1. Jung CH, Son JW, Kang S, Kim WJ, Kim HS, Kim HS, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J. 2021; 45(1):1–10. PMID:
33434426.

2. Kim BY, Won JC, Lee JH, Kim HS, Park JH, Ha KH, et al. Diabetes fact sheets in Korea, 2018: an appraisal of current status. Diabetes Metab J. 2019; 43(4):487–494. PMID:
31339012.

3. White JR Jr. A brief history of the development of diabetes medications. Diabetes Spectr. 2014; 27(2):82–86. PMID:
26246763.

4. Giugliano D, Longo M, Maiorino MI, Bellastella G, Chiodini P, Solerte SB, et al. Efficacy of SGLT-2 inhibitors in older adults with diabetes: systematic review with meta-analysis of cardiovascular outcome trials. Diabetes Res Clin Pract. 2020; 162:108114. PMID:
32165164.

5. Kristensen SL, Rørth R, Jhund PS, Docherty KF, Sattar N, Preiss D, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 2019; 7(10):776–785. PMID:
31422062.

6. Kim MK, Ko SH, Kim BY, Kang ES, Noh J, Kim SK, et al. 2019 clinical practice guidelines for type 2 diabetes mellitus in Korea. Diabetes Metab J. 2019; 43(4):398–406. PMID:
31441247.

7. American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: Standards of medical care in diabetes-2021. Diabetes Care. 2021; 44(Suppl 1):S111–S124. PMID:
33298420.
8. Bang C, Mortensen MB, Lauridsen KG, Bruun JM. Trends in antidiabetic drug utilization and expenditure in Denmark: a 22-year nationwide study. Diabetes Obes Metab. 2020; 22(2):167–172. PMID:
31486269.

9. Ko SH, Kim DJ, Park JH, Park CY, Jung CH, Kwon HS, et al. Trends of antidiabetic drug use in adult type 2 diabetes in Korea in 2002–2013: nationwide population-based cohort study. Medicine (Baltimore). 2016; 95(27):e4018. PMID:
27399082.
10. Hripcsak G, Duke JD, Shah NH, Reich CG, Huser V, Schuemie MJ, et al. Observational Health Data Sciences and Informatics (OHDSI): opportunities for observational researchers. Stud Health Technol Inform. 2015; 216:574–578. PMID:
26262116.
11. Jeon Y, Choi Y, Kim EH, Oh S, Lee H. Common data model-based real-world data for practical clinical practice guidelines: clinical pharmacology perspectives. Transl Clin Pharmacol. 2020; 28(2):67–72. PMID:
32656157.

12. Hripcsak G, Ryan PB, Duke JD, Shah NH, Park RW, Huser V, et al. Characterizing treatment pathways at scale using the OHDSI network. Proc Natl Acad Sci U S A. 2016; 113(27):7329–7336. PMID:
27274072.

13. Kim H, Yoo S, Jeon Y, Yi S, Kim S, Choi SA, et al. Characterization of anti-seizure medication treatment pathways in pediatric epilepsy using the electronic health record-based common data model. Front Neurol. 2020; 11:409. PMID:
32477256.

14. Zhang X, Wang L, Miao S, Xu H, Yin Y, Zhu Y, et al. Analysis of treatment pathways for three chronic diseases using OMOP CDM. J Med Syst. 2018; 42(12):260. PMID:
30421323.

15. Yoon D, Ahn EK, Park MY, Cho SY, Ryan P, Schuemie MJ, et al. Conversion and data quality assessment of electronic health record data at a Korean tertiary teaching hospital to a common data model for distributed network research. Healthc Inform Res. 2016; 22(1):54–58. PMID:
26893951.

16. Won JC, Lee JH, Kim JH, Kang ES, Won KC, Kim DJ, et al. Diabetes fact sheet in Korea, 2016: an appraisal of current status. Diabetes Metab J. 2018; 42(5):415–424. PMID:
30113146.

17. Cahn A, Cefalu WT. Clinical considerations for use of initial combination therapy in type 2 diabetes. Diabetes Care. 2016; 39(Suppl 2):S137–S145. PMID:
27440826.

19. Karter AJ, Subramanian U, Saha C, Crosson JC, Parker MM, Swain BE, et al. Barriers to insulin initiation: the translating research into action for diabetes insulin starts project. Diabetes Care. 2010; 33(4):733–735. PMID:
20086256.

20. Cho YK, Lee J, Kim HS, Park JY, Jung CH, Lee WJ. Clinical efficacy of quadruple oral therapy for type 2 diabetes in real-world practice: a retrospective observational study. Diabetes Ther. 2020; 11(9):2029–2039. PMID:
32696268.
21. Moon JS, Suh S, Kim SS, Jin HY, Kim JM, Jang MH, et al. Efficacy and safety of treatment with quadruple oral hypoglycemic agents in uncontrolled type 2 diabetes mellitus: a multi-center, retrospective, observational study. Diabetes Metab J. Forthcoming. 2020; DOI:
10.4093/dmj.2020.0107.

22. Grant RW, Wexler DJ, Watson AJ, Lester WT, Cagliero E, Campbell EG, et al. How doctors choose medications to treat type 2 diabetes: a national survey of specialists and academic generalists. Diabetes Care. 2007; 30(6):1448–1453. PMID:
17337497.

23. Ko SH, Kim SR, Kim DJ, Oh SJ, Lee HJ, Shim KH, et al. 2011 clinical practice guidelines for type 2 diabetes in Korea. Diabetes Metab J. 2011; 35(5):431–436. PMID:
22111032.

24. Paolisso G, Monami M, Marfella R, Rizzo MR, Mannucci E. Dipeptidyl peptidase-4 inhibitors in the elderly: more benefits or risks? Adv Ther. 2012; 29(3):218–233. PMID:
22411425.

25. Nelinson DS, Sosa JM, Chilton RJ. SGLT2 inhibitors: a narrative review of efficacy and safety. J Osteopath Med. 2021; 121(2):229–239. PMID:
33567084.

26. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998; 352(9131):854–865. PMID:
9742977.
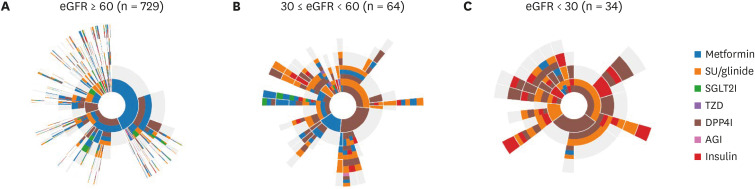
27. U.S. Food and Drug Administration. FDA drug safety communication: FDA revises warnings regarding use of the diabetes medicine metformin in certain patients with reduced kidney function. Updated 2017. Accessed May 12, 2021.
http://www.fda.gov/Drugs/DrugSafety/ucm493244.htm.
28. Hur KY, Kim MK, Ko SH, Han M, Lee DW, Kwon HS, et al. Metformin treatment for patients with diabetes and chronic kidney disease: a Korean Diabetes Association and Korean Society of Nephrology Consensus Statement. Diabetes Metab J. 2020; 44(1):3–10. PMID:
32097995.

29. Gillett MJ. International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009; 32(7):1327–1334. PMID:
19502545.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download