc analysis the DENERHTN study. Hypertension. 2019; 74:1096–1103. PMID:
31995406.
46. Mahfoud F, Tunev S, Ewen S, et al. Impact of lesion placement on efficacy and safety of catheter-based radiofrequency renal denervation. J Am Coll Cardiol. 2015; 66:1766–1775. PMID:
26483099.
47. Fengler K, Ewen S, Höllriegel R, et al. Blood pressure response to main renal artery and combined main renal artery plus branch renal denervation in patients with resistant hypertension. J Am Heart Assoc. 2017; 6:e006196. PMID:
28862930.

48. Henegar JR, Zhang Y, Hata C, Narciso I, Hall ME, Hall JE. Catheter-based radiofrequency renal denervation: location effects on renal norepinephrine. Am J Hypertens. 2015; 28:909–914. PMID:
25576624.

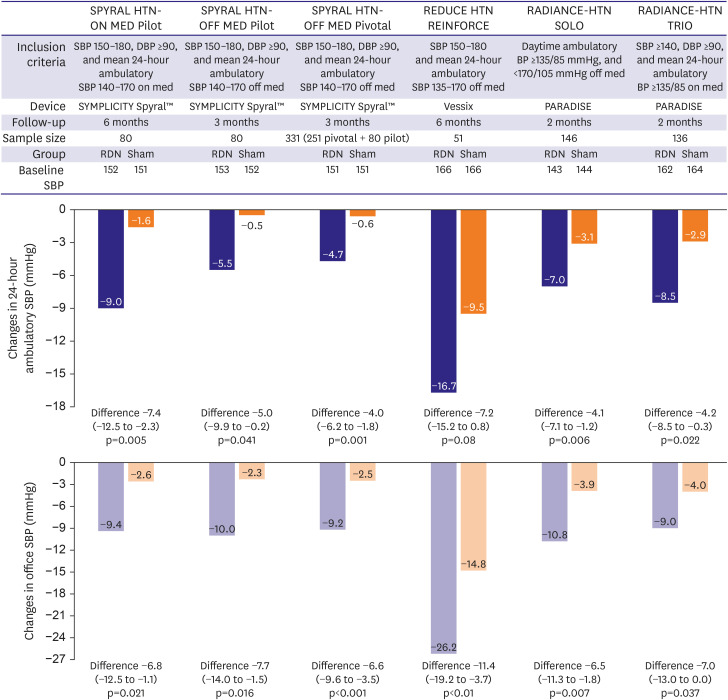
49. Townsend RR, Mahfoud F, Kandzari DE, et al. Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial. Lancet. 2017; 390:2160–2170. PMID:
28859944.
50. Kandzari DE, Böhm M, Mahfoud F, et al. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the SPYRAL HTN-ON MED proof-of-concept randomised trial. Lancet. 2018; 391:2346–2355. PMID:
29803589.
51. Pekarskiy SE, Baev AE, Mordovin VF, et al. Denervation of the distal renal arterial branches vs. conventional main renal artery treatment: a randomized controlled trial for treatment of resistant hypertension. J Hypertens. 2017; 35:369–375. PMID:
28005705.
52. Böhm M, Kario K, Kandzari DE, et al. Efficacy of catheter-based renal denervation in the absence of antihypertensive medications (SPYRAL HTN-OFF MED Pivotal): a multicentre, randomised, sham-controlled trial. Lancet. 2020; 395:1444–1451. PMID:
32234534.
53. Worthley SG, Tsioufis CP, Worthley MI, et al. Safety and efficacy of a multi-electrode renal sympathetic denervation system in resistant hypertension: the EnligHTN I trial. Eur Heart J. 2013; 34:2132–2140. PMID:
23782649.

54. Sievert H, Schofer J, Ormiston J, et al. Renal denervation with a percutaneous bipolar radiofrequency balloon catheter in patients with resistant hypertension: 6-month results from the REDUCE-HTN clinical study. EuroIntervention. 2015; 10:1213–1220. PMID:
25452197.

55. Ormiston JA, Watson T, van Pelt N, et al. First-in-human use of the OneShot™ renal denervation system from Covidien. EuroIntervention. 2013; 8:1090–1094. PMID:
23339814.

56. Kario K, Rumoroso JR, Okawara Y, et al. Renal sympathetic denervation in patients with resistant hypertension: a feasibility study. Pulse (Basel). 2019; 6:137–143. PMID:
31049313.

57. Li Y, Nawabi AQ, Feng Y, Dai Q, Ma G, Liu N. Safety and efficacy of a new renal denervation catheter in hypertensive patients in the absent of antihypertensive medications: a pilot study. Int J Hypertens. 2019; 2019:7929706. PMID:
30906590.

58. Kim CJ, Chang K, Kim BK, Park CG, Jang Y. An open-label, single-arm, multicenter feasibility study evaluating the safety of catheter-based renal denervation with DENEX™ in patients with uncontrolled hypertension on standard medical therapy. Korean Circ J. 2021; 51:43–55. PMID:
33377328.

59. Weber MA, Kirtane AJ, Weir MR, et al. The REDUCE HTN: REINFORCE: randomized, sham-controlled trial of bipolar radiofrequency renal denervation for the treatment of hypertension. JACC Cardiovasc Interv. 2020; 13:461–470. PMID:
32081240.
60. Mabin T, Sapoval M, Cabane V, Stemmett J, Iyer M. First experience with endovascular ultrasound renal denervation for the treatment of resistant hypertension. EuroIntervention. 2012; 8:57–61. PMID:
22580249.

61. Azizi M, Schmieder RE, Mahfoud F, et al. Endovascular ultrasound renal denervation to treat hypertension (RADIANCE-HTN SOLO): a multicentre, international, single-blind, randomised, sham-controlled trial. Lancet. 2018; 391:2335–2345. PMID:
29803590.
62. Azizi M, Schmieder RE, Mahfoud F, et al. Six-month results of treatment-blinded medication titration for hypertension control following randomization to endovascular ultrasound renal denervation or a sham procedure in the RADIANCE-HTN SOLO trial. Circulation. 2019; 139:2542–2553.
63. Azizi M, Daemen J, Lobo MD, et al. 12-Month results from the unblinded phase of the RADIANCE-HTN SOLO trial of ultrasound renal denervation. JACC Cardiovasc Interv. 2020; 13:2922–2933. PMID:
33357531.

64. Azizi M, Sanghvi K, Saxena M, et al. Ultrasound renal denervation for hypertension resistant to a triple medication pill (RADIANCE-HTN TRIO): a randomised, multicentre, single-blind, sham-controlled trial. Lancet. 2021; [Epub ahead of print].
65. Fischell TA, Vega F, Raju N, et al. Ethanol-mediated perivascular renal sympathetic denervation: preclinical validation of safety and efficacy in a porcine model. EuroIntervention. 2013; 9:140–147. PMID:
23685302.

66. Mahfoud F, Renkin J, Sievert H, et al. Alcohol-mediated renal denervation using the peregrine system infusion catheter for treatment of hypertension. JACC Cardiovasc Interv. 2020; 13:471–484. PMID:
32081241.

67. Fengler K, Rommel KP, Blazek S, et al. A three-arm randomized trial of different renal denervation devices and techniques in patients with resistant hypertension (RADIOSOUND-HTN). Circulation. 2019; 139:590–600. PMID:
30586691.

68. Townsend RR, Walton A, Hettrick DA, et al. Review and meta-analysis of renal artery damage following percutaneous renal denervation with radiofrequency renal artery ablation. EuroIntervention. 2020; 16:89–96. PMID:
32038027.

69. Ueshima H, Sekikawa A, Miura K, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008; 118:2702–2709. PMID:
19106393.
70. Wang TD, Goto S, Bhatt DL, et al. Ethnic differences in the relationships of anthropometric measures to metabolic risk factors in Asian patients at risk of atherothrombosis: results from the REduction of Atherothrombosis for Continued Health (REACH) Registry. Metabolism. 2010; 59:400–408. PMID:
19800641.
71. Kario K, Chen CH, Park S, et al. Consensus document on improving hypertension management in Asian patients, taking into account Asian characteristics. Hypertension. 2018; 71:375–382. PMID:
29311253.

72. Arima H, Murakami Y, Lam TH, et al. Effects of prehypertension and hypertension subtype on cardiovascular disease in the Asia-Pacific Region. Hypertension. 2012; 59:1118–1123. PMID:
22547441.

73. Hoshide S, Wang JG, Park S, et al. Treatment considerations of clinical physician on hypertension management in Asia. Curr Hypertens Rev. 2016; 12:164–168. PMID:
26264816.

74. Uzu T, Ishikawa K, Fujii T, Nakamura S, Inenaga T, Kimura G. Sodium restriction shifts circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation. 1997; 96:1859–1862. PMID:
9323073.

75. Kario K, Bhatt DL, Brar S, Bakris GL. Differences in dynamic diurnal blood pressure variability between Japanese and American treatment-resistant hypertensive populations. Circ J. 2017; 81:1337–1345. PMID:
28458378.

76. Omboni S, Aristizabal D, De la Sierra A, et al. Hypertension types defined by clinic and ambulatory blood pressure in 14 143 patients referred to hypertension clinics worldwide. Data from the ARTEMIS study. J Hypertens. 2016; 34:2187–2198. PMID:
27512964.

77. Zhou HH, Koshakji RP, Silberstein DJ, Wilkinson GR, Wood AJ. Racial differences in drug response. Altered sensitivity to and clearance of propranolol in men of Chinese descent as compared with American whites. N Engl J Med. 1989; 320:565–570. PMID:
2536896.
78. Kario K, Kim BK, Aoki J, et al. Renal denervation in Asia: consensus statement of the Asia Renal Denervation Consortium. Hypertension. 2020; 75:590–602. PMID:
32008432.
79. Yang JH, Choi SH, Gwon HC. Percutaneous renal sympathetic denervation for the treatment of resistant hypertension with heart failure: first experience in Korea. J Korean Med Sci. 2013; 28:951–954. PMID:
23772164.

80. Kim BK, Böhm M, Mahfoud F, et al. Renal denervation for treatment of uncontrolled hypertension in an Asian population: results from the Global SYMPLICITY Registry in South Korea (GSR Korea). J Hum Hypertens. 2016; 30:315–321. PMID:
26155994.

81. Stavropoulos K, Patoulias D, Imprialos K, et al. Efficacy and safety of renal denervation for the management of arterial hypertension: a systematic review and meta-analysis of randomized, sham-controlled, catheter-based trials. J Clin Hypertens (Greenwich). 2020; 22:572–584. PMID:
32049436.

82. Agasthi P, Shipman J, Arsanjani R, et al. Renal denervation for resistant hypertension in the contemporary era: a systematic review and meta-analysis. Sci Rep. 2019; 9:6200. PMID:
30996305.

83. Cheng X, Zhang D, Luo S, Qin S. Effect of catheter-based renal denervation on uncontrolled hypertension: a systematic review and meta-analysis. Mayo Clin Proc. 2019; 94:1695–1706. PMID:
31402054.

84. Francis GS, Goldsmith SR, Levine TB, Olivari MT, Cohn JN. The neurohumoral axis in congestive heart failure. Ann Intern Med. 1984; 101:370–377. PMID:
6147109.

85. Waagstein F, Bristow MR, Swedberg K, et al. Beneficial effects of metoprolol in idiopathic dilated cardiomyopathy. Lancet. 1993; 342:1441–1446. PMID:
7902479.

86. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet. 1999; 353:9–13. PMID:
10023943.
87. Packer M, Coats AJ, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001; 344:1651–1658. PMID:
11386263.

88. SOLVD Investigators. Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991; 325:293–302. PMID:
2057034.

89. Granger CB, McMurray JJ, Yusuf S, et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme inhibitors: the CHARM-Alternative trial. Lancet. 2003; 362:772–776. PMID:
13678870.

90. Cohn JN, Tognoni G. Valsartan Heart Failure Trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001; 345:1667–1675. PMID:
11759645.

91. Brandt MC, Mahfoud F, Reda S, et al. Renal sympathetic denervation reduces left ventricular hypertrophy and improves cardiac function in patients with resistant hypertension. J Am Coll Cardiol. 2012; 59:901–909. PMID:
22381425.

92. Davies JE, Manisty CH, Petraco R, et al. First-in-man safety evaluation of renal denervation for chronic systolic heart failure: primary outcome from REACH-Pilot study. Int J Cardiol. 2013; 162:189–192. PMID:
23031283.

93. Patel HC, Rosen SD, Hayward C, et al. Renal denervation in heart failure with preserved ejection fraction (RDT-PEF): a randomized controlled trial. Eur J Heart Fail. 2016; 18:703–712. PMID:
26990920.
94. Schotten U, Verheule S, Kirchhof P, Goette A. Pathophysiological mechanisms of atrial fibrillation: a translational appraisal. Physiol Rev. 2011; 91:265–325. PMID:
21248168.

95. Pokushalov E, Romanov A, Corbucci G, et al. A randomized comparison of pulmonary vein isolation with versus without concomitant renal artery denervation in patients with refractory symptomatic atrial fibrillation and resistant hypertension. J Am Coll Cardiol. 2012; 60:1163–1170. PMID:
22958958.

96. Steinberg JS, Shabanov V, Ponomarev D, et al. Effect of renal denervation and catheter ablation vs catheter ablation alone on atrial fibrillation recurrence among patients with paroxysmal atrial fibrillation and hypertension: the ERADICATE-AF randomized clinical trial. JAMA. 2020; 323:248–255. PMID:
31961420.
97. Sarafidis PA, Sharpe CC, Wood E, et al. Prevalence, patterns of treatment, and control of hypertension in predialysis patients with chronic kidney disease. Nephron Clin Pract. 2012; 120:c147–55. PMID:
22678150.

98. Hering D, Mahfoud F, Walton AS, et al. Renal denervation in moderate to severe CKD. J Am Soc Nephrol. 2012; 23:1250–1257. PMID:
22595301.

99. Hering D, Marusic P, Duval J, et al. Effect of renal denervation on kidney function in patients with chronic kidney disease. Int J Cardiol. 2017; 232:93–97. PMID:
28089459.

100. Kiuchi MG, Maia GL, de Queiroz Carreira MA, et al. Effects of renal denervation with a standard irrigated cardiac ablation catheter on blood pressure and renal function in patients with chronic kidney disease and resistant hypertension. Eur Heart J. 2013; 34:2114–2121. PMID:
23786861.

101. Scalise F, Sole A, Singh G, et al. Renal denervation in patients with end-stage renal disease and resistant hypertension on long-term haemodialysis. J Hypertens. 2020; 38:936–942. PMID:
31990900.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download