INTRODUCTION
Myocarditis/pericarditis are one of the most serious infectious and/or inflammatory diseases that can result from various etiology, most commonly viral infection,
12 and can also be caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
3
Since the emergence of SARS-CoV-2 at the end of 2019, globally, there have been 181.9 million confirmed cases of coronavirus disease 2019 (COVID-19) and 3.9 million deaths as of June 30, 2021.
4 COVID-19 vaccines were developed with an unprecedented speed in 2020, and as of June 30, 2021, 3.0 billion doses have been vaccinated with one of the emergently authorized vaccines.
4 In South Korea, two viral vector vaccines (AZD1222 [AstraZeneca] and Ad26.COV2.S [Janssen]) and two mRNA vaccines (BNT162b2 [Pfizer-BioNTech] and mRNA-1273 [Moderna]) are authorized for emergency use.
5 As of June 30, 2021, 18.8 million doses of vaccines were given, and 84,839 cases of adverse events were reported mainly for AZD1222 [AstraZeneca] and BNT162b2 [Pfizer-BioNTech] vaccines.
6
Currently, BNT162b2 [Pfizer-BioNTech] vaccine is the only vaccine that has been authorized for use in adolescents 16 years and older in Korea and many other countries. In addition, on May 12, 2021, the U.S. Advisory Committee on Immunization Practices' (ACIP's) interim recommendations for the use of Pfizer-BioNTech COVID-19 vaccine in adolescents aged 12–15 years were issued, and vaccination was performed in children to 12 years of age in the U.S.; 22.1% of adolescents ages 12-15 years has been fully vaccinated as of July 1, 2021.
7 As of June 11, 2021, 4,229,597 doses were given in adolescents aged 12-17 years old and 147 cases of myocarditis/pericarditis were reported (19 cases from 2,189,726 doses given in female, 128 cases from 2,039,871 doses given in male assuming a 7-day post-vaccination observation window).
8 It appears that the risk of developing myocarditis/pericarditis is higher after the second dose.
In Korea, COVID-19 vaccines have not been given to young individuals under the age of 18 years, but the Korean health authority plans to vaccinate adolescents starting high school seniors during the summer vacation of 2021.
9 With this background, there is an urgent need for a review on the epidemiology and clinical manifestations of myocarditis/pericarditis among Korean children. We performed a retrospective study in patients who were hospitalized to two major hospitals in Korea due to myocarditis/pericarditis for 10 years before COVID-19 era.
Go to :

DISCUSSION
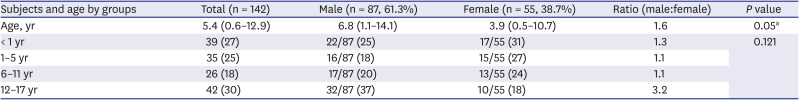
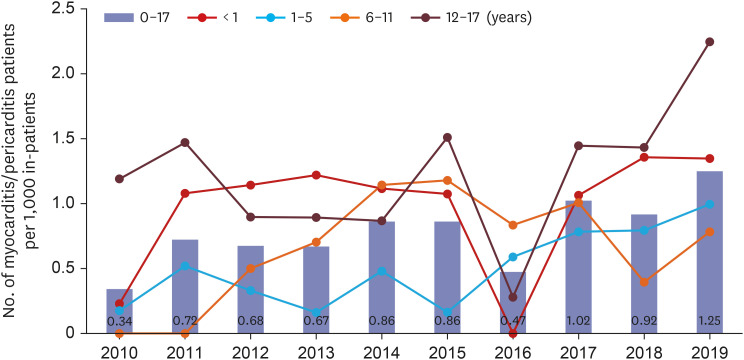
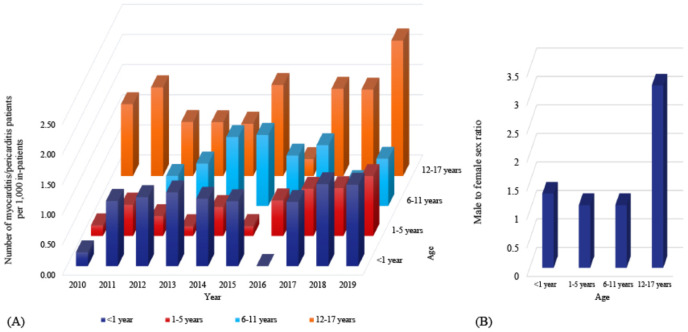
This study investigated the epidemiology, clinical manifestations, and outcome on pediatric patients who were hospitalized due to myocarditis/pericarditis before the COVID-19 era. We observed that myocarditis/pericarditis occur in all ages with a predominance in the male adolescent age group 12–17 years and had favorable outcome without any mortality. In addition, an increasing tendency for the annual frequency of myocarditis/pericarditis was observed during the study period.
During the COVID-19 pandemic, the vaccine has been the most successful measurements to control the outbreak, in addition to social distancing policy. There was a dramatic decrease in the burden of morbidity and mortality of COVID-19 in several countries where the COVID-19 vaccines were rolled out in the adult population early in 2020–2021. However, there have been changes in vaccine recommendation policies such as restricting ages or adding warnings after the reports on thrombosis with thrombocytopenia syndrome following adenovirus vectored COVID-19 vaccination in many countries.
13141516 Although this raised concerns for vaccine safety issues and hesitancy, governments in all countries continued COVID-19 vaccination with careful monitoring for adverse events and assessment of the risks-and-benefit analysis. Following the adults, vaccination in the pediatric population has been the topic for discussion and debate.
After the rolling out the vaccines in adults in Korea, February 2021, COVID-19 vaccines have not been recommended to pediatric population yet as of the end of June 2021, Korea Disease Control and Prevention Agency plans to vaccinate high school seniors during the summer school break in July 2021. However, since the first report on seven adolescents who developed symptomatic acute myocarditis after the BNT162b2 [Pfizer-BioNTech] vaccines in the U.S.,
17 post mRNA COVID-19 vaccination myocarditis has alerted the clinicians and health authorities.
Most of the COVID-19 infections in pediatric population showed mild symptoms and favorable clinical courses, but severe manifestations were observed in some patients with multisystem inflammatory syndrome in children (MIS-C). In the U.S., the cumulative incidence of MIS-C per 100,000 persons aged younger than 21 years was 2.1.
18 On the other hand, as of June 11, 2021, the number of myocarditis/pericarditis reported per 1,000,000 doses of mRNA vaccines was 4.0,
8 which is less common compared to the incidence of MIS-C. However, the incidence of MIS-C in Korea younger than 20 years is lower (only 3 cases were reported to the national surveillance system during seven months of surveillance period, 0.03 per 100,000 persons) than those in the U.S. or Europe.
1920 Moreover, safety issues have been concerned after the initiation of the mRNA vaccine to the pediatric population. The incidence by age should be considered because the incidence of myocarditis after mRNA vaccination was reported up to 66 cases per 1,000,000 doses in 12–17-year-old males.
8 Therefore, the benefits and risks of vaccination and myocarditis/pericarditis should be considered while taking into account differences between region, race, and age.
Myocarditis often results from viral infections that have a predilection for the myocardium that causes unwanted immune-mediated inflammation and eventually myocardial cell dysfunction and reduced contractility.
1 Post-vaccination myocarditis is a known but rare adverse event after other vaccination, such as smallpox or diphtheria, whole-cell pertussis, and tetanus toxoid vaccination (DTP) vaccination.
2122 After smallpox vaccination, myocarditis occurred at a rate of 1 per 12,819 primary vaccinees (or 7.8 per 100,000 persons) among vaccinia naïve U.S. military personnel with mean age 26.5 (20–34 years). The time from vaccination to symptom onset was mean 10.5 days (range, 7–19 days), and all cases were white men.
21 For myocarditis following DTP vaccination, there are only a few case reports, mainly after whole-cell pertussis vaccination, which is not used in Korea or other developed countries where acellular vaccines are used.
The baseline incidences of myocarditis may vary; In Korea, it has been reported to occur in 1.4 per 100,000 children in 2007 and 2.1 per 100,000 children in 2016 from a nationwide Health Insurance Review and Assessment Service Database (claims data of children and adolescents aged ≤ 19 years).
23 It was reported as 1.95 per 100,000 person-year in children < 15 years of age in Finland
24 and 2.16 expected cases per 100,000 U.S. military service members in a 30-day period.
21 Although population-level data from insurance claims may provide a big picture, further detailed data using hospital medical records would still be of interest to clinicians. In this study, data on children who were hospitalized to two major referral hospitals in Korea and present additionally useful and somewhat distinct observations.
In addition, the frequency of myocarditis showed to increase from 0.34 in 2010 to 1.25 in 2019 per 1,000 in-patients in this study. This trend is similar to other studies, and it was difficult to prove the exact cause in this study. However, other studies suggest that the increase in incidence is due to changes in physician's perception of the myocarditis
23 and the development of diagnostic techniques such as cardiac magnetic resonance imaging (MRI).
25
In a study by Kim and Cho,
23 they included only ICD-10 codes for I40, I41, or I51.4, while we included more codes as described in methods. In addition, Kim and Cho
23 combined the data for heart transplantation with deceased patients' data, but we combined the data for heart transplantation with survived patients' data since from clinician's standpoint, heart transplant recipients are still alive. Since we wanted to look at the baseline frequencies of myocarditis/pericarditis data in age groups in which the step-wise COVID-19 vaccination expansion is expected, our age group classification was further divided in children one year and older. The proportion of patients were 27% vs. 25% vs. 18% vs. 30% in four age groups (< 1 year vs. 1–5 years vs. 6–11 years vs. 12–17 years), respectively. It was also noted that in the age group 12–17 years, male predominance was observed. Kim and Cho
23 observed that nearly 50% of cases occurred between January and March, but our study did not show any significant seasonality.
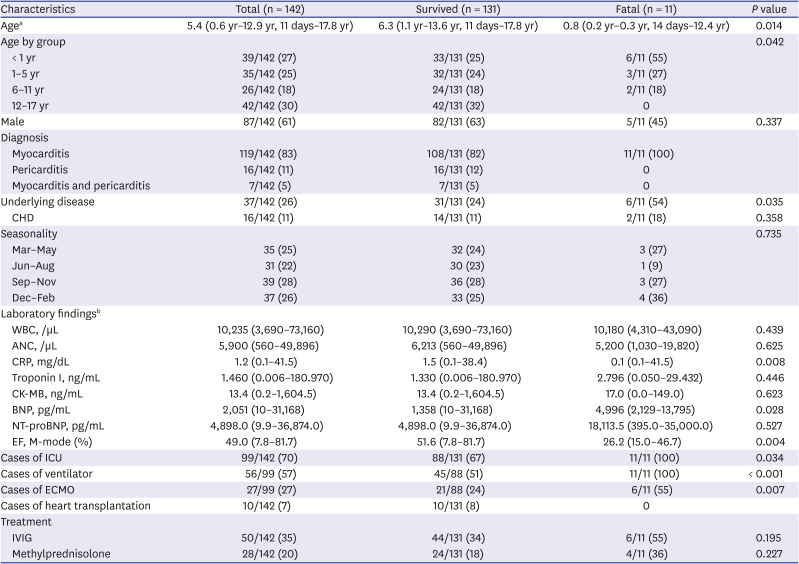
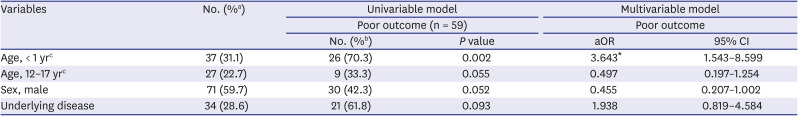
The frequency of myocarditis showed a bimodal trend in infants and adolescents in this study, which was comparable to previous studies on pediatric myocarditis.
2526 In addition, age younger than one year was the risk factor for poor outcome in this present study with higher mortality than other age groups. A multicenter study in the U.S. reported that the death/transplant group had a lower median age than the survived group (7.75 years vs. 14 years).
26 Furthermore, a study using data from the Korean Health Insurance Review and Assessment Service, fulminant myocarditis showed the highest incidence in infants under 28 days, and the incidence decreased with increasing age.
23
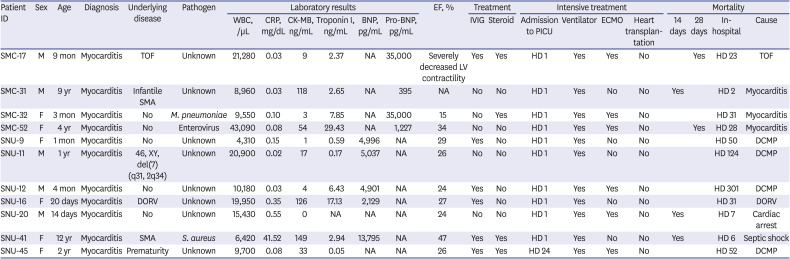
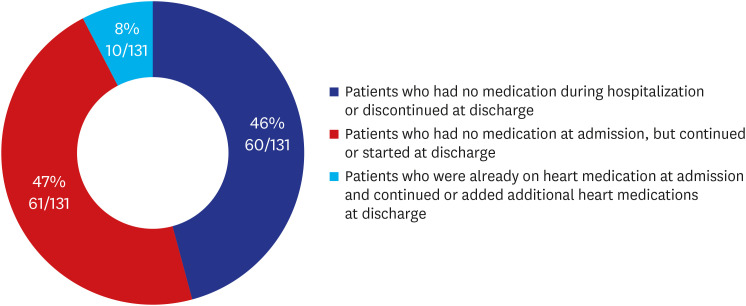
The current study can present further data on discharge medication and detailed information on mortality cases. In addition, statistical analysis on laboratory data showed that there were differences in CRP level, BNP level, and ejection fraction value between the survival group and death group. Furthermore, age younger than 1 year and myocarditis without pericarditis were the main risk factor for the composite poor outcomes. These may serve as useful markers to predict the patient's course and outcome for clinicians in the early course of the disease, and this needs to be further confirmed in future studies.
In this study, the vaccination record was not reviewed in relation to myocarditis/pericarditis development, and biopsy or MRI was not performed in all patients to make the definite diagnosis of etiology. This study was performed in two tertiary centers in the capital area. Therefore, selection bias might have occurred. In addition, the evaluation of etiology was not made uniformly.
In conclusion, we observed that myocarditis/pericarditis occurred most commonly in young infants and adolescents with male predominance, particularly in adolescents. Unlike infants, the outcome was fair in adolescents. Close monitoring for the occurrence of myocarditis/pericarditis is needed after the introduction of the COVID-19 vaccine to adolescents.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download