Abstract
The proportion of population vaccinated cannot be directly translated into the herd immunity. We have to account for the age-stratified contact patterns to calculate the population immunity level, since not every individual gathers evenly. Here, we calculated the contact-adjusted population immunity against severe acute respiratory syndrome coronavirus 2 in South Korea using age-specific incidence and vaccine uptake rate. We further explored options to achieve the theoretical herd immunity with age-varying immunity scenarios. As of June 21, 2021, when a quarter of the population received at least one dose of a coronavirus disease 2019 (COVID-19) vaccine, the contact-adjusted immunity level was 12.5% under the social distancing level 1. When 80% of individuals aged 10 years and over gained immunity, we could achieve a 58.2% contact-adjusted immunity level. The pros and cons of vaccinating children should be weighed since the risks of COVID-19 for the young are less than the elderly, and the long-term safety of vaccines is still obscure.
Graphical Abstract
Coronavirus disease 2019 (COVID-19) has swamped the world since the first reported case in November 2019, with 179 million confirmed cases and 3.8 million deaths as of June 26, 2021.1 However, according to the World Health Organization in October 2020, 10% of the global population might have been infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), without even confirmation.2
Given that in mind, South Korea has defended SARS-CoV-2 well with keen public health measures.3 It reported 154,457 confirmed cases and 2,012 deaths as of June 26, 2021, recording a case fatality ratio of 1.3%, which is close to the known infection fatality ratio 1.15% (0.78–1.79%, 95% prediction interval range) in high-income countries.45 This suggests that the South Korean ascertainment ratio is not far from the reality, in line with the low seroprevalence of SARS-CoV-2 specific antibodies as 0.27% in May 2021.
To maintain this status, COVID-19 vaccines are expected to play an important role especially in South Korea, considering that immunity from natural infection is insufficient to reach herd immunity levels (i.e., proportion of immune individuals that lead to a decline of infection). The basic reproduction number (R0) is often cited to be between 2 and 3 for SARS-CoV-2, although a wider range of values is possible.678 Based on these values of R0, the herd immunity level to prevent COVID-19 outbreaks requires a population immunity of 50% to 67% (1 − 1/R0).
To capture reality, transmission-relevant contact occurring between different age groups should be considered in calculating population immunity levels.9 We calculated the contact-adjusted immunity levels against SARS-CoV-2 in South Korea and explored future options to achieve a contact-adjusted immunity level as a herd-immunity threshold.
We used publicly available data reported daily by the Korea Disease Control and Prevention Agency.10 Age-specific immunity levels were estimated by combining the COVID-19 incidence data with vaccine coverage data. We assumed 100% immunity after natural SARS-CoV-2 infection and a vaccine effectiveness of 86.0%, 89.7%, and 66.9% after one dose of AstraZeneca, Pfizer/BioNTech, and Janssen vaccine, respectively.101112
Because social contact patterns in South Korea have not been elucidated, we attempted to find plausible substitutes. We adopted the projected number of contacts between age groups from a study conducted by Prem et al.13 To capture the change of contact patterns as a result of social distancing measures, we accounted for school closure policies and reduced contact rates at both work and other places using Google mobility data.1415 In short, school attendance in South Korea was capped at two-thirds during national distancing level 1, one-third during level 2 (except for high schools which remained at two-thirds), and remote learning only during level 3.4 We also conducted a sensitivity analysis by splitting age groups into two groups: under the age of 20 and 20 years or more, with varying the number of contacts in each group by 0.8 to 1.2 times. Age-structured population data was obtained from Statistics Korea.16
We calculated plain immunity levels as the overall proportion of the population that were immune, and further combined immunity levels with contact data to calculate contact-adjusted immunity levels.917 Briefly, the R0 is defined as the spectral radius (largest eigenvalue, ρ) of the next-generation matrix K.
In the age-structured model, the elements of the next-generation matrix are presented as
where qi denotes the probability that a contact between a susceptible in age group i and an infectious person leads to infection, Φij is the number of contacts an individual of age group j makes with those of age group i. Ni and Nj are the number of individuals in groups i and j, respectively. We used qi values from our previous study (the lowest value of 0.0293, 95% confidence interval [CI; 0.0270–0.0316] in the age group 5 to 10 years; the highest value of 0.157, 95% CI [0.1518–0.1637] in the age group of over 75 years).18
K' is a matrix with elements
where ri is the immunity level in age group i. We interpreted
as contact-adjusted immunity, which is the population immunity once age-specific contact patterns are considered. All analyses were conducted using the R statistical software version 3.6.1 (R foundation for Statistical Computing, Vienna, Austria). Code and data to reproduce the analyses are available at https://github.com/Hwichang/Contact-adjusted-immunity-levels-against-COVID-19-in-South-Korea.
First, we calculated cumulative contact-adjusted immunity levels based on the reported age-specific incidence and vaccination proportion at present. Further, we explored future options to achieve herd immunity levels with age-varying immunity scenarios.
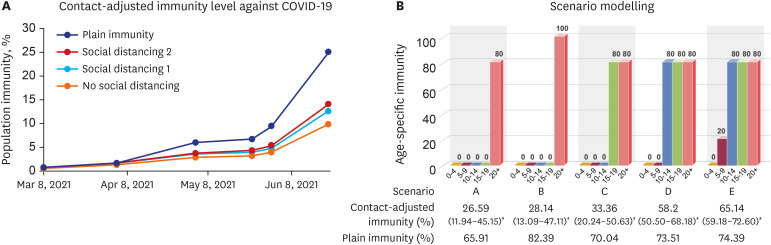
The contact matrices of original (no social distancing), social distancing level 1, and 2 are presented in Fig. 1. The contact-adjusted immunity level estimated based on both COVID-19 incidence and vaccination data under different social distancing policies are shown in Fig. 2A. As of June 21, 2021, when a quarter of the population had received at least one dose of a COVID-19 vaccine, the contact-adjusted immunity level reached 12.5% under social distancing level 1 (14.1% under social distancing level 2).
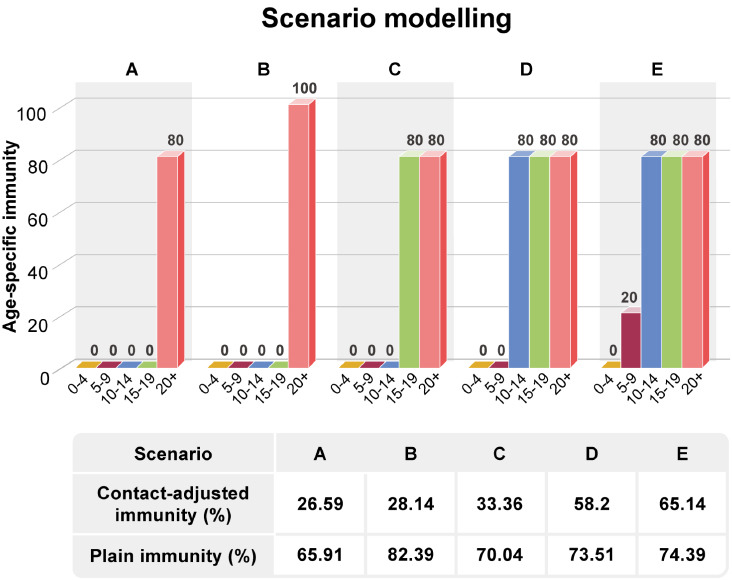
Currently, authorized COVID-19 vaccines in South Korea have been scheduled for individuals 18 years and over. In that, we explored how far the population immunity could reach when most of the population aged 20 years and over gained immunity against SARS-CoV-2. Since we expect normal life to resume as in the pre-COVID-19 era once sufficient people are vaccinated, we applied the original contact matrix to calculate the contact-adjusted population immunity. Even if we achieve 100% immunity for everyone aged 20 years and over, the contact-adjusted immunity would be 28.1%, which is less than the expected herd immunity threshold. When 80% of individuals aged 10 years and over gained immunity, we could achieve a 58.2% contact-adjusted immunity level (Fig. 2B). Various scenarios to attain higher immunity levels are shown in Supplementary Fig. 1.
In this study, we present contact-adjusted immunity levels against SARS-CoV-2 in South Korea, as the vaccinated population increases. Contact numbers in school-aged children are greater than for most other age groups, and an elderly-oriented vaccination strategy is thus less likely to achieve the herd immunity threshold.
Herd immunity, however, is not a fixed level. It theoretically depends on the R0 without any intervention, but it can be changed by the effective reproduction number (Re) at a specific time and place. If strict social distancing measures are applied and the Re drops below 1, there is no need for herd immunity to suppress the outbreak since it will fade away by itself. In contrast, if the R0 of variants is higher than the original virus, herd immunity is unlikely to be achieved.
To reach the theoretical herd immunity against SARS-CoV-2, it appears that the immunity of those aged 10- to 19-years is important. Nonetheless, the risks of COVID-19 for children are much less than that for the elderly, and the long-term safety of mRNA and viral vector vaccines, both delivering genetic materials into the host, is yet to be elucidated. There are reports of myocarditis and pericarditis following mRNA vaccines, particularly in adolescents and young adults in the United States, and thrombosis after viral vector vaccines again in younger adults in Europe.192021
Given that the clinical impact of COVID-19 is particularly harmful to the elderly, and there are still safety issues in the young, it is time to weigh up the pros and cons of vaccinating younger age groups. These groups have the highest contact numbers, and herd immunity may not be achieved without including them but vaccinating the most vulnerable elderly might be enough to restore the normality. Indeed, the United Kingdom (UK) announced zero coronavirus deaths on June 1, 2021, since the pandemic began.22 The UK has one of the world's highest vaccination rates, and it also maintains the elderly-prioritized vaccination strategy.
There are some limitations in this study. First, the employed contact matrix is not of our own empirical data, but of mathematically estimated one. Furthermore, although we tried to modify this original (pre-pandemic) contact matrix to apply social distancing measures, it might be insufficient to reflect reality. Nonetheless, the employed matrix in this study shows an age-assortative mixing pattern that is similar to the age-specific transmission matrix in South Korea.23 Establishing a South Korean contact matrix may improve the accuracy of our analysis. Second, we could not take into account the individual variation in transmissibility such as a super-spreading event, which is a notable feature of SARS-CoV-2. Hence, the estimates driven here might not be convincing. Third, we regard the confirmed COVID-19 case numbers as real case numbers since the case fatality ratio is close to the reference and the latest national seroprevalence of SARS-CoV-2 antibodies was 0.27% as in May 2021.5 However, this assumption might not be accurate. Lastly, we did not account for the waning of vaccine-induced immunity in this study.
Here, we presented contact-adjusted population immunity against SARS-CoV-2 in South Korea. We believe that this is the first report of contact-adjusted immunity against SARS-CoV-2 using national seroprevalence data, vaccine uptake rates, and an age-specific contact matrix. Further, we propose target age-specific immunity levels required to reach the herd immunity. The theoretical herd immunity threshold might not be attainable, but we might be able to restore the normalcy with vaccinating the vulnerable population, especially the elderly.
ACKNOWLEDGMENTS
The graphic work was supported by the Creative Media Service in National Cancer Center Korea.
Notes
Funding: This work was supported by the National Research Foundation of Korea (NRF) grants funded by the Korea government (MSIT) (No. 2020R1A2C3A01003550) and (No. 2021R1F1A1064473).
Author Contributions:
Conceptualization: Chun JY, Kim Y.
Data curation: Jeong H.
Funding acquisition: Chun JY, Kim Y.
Investigation: Jeong H, Kim Y.
Methodology: Chun JY, Jeong H.
Supervision: Kim Y.
Visualization: Chun JY.
Writing - original draft: Chun JY, Jeong H, Kim Y.
Writing - review & editing: Chun JY, Jeong H, Kim Y.
References
1. World Health Organization. WHO coronavirus (COVID-19) dashboard. Updated 2021. Accessed June 26, 2021. https://covid19.who.int/.
2. World Health Organization. COVID-19 virtual press conference transcript - 12 October 2020. Updated 2020. Accessed July 3, 2021. https://www.who.int/publications/m/item/covid-19-virtual-press-conference-transcript---12-October-2020.
3. Ryu S, Ali ST, Jang C, Kim B, Cowling BJ. Effect of nonpharmaceutical interventions on transmission of severe acute respiratory syndrome coronavirus 2, South Korea, 2020. Emerg Infect Dis. 2020; 26(10):2406–2410. PMID: 32487283.

4. Ministry of Health and Welfare (KR). Coronavirus disease-19, Republic of Korea. Updated 2021. Accessed June 26, 2021. http://ncov.mohw.go.kr/.
5. Brazeau N, Verity R, Jenks S, Fu H, Whittaker C, Winskill P, et al. Report 34: COVID-19 infection fatality ratio: estimates from seroprevalence. Updated 2020. Accessed June 28, 2021. https://www.imperial.ac.uk/media/imperial-college/medicine/mrc-gida/2020-10-29-COVID19-Report-34.pdf.
6. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020; 382(13):1199–1207. PMID: 31995857.

7. Petersen E, Koopmans M, Go U, Hamer DH, Petrosillo N, Castelli F, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis. 2020; 20(9):e238–e244. PMID: 32628905.

8. Park SW, Bolker BM, Champredon D, Earn DJ, Li M, Weitz JS, et al. Reconciling early-outbreak estimates of the basic reproductive number and its uncertainty: framework and applications to the novel coronavirus (SARS-CoV-2) outbreak. J R Soc Interface. 2020; 17(168):20200144. PMID: 32693748.

9. Funk S, Knapp JK, Lebo E, Reef SE, Dabbagh AJ, Kretsinger K, et al. Combining serological and contact data to derive target immunity levels for achieving and maintaining measles elimination. BMC Med. 2019; 17(1):180. PMID: 31551070.

10. Korea Disease Control and Prevention Agency. Press release: Korea COVID-19 update. Updated 2021. Accessed June 26, 2021. http://www.kdca.go.kr/board/board.es?mid=a20501000000&bid=0015&list_no=713774&act=view.
12. Sadoff J, Gray G, Vandebosch A, Cárdenas V, Shukarev G, Grinsztejn B, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against COVID-19. N Engl J Med. 2021; 384(23):2187–2201. PMID: 33882225.

13. Prem K, Zandvoort KV, Klepac P, Eggo RM, Davies NG, Cook AR, et al. Projecting contact matrices in 177 geographical regions: an update and comparison with empirical data for the COVID-19 era. PLOS Comput Biol. 2021; 17(7):e1009098. PMID: 34310590.

14. Ministry of Education (KR). Remote learning and school opening information. Updated 2021. Accessed June 26, 2021. https://www.moe.go.kr/sub/info.do?m=580201&page=580201&num=02&s=moe.
15. Google. COVID-19 community mobility reports. Updated 2021. Accessed June 26, 2021. https://www.google.com/covid19/mobility/.
16. Korean Statistical Information Service. Population projection for Korea. Updated 2021. Accessed June 26, 2021. https://kosis.kr/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ZTITLE&parmTabId=M_01_01#SelectStatsBoxDiv.
17. Chun JY, Park WB, Kim NJ, Choi EH, Funk S, Oh MD. Estimating contact-adjusted immunity levels against measles in South Korea and prospects for maintaining elimination status. Vaccine. 2020; 38(2):107–111. PMID: 31679860.

18. Chun JY, Jeong H, Beutels P, Ohmagari N, Kim Y, Tsuzuki S. COVID-19 vaccine prioritisation in Japan and South Korea. medRxiv.

19. Wise J. COVID-19: Should we be worried about reports of myocarditis and pericarditis after mRNA vaccines? BMJ. 2021; 373:n1635. PMID: 34167952.

20. Centers for Disease Control and Prevention. Safety of COVID-19 vaccines. Updated 2021. Accessed June 28, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/myocarditis.html.
22. Public Health England. Coronavirus (COVID-19) in the UK. Updated 2021. Accessed July 1, 2021. https://coronavirus.data.gov.uk/.
23. Ryu S, Ali ST, Noh E, Kim D, Lau EH, Cowling BJ. Transmission dynamics and control of two epidemic waves of SARS-CoV-2 in South Korea. BMC Infect Dis. 2021; 21(1):485. PMID: 34039296.

SUPPLEMENTARY MATERIAL
Supplementary Fig. 1
Various scenario modelling of contact-adjusted immunity level against coronavirus disease 2019 through raising immunity of each age group.
Fig. 1
Age-specific contact patterns in South Korea under the different social distancing measures.13
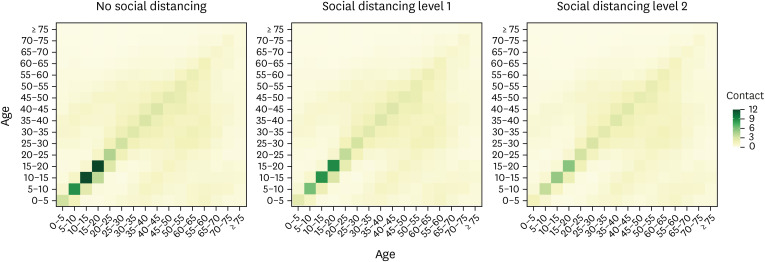
Fig. 2
Contact-adjusted immunity level against COVID-19 (A) based on the reported age-specific incidence and vaccine uptake rates under the various social distancing measures, and (B) scenario modelling through raising immunity of each age group. Plain immunity was calculated by overall proportion of the population immune.
COVID-19 = coronavirus disease 2019.
*In sensitivity analysis, the lowest value is drawn if there are 1.2 times contacts for age groups under 20 (< 20 years) and 0.8 times contacts for age groups 20 years and over (≥ 20 years); and the highest is drawn if there are 0.8 times contacts for < 20 years groups and 1.2 times contacts for ≥ 20 years groups.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download