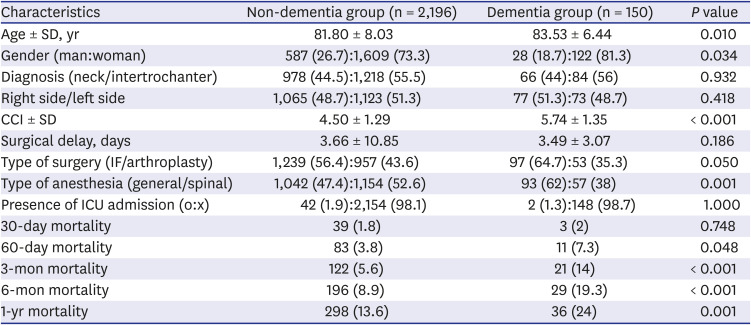
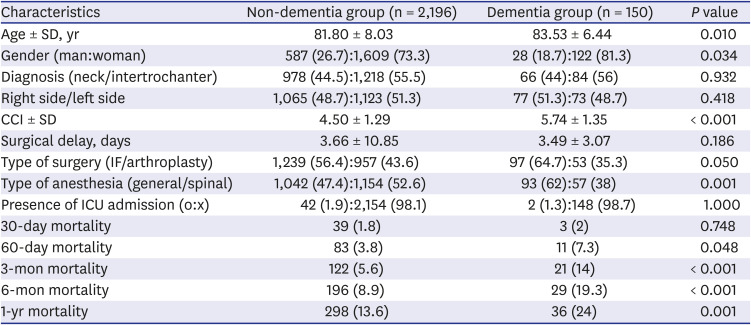
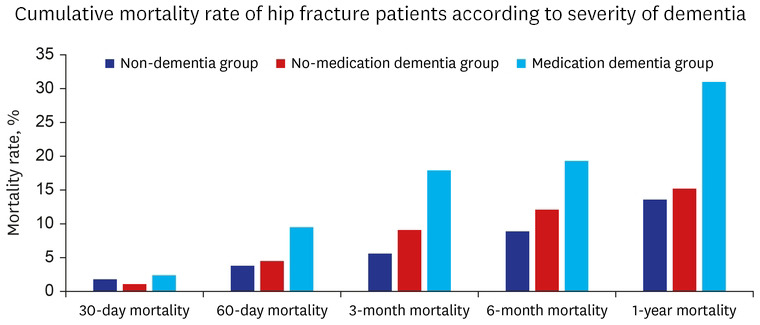
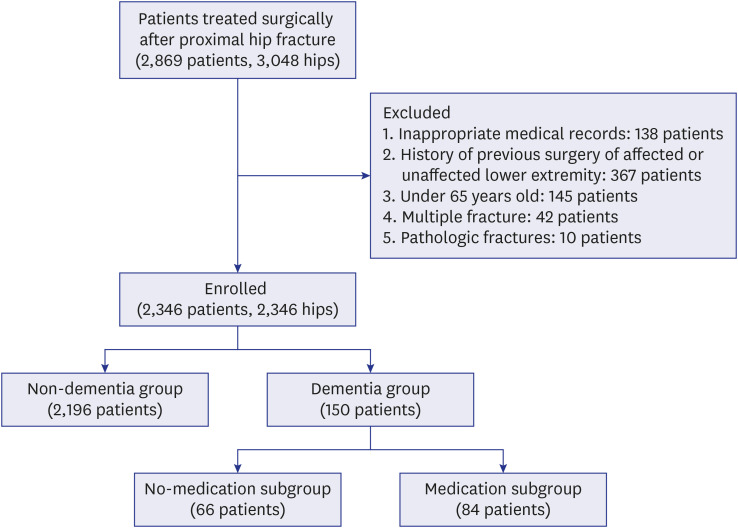
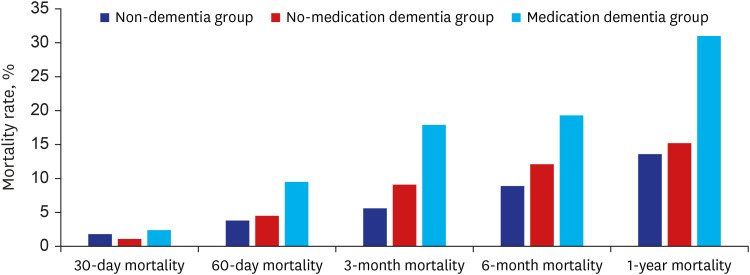
Of the 2,346 patients with hip fractures, 150 (6.4%) patients were diagnosed with dementia. The 30-day, 60-day, 3-month, 6-month, and 1-year postoperative cumulative mortality rates were 1.8%, 3.8%, 5.6%, 8.9%, and 13.6%, respectively, in the non-dementia group, and 2%, 7.3%, 14%, 19.3%, and 24%, respectively, in the dementia group (
Table 1,
Fig. 2). The dementia group was older (
P = 0.010), had a higher proportion of women (
P = 0.034), worse CCI (
P < 0.001), and higher prevalence of general anesthesia (
P = 0.001).
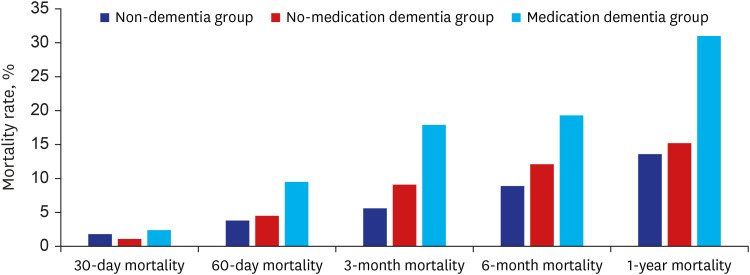 | Fig. 2 The graph shows the mortality rates of each group.
|
Table 1
Summary of characteristics between non-dementia and dementia groups
|
Characteristics |
Non-dementia group (n = 2,196) |
Dementia group (n = 150) |
P value |
|
Age ± SD, yr |
81.80 ± 8.03 |
83.53 ± 6.44 |
0.010 |
|
Gender (man:woman) |
587 (26.7):1,609 (73.3) |
28 (18.7):122 (81.3) |
0.034 |
|
Diagnosis (neck/intertrochanter) |
978 (44.5):1,218 (55.5) |
66 (44):84 (56) |
0.932 |
|
Right side/left side |
1,065 (48.7):1,123 (51.3) |
77 (51.3):73 (48.7) |
0.418 |
|
CCI ± SD |
4.50 ± 1.29 |
5.74 ± 1.35 |
< 0.001 |
|
Surgical delay, days |
3.66 ± 10.85 |
3.49 ± 3.07 |
0.186 |
|
Type of surgery (IF/arthroplasty) |
1,239 (56.4):957 (43.6) |
97 (64.7):53 (35.3) |
0.050 |
|
Type of anesthesia (general/spinal) |
1,042 (47.4):1,154 (52.6) |
93 (62):57 (38) |
0.001 |
|
Presence of ICU admission (o:x) |
42 (1.9):2,154 (98.1) |
2 (1.3):148 (98.7) |
1.000 |
|
30-day mortality |
39 (1.8) |
3 (2) |
0.748 |
|
60-day mortality |
83 (3.8) |
11 (7.3) |
0.048 |
|
3-mon mortality |
122 (5.6) |
21 (14) |
< 0.001 |
|
6-mon mortality |
196 (8.9) |
29 (19.3) |
< 0.001 |
|
1-yr mortality |
298 (13.6) |
36 (24) |
0.001 |

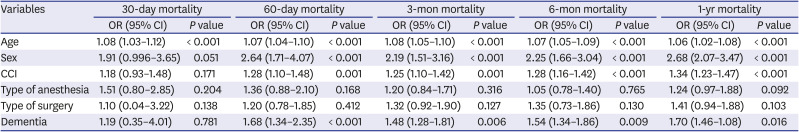
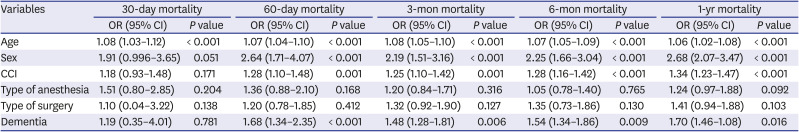
To analyze the risk factors for the 30-day, 60-day, 3-month, 6-month, and 1-year mortality in elderly patients with hip fractures, multivariable logistic regression was performed (
Table 2). Age (odds ratio [OR], 1.08; 95% confidence interval [CI], 1.03–1.12;
P < 0.001) was identified as a factor that affected the 30-day mortality, and age (OR, 1.07; 95% CI, 1.04–1.10;
P < 0.001), sex (OR, 2.64; 95% CI, 1.71–4.07;
P < 0.001), CCI (OR, 1.28; 95% CI, 1.10–1.48;
P = 0.001), and dementia (OR, 1.68; 95% CI, 1.34–2.35;
P < 0.001) were identified as factors that affected the 60-day mortality. The factors that affected the 3-month mortality were age (OR, 1.08; 95% CI, 1.05–1.10;
P < 0.001), sex (OR, 2.19; 95% CI, 1.51–3.16;
P < 0.001), CCI (OR, 1.25; 95% CI, 1.10–1.42;
P = 0.001), and dementia (OR, 1.48; 95% CI, 1.28–1.81;
P = 0.006). The factors that affected the 6-month mortality were age (OR, 1.07; 95% CI, 1.05–1.09;
P < 0.001), sex (OR, 2.25; 95% CI, 1.66–3.04;
P < 0.001), CCI (OR, 1.28; 95% CI, 1.16–1.42;
P < 0.001), and dementia (OR, 1.54; 95% CI, 1.34–1.86;
P = 0.009). The factors that affected the 1-year mortality were age (OR, 1.06; 95% CI, 1.02–1.08;
P < 0.001), sex (OR, 2.68; 95% CI, 2.07–3.47;
P < 0.001), CCI (OR, 1.34; 95% CI, 1.23–1.47;
P < 0.001), and dementia (OR, 1.70; 95% CI, 1.46–1.08;
P = 0.016).
Table 2
Risk factors affecting postoperative mortality in elderly hip fracture patients
|
Variables |
30-day mortality |
60-day mortality |
3-mon mortality |
6-mon mortality |
1-yr mortality |
|
OR (95% CI) |
P value |
OR (95% CI) |
P value |
OR (95% CI) |
P value |
OR (95% CI) |
P value |
OR (95% CI) |
P value |
|
Age |
1.08 (1.03–1.12) |
< 0.001 |
1.07 (1.04–1.10) |
< 0.001 |
1.08 (1.05–1.10) |
< 0.001 |
1.07 (1.05–1.09) |
< 0.001 |
1.06 (1.02–1.08) |
< 0.001 |
|
Sex |
1.91 (0.996–3.65) |
0.051 |
2.64 (1.71–4.07) |
< 0.001 |
2.19 (1.51–3.16) |
< 0.001 |
2.25 (1.66–3.04) |
< 0.001 |
2.68 (2.07–3.47) |
< 0.001 |
|
CCI |
1.18 (0.93–1.48) |
0.171 |
1.28 (1.10–1.48) |
0.001 |
1.25 (1.10–1.42) |
0.001 |
1.28 (1.16–1.42) |
< 0.001 |
1.34 (1.23–1.47) |
< 0.001 |
|
Type of anesthesia |
1.51 (0.80–2.85) |
0.204 |
1.36 (0.88–2.10) |
0.168 |
1.20 (0.84–1.71) |
0.316 |
1.05 (0.78–1.40) |
0.765 |
1.24 (0.97–1.88) |
0.092 |
|
Type of surgery |
1.10 (0.04–3.22) |
0.138 |
1.20 (0.78–1.85) |
0.412 |
1.32 (0.92–1.90) |
0.127 |
1.35 (0.73–1.86) |
0.130 |
1.41 (0.94–1.88) |
0.103 |
|
Dementia |
1.19 (0.35–4.01) |
0.781 |
1.68 (1.34–2.35) |
< 0.001 |
1.48 (1.28–1.81) |
0.006 |
1.54 (1.34–1.86) |
0.009 |
1.70 (1.46–1.08) |
0.016 |

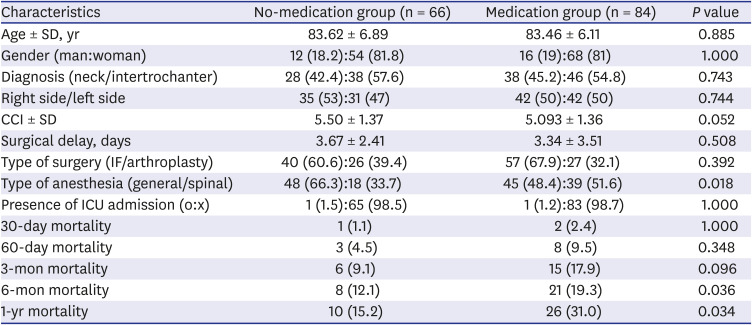
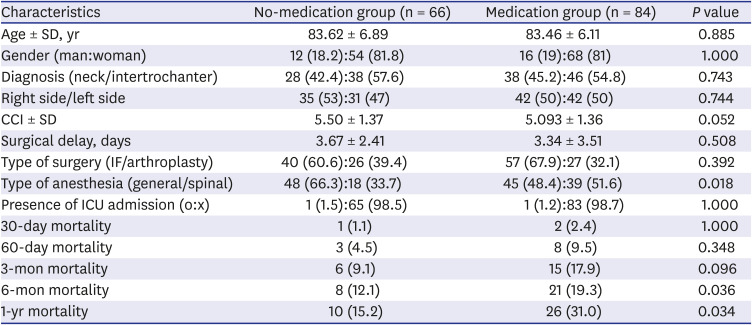
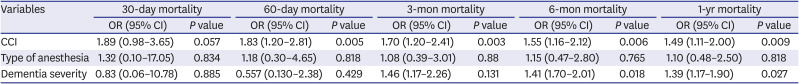
In the subgroup analysis, among the 150 patients with dementia, the 30-day and 60-day, 3-month, 6-month, and 1-year postoperative cumulative mortality rates were 1.1%, 4.5%, 9.1%, 12.1%, and 15.2%, respectively, in the no-medication subgroup (66 patients), and 2.4%, 9.5%, 17.9%, 19.3%, and 31%, respectively, in the medication subgroup (84 patients) (
Table 3,
Fig. 2).
Table 3
Summary of characteristics of dementia patients in the no-medication group and medication group
|
Characteristics |
No-medication group (n = 66) |
Medication group (n = 84) |
P value |
|
Age ± SD, yr |
83.62 ± 6.89 |
83.46 ± 6.11 |
0.885 |
|
Gender (man:woman) |
12 (18.2):54 (81.8) |
16 (19):68 (81) |
1.000 |
|
Diagnosis (neck/intertrochanter) |
28 (42.4):38 (57.6) |
38 (45.2):46 (54.8) |
0.743 |
|
Right side/left side |
35 (53):31 (47) |
42 (50):42 (50) |
0.744 |
|
CCI ± SD |
5.50 ± 1.37 |
5.093 ± 1.36 |
0.052 |
|
Surgical delay, days |
3.67 ± 2.41 |
3.34 ± 3.51 |
0.508 |
|
Type of surgery (IF/arthroplasty) |
40 (60.6):26 (39.4) |
57 (67.9):27 (32.1) |
0.392 |
|
Type of anesthesia (general/spinal) |
48 (66.3):18 (33.7) |
45 (48.4):39 (51.6) |
0.018 |
|
Presence of ICU admission (o:x) |
1 (1.5):65 (98.5) |
1 (1.2):83 (98.7) |
1.000 |
|
30-day mortality |
1 (1.1) |
2 (2.4) |
1.000 |
|
60-day mortality |
3 (4.5) |
8 (9.5) |
0.348 |
|
3-mon mortality |
6 (9.1) |
15 (17.9) |
0.096 |
|
6-mon mortality |
8 (12.1) |
21 (19.3) |
0.036 |
|
1-yr mortality |
10 (15.2) |
26 (31.0) |
0.034 |





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download