1. Fagherazzi G, Goetzinger C, Rashid MA, Aguayo GA, Huiart L. Digital health strategies to fight COVID-19 worldwide: challenges, recommendations, and a call for papers. J Med Internet Res. 2020; 22(6):e19284. PMID:
32501804.

2. Kim HS. Lessons from temporary telemedicine initiated owing to outbreak of COVID-19. Healthc Inform Res. 2020; 26(2):159–161. PMID:
32547813.

3. Sharma A, Harrington RA, McClellan MB, Turakhia MP, Eapen ZJ, Steinhubl S, et al. Using digital health technology to better generate evidence and deliver evidence-based care. J Am Coll Cardiol. 2018; 71(23):2680–2690. PMID:
29880129.
4. Kim HS, Yoon KH. Lessons from use of continuous glucose monitoring systems in digital healthcare. Endocrinol Metab (Seoul). 2020; 35(3):541–548. PMID:
32981296.

5. Dunn P, Hazzard E. Technology approaches to digital health literacy. Int J Cardiol. 2019; 293:294–296. PMID:
31350037.

6. Kim HS, Cho JH, Yoon KH. New directions in chronic disease management. Endocrinol Metab (Seoul). 2015; 30(2):159–166. PMID:
26194075.

7. Kim HS, Lee KH, Kim H, Kim JH. Using mobile phones in healthcare management for the elderly. Maturitas. 2014; 79(4):381–388. PMID:
25270725.

8. Godfrey A, Goldsack JC, Tenaerts P, Coravos A, Aranda C, Hussain A, et al. BioMeT and algorithm challenges: a proposed digital standardized evaluation framework. IEEE J Transl Eng Health Med. 2020; 8:0700108. PMID:
32542118.

9. Rockwern B, Johnson D, Snyder Sulmasy L. Medical Informatics Committee and Ethics, Professionalism and Human Rights Committee of the American College of Physicians. Health information privacy, protection, and use in the expanding digital health ecosystem: a position paper of the American College of Physicians. Ann Intern Med. 2021; 174(7):994–998. PMID:
33900797.

10. Sim I. Mobile devices and health. N Engl J Med. 2019; 381(10):956–968. PMID:
31483966.

11. Kim HS, Kim DJ, Yoon KH. Medical big data is not yet available: why we need realism rather than exaggeration. Endocrinol Metab (Seoul). 2019; 34(4):349–354. PMID:
31884734.

12. Maeder A, Poultney N, Morgan G, Lippiatt R. Patient compliance in home-based self-care telehealth projects. J Telemed Telecare. 2015; 21(8):439–442. PMID:
26556057.

13. Blakey JD, Bender BG, Dima AL, Weinman J, Safioti G, Costello RW. Digital technologies and adherence in respiratory diseases: the road ahead. Eur Respir J. 2018; 52(5):1801147. PMID:
30409819.

14. Bhavnani SP, Narula J, Sengupta PP. Mobile technology and the digitization of healthcare. Eur Heart J. 2016; 37(18):1428–1438. PMID:
26873093.

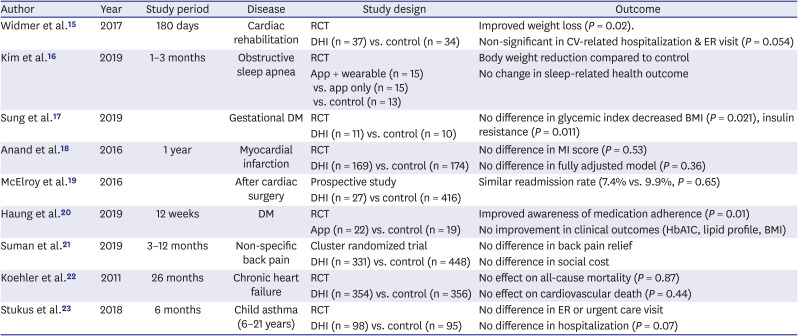
15. Widmer RJ, Allison TG, Lennon R, Lopez-Jimenez F, Lerman LO, Lerman A. Digital health intervention during cardiac rehabilitation: a randomized controlled trial. Am Heart J. 2017; 188:65–72. PMID:
28577682.

16. Kim JW, Ryu B, Cho S, Heo E, Kim Y, Lee J, et al. Impact of personal health records and wearables on health outcomes and patient response: three-arm randomized controlled trial. JMIR Mhealth Uhealth. 2019; 7(1):e12070. PMID:
30609978.

17. Sung JH, Lee DY, Min KP, Park CY. Peripartum management of gestational diabetes using a digital health care service: a pilot, randomized controlled study. Clin Ther. 2019; 41(11):2426–2434. PMID:
31587813.

18. Anand SS, Samaan Z, Middleton C, Irvine J, Desai D, Schulze KM, et al. A digital health intervention to lower cardiovascular risk: a randomized clinical trial. JAMA Cardiol. 2016; 1(5):601–606. PMID:
27438754.
19. McElroy I, Sareh S, Zhu A, Miranda G, Wu H, Nguyen M, et al. Use of digital health kits to reduce readmission after cardiac surgery. J Surg Res. 2016; 204(1):1–7. PMID:
27451860.

20. Huang Z, Tan E, Lum E, Sloot P, Boehm BO, Car J. A smartphone app to improve medication adherence in patients with type 2 diabetes in Asia: feasibility randomized controlled trial. JMIR Mhealth Uhealth. 2019; 7(9):e14914. PMID:
31516127.

21. Suman A, Schaafsma FG, van Dongen JM, Elders PJ, Buchbinder R, van Tulder MW, et al. Effectiveness and cost-utility of a multifaceted eHealth strategy to improve back pain beliefs of patients with non-specific low back pain: a cluster randomised trial. BMJ Open. 2019; 9(12):e030879.

22. Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Böhm M, et al. Impact of remote telemedical management on mortality and hospitalizations in ambulatory patients with chronic heart failure: the telemedical interventional monitoring in heart failure study. Circulation. 2011; 123(17):1873–1880. PMID:
21444883.
23. Stukus DR, Farooqui N, Strothman K, Ryan K, Zhao S, Stevens JH, et al. Real-world evaluation of a mobile health application in children with asthma. Ann Allergy Asthma Immunol. 2018; 120(4):395–400.e1. PMID:
29452259.

24. Kim HS, Hwang Y, Lee JH, Oh HY, Kim YJ, Kwon HY, et al. Future prospects of health management systems using cellular phones. Telemed J E Health. 2014; 20(6):544–551. PMID:
24693986.

25. Kim HS, Jeong YJ, Baik SJ, Yang SJ, Kim TM, Kim H, et al. Social networking services-based communicative care for patients with diabetes mellitus in Korea. Appl Clin Inform. 2016; 7(3):899–911. PMID:
27679839.

26. Kim HS, Choi W, Baek EK, Kim YA, Yang SJ, Choi IY, et al. Efficacy of the smartphone-based glucose management application stratified by user satisfaction. Diabetes Metab J. 2014; 38(3):204–210. PMID:
25003074.

27. Lu L, Zhang J, Xie Y, Gao F, Xu S, Wu X, et al. Wearable health devices in health care: narrative systematic review. JMIR Mhealth Uhealth. 2020; 8(11):e18907. PMID:
33164904.

28. Ferguson CM. Chapter 93. Inspection, auscultation, palpation, and percussion of the abdomen. Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, UK: Butterworths;1990. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK420/.
29. Yeston NS. Inspection, palpation, percussion, and auscultation = connection. Conn Med. 2002; 66(12):757–758. PMID:
12532611.
30. Nittas V, Lun P, Ehrler F, Puhan MA, Mütsch M. Electronic patient-generated health data to facilitate disease prevention and health promotion: scoping review. J Med Internet Res. 2019; 21(10):e13320. PMID:
31613225.

31. Kim HS. Apprehensions about excessive belief in digital therapeutics: points of concern excluding merits. J Korean Med Sci. 2020; 35(45):e373. PMID:
33230984.

32. Kim SK, Kim HJ, Kim T, Hur KY, Kim SW, Lee MK, et al. Effectiveness of 3-day continuous glucose monitoring for improving glucose control in type 2 diabetic patients in clinical practice. Diabetes Metab J. 2014; 38(6):449–455. PMID:
25541608.

33. Cappon G, Vettoretti M, Sparacino G, Facchinetti A. Continuous glucose monitoring sensors for diabetes management: a review of technologies and applications. Diabetes Metab J. 2019; 43(4):383–397. PMID:
31441246.

34. Kim HS, Shin JA, Chang JS, Cho JH, Son HY, Yoon KH. Continuous glucose monitoring: current clinical use. Diabetes Metab Res Rev. 2012; 28(Suppl 2):73–78. PMID:
23280870.

35. Lee SK, Shin DH, Kim YH, Lee KS. Effect of diabetes education through pattern management on self-care and self-efficacy in patients with type 2 diabetes. Int J Environ Res Public Health. 2019; 16(18):3323.

36. Kim HS, Kim H, Lee S, Lee KH, Kim JH. Current clinical status of telehealth in Korea: categories, scientific basis, and obstacles. Healthc Inform Res. 2015; 21(4):244–250. PMID:
26618030.

37. Lee J, Kim HS, Kim JE. Out-of-hospital data: patient generated health data. J Korean Diabetes. 2020; 21(3):149–155.

38. Codella J, Partovian C, Chang HY, Chen CH. Data quality challenges for person-generated health and wellness data. IBM J Res Develop. 2018; 62(1):3:1–3:8.

39. Abdolkhani R, Borda A, Gray K. Quality management of patient generated health data in remote patient monitoring using medical wearables- a systematic review. Stud Health Technol Inform. 2018; 252:1–7. PMID:
30040674.
40. Saravanakumar NM, Eswari T, Sampath P, Lavanya S. Predictive methodology for diabetic data analysis in big data. Procedia Comput Sci. 2015; 50:203–208.
41. Purswani JM, Dicker AP, Champ CE, Cantor M, Ohri N. Big data from small devices: the future of smartphones in oncology. Semin Radiat Oncol. 2019; 29(4):338–347. PMID:
31472736.

42. Lee J, Kim HS, Kim DJ. Recent technology-driven advancements in cardiovascular disease prevention. Cardiovasc Prev Pharmacother. 2019; 1(2):43–49.
43. Jung SH, Kang IK, Park CY, Ryu MS, Woo JT, Kim SW, et al. Continuous glucose monitoring is needed to detect unrecognized hypoglycemic event in diabetic patients with stroke. Diabetes Monit. 2002; 3(2):140–151.
44. Smith B, Magnani JW. New technologies, new disparities: The intersection of electronic health and digital health literacy. Int J Cardiol. 2019; 292:280–282. PMID:
31171391.

45. Greaves F, Joshi I, Campbell M, Roberts S, Patel N, Powell J. What is an appropriate level of evidence for a digital health intervention? Lancet. 2019; 392(10165):2665–2667. PMID:
30545779.

46. Melstrom LG, Rodin AS, Rossi LA, Fu P Jr, Fong Y, Sun V. Patient generated health data and electronic health record integration in oncologic surgery: a call for artificial intelligence and machine learning. J Surg Oncol. 2021; 123(1):52–60. PMID:
32974930.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download