Depression has been reported to be a risk factor of coronary artery disease (CAD).1) Another study about depression and CAD is set to be published in this current issue of the Korean Circulation Journal. However, it is somewhat different from previous studies.
Kim et al.2) reported a higher prevalence of depression in women with CAD (22% vs. 6.5% without CAD), but no significant increase was observed in men with CAD (5.5% vs. 3.4% without CAD). Although women have been acknowledged to be more susceptible to depression than men,3)4)5)6) this large sex disparity has not been reported. Interestingly, the prevalence was similar to that reported in previous studies (20–30% in women with CAD or acute myocardial infarction, and 5% in the general population)1) except for men with CAD.
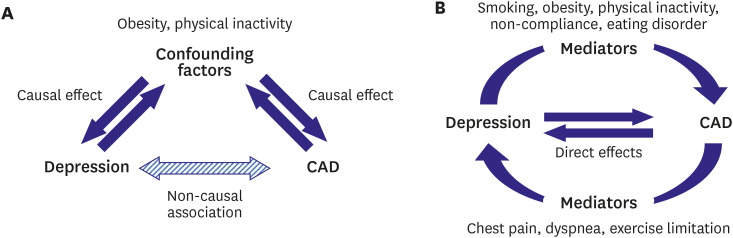
Interpreting the results requires caution as the study is cross-sectional and observational, with misclassification being the most worrisome source of error. The diagnosis of CAD was not medically verified, but based on a survey. People might have thought of chest discomfort and/or dyspnea from psychogenic origins as cardiac problems. In addition, we cannot determine the exact relationship between CAD and depression. From the previous studies, the relationship seems to be bidirectional, and complicated with various mediators and confounding factors such as diabetes mellitus, smoking, physical inactivity, obesity and non-compliance (Figure 1). The relationship and the methods of analysis are interesting issues in epidemiology and biostatistics.
Nevertheless, the high prevalence of depression (up to 30% in women younger than 65 years) has important clinical implication. As the authors have quoted, depression has a significant impact on the prognosis of CAD regardless of the onset.7) Depression itself is a serious disease that needs to be addressed. Hence, even cardiologists should pay attention to the mental health status of their patients, especially young women. It would be worthwhile to include a screening protocol for depression before discharge or at the diagnosis of CAD.
Notes
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
References
1. Carney RM, Freedland KE. Depression and coronary heart disease. Nat Rev Cardiol. 2017; 14:145–155. PMID: 27853162.

2. Kim NH, Lee YH, Kim M. Community-dwelling individuals with coronary artery disease have higher risk of depression than the general population in female, but not in male. Korean Circ J. 2021; 51:752–763.

3. Mallik S, Spertus JA, Reid KJ, et al. Depressive symptoms after acute myocardial infarction: evidence for highest rates in younger women. Arch Intern Med. 2006; 166:876–883. PMID: 16636213.
4. Vaccarino V, Shah AJ, Rooks C, et al. Sex differences in mental stress-induced myocardial ischemia in young survivors of an acute myocardial infarction. Psychosom Med. 2014; 76:171–180. PMID: 24608039.

5. Smolderen KG, Strait KM, Dreyer RP, et al. Depressive symptoms in younger women and men with acute myocardial infarction: insights from the VIRGO study. J Am Heart Assoc. 2015; 4:e001424. PMID: 25836055.

6. Vaccarino V, Badimon L, Bremner JD, et al. Depression and coronary heart disease: 2018 position paper of the ESC working group on coronary pathophysiology and microcirculation. Eur Heart J. 2020; 41:1687–1696. PMID: 30698764.

7. Leung YW, Flora DB, Gravely S, Irvine J, Carney RM, Grace SL. The impact of premorbid and postmorbid depression onset on mortality and cardiac morbidity among patients with coronary heart disease: meta-analysis. Psychosom Med. 2012; 74:786–801. PMID: 23001393.
Figure 1
Relationships between CAD and depression.
(A) Non-causal association by confounding factors. (B) Causal relationships with direct effects and mediators. Some factors can simultaneously act as confounding factors and mediators, making it difficult to analyze and estimate the effect size.
CAD = coronary artery disease.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download