INTRODUCTION
The term “North Korean defector” refers to a person who has an address, family, spouse, or job in North Korea and has not acquired foreign nationality after escaping from North Korea.
1 According to the Ministry of Unification, 33,658 North Korean defectors (9,042 males and 24,256 females) had entered South Korea until March 31, 2020.
2 North Korean defectors have a lower level of health than South Koreans and have a higher level of desire to fulfil unmet medical needs because of many physical and mental health problems that may have been acquired during their defection.
34567 However, most of the national and international studies conducted on North Korean defectors have focused on mental health and have relied on questionnaires and interviews for data collection. Thus, there is a need for research on the physical health based on scientific evidence using big data to develop public health interventions directed toward these defectors.
789
South Korea has a National Health Insurance System (NHIS) that covers more than 99% of the total South Korean population, which includes North Korean defectors.
10 North Korean defectors are enrolled in the NHIS as a medical aid beneficiary type 1 at Hanawon, which is a non-profit public organization that was established by the Ministry of Unification in 2010, and their medical expenses for the services covered for the medical aid beneficiary type 1 are supported through public funds.
11 Therefore, there is a need to establish customized public health and healthcare policies to improve the health of North Korean defectors and to satisfy their desires for unmet medical needs. Furthermore, there is a need to comprehensively measure the health level of North Korean defectors based on summary measures of population health (SMPH) to provide a basis for effective policy decision-making.
The SMPH indicator has emerged to overcome the limitations of the traditional epidemiological indicators, such as incidence, prevalence, and mortality. Traditional epidemiological indicators cannot comprehensively measure health levels due to death, disease, disability, etc.; cannot consider the quality of life; and make it difficult to compare the health level of different countries. However, the SMPH is a single, efficient indicator that comprehensively measures the health burden in the population due to death, disease, and disability while considering the quality of life. Therefore, the SMPH facilitates the efficient use of limited healthcare resources.
Globally, efforts to comprehensively measure health levels, including injuries and deaths of individuals and groups, and to compare the health levels of different countries have continued and finally led to the development of several SMPH indicators.
12 Among the SMPH, the World Health Organization and the Institute for Health Metrics and Evaluation at the University of Washington (Seattle, Washington, USA), which supports major decision-making and projects on global health, have newly developed the disability-adjusted life years (DALYs) through the Global Burden of Diseases (GBD) project that was initiated in 1992.
131415 DALYs consist of the sum of the years of life lost (YLL) due to premature death, which refers to the number of years lost as a person dies earlier than their life expectancy, and the years lived with disability (YLD), which refers to the number of healthy years lost due to morbidity or injuries. Thus, one DALY means that one healthy year is lost due to premature death, disease, or disability. Therefore, the higher the DALY, the wider the gap from the ideal health level.
5 DALYs comprehensively measure the disease burden, including injuries and deaths, which bridges the gap between the ideal health level and the actual health level, and facilitates a consideration of the quality of life of the population as well as a comparison of health levels of countries. It is used to determine the priority of welfare policies.
16
In South Korea, the concept of DALYs was introduced in the late 1990s, and early studies in South Korea focused on individual diseases, such as stroke.
17 However, a recent study, which was conducted from 2013 to 2018 by the Research and Development (R&D) Project of the Ministry of Health and Welfare, measured the disease burden of South Koreans for all diseases.
18
This study was conducted with an aim to examine the disease burden of North Korean defectors in South Korea based on sex, age, and all diseases from 2000 to 2018 as well as to study the changes in the disease burden over time.
DISCUSSION
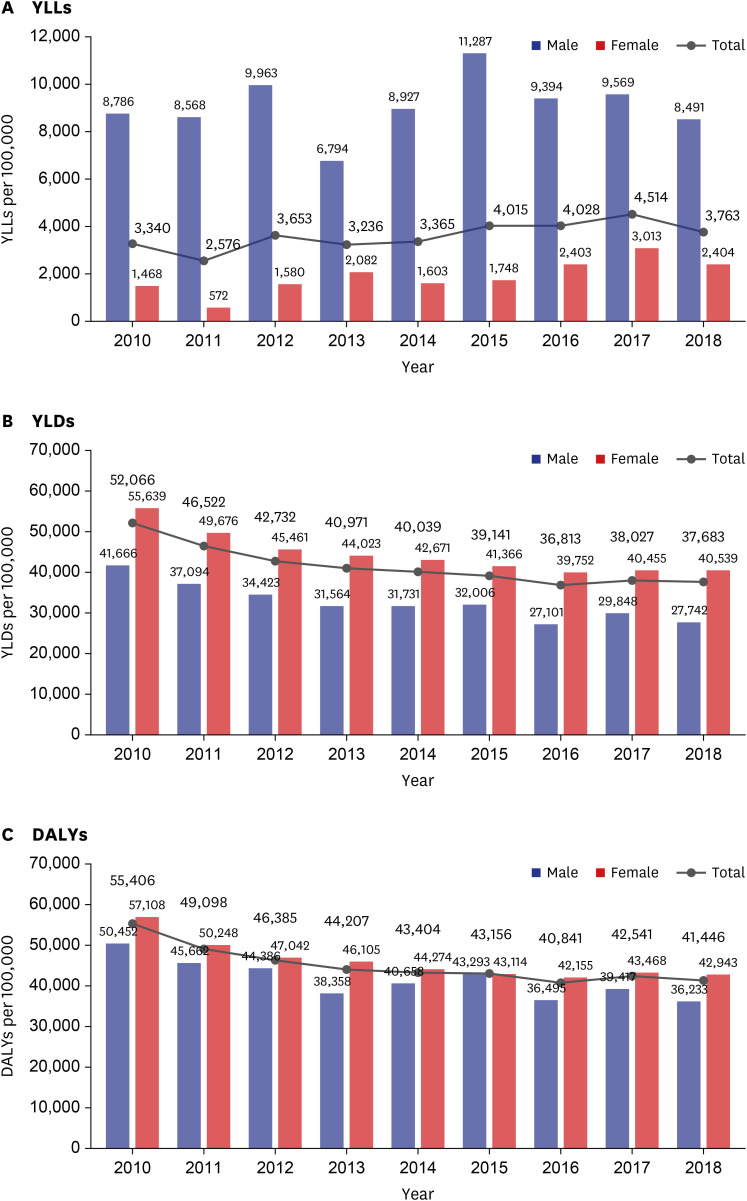
This study measured the disease burden of North Korean defectors from 2010 to 2018, and the results showed that the YLL per 100,000 population increased by approximately 13%, whereas the YLD per 100,000 population decreased by approximately 27.6%. Therefore, comprehensively, the DALY per 100,000 population decreased by 25.2% (
Fig. 4). This trend is completely opposite from that of disease burden in the South Korean population.
1018
The calculation of the YLL, YLD, and DALY per 100,000 population is based on the crude YLL, YLD, and DALY values as the numerator and the number of individuals in the population for a specific year as the denominator. Therefore, the YLL, YLD, and DALY per 100,000 population will be affected by the increase or decrease in the values of the numerator or denominator for the corresponding year.
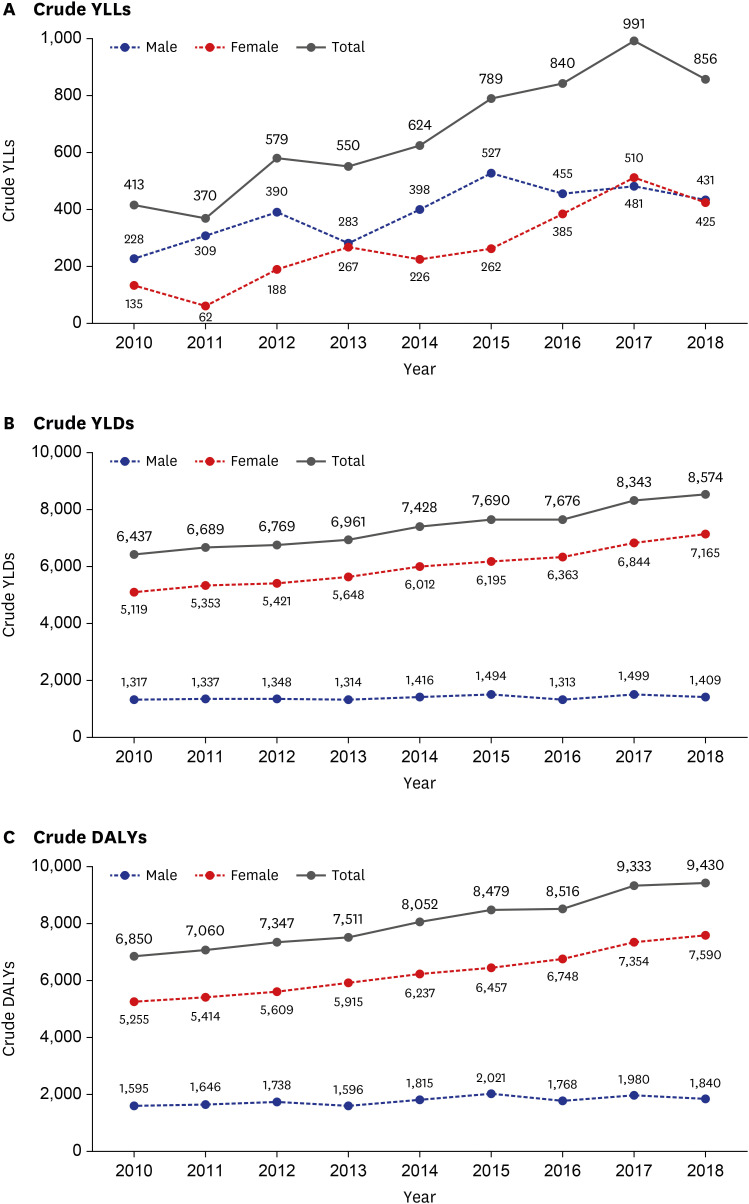
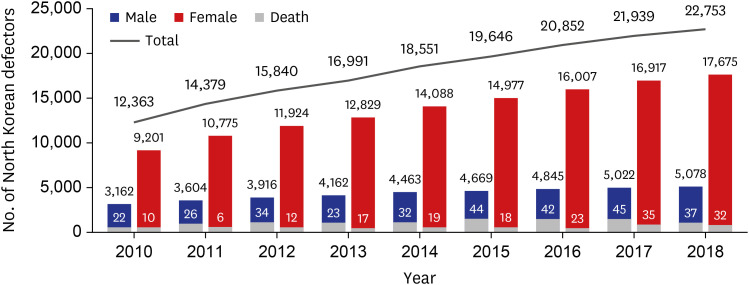
In this study, the crude YLL (the numerator) increased approximately 2.0 times from 413 in 2010 to 856 in 2018 (
Fig. 3A), whereas the number of study participants (North Korean defectors; denominator) increased by 1.8 from 12,363 in 2010 to 22,753 in 2018 (
Fig. 1). Therefore, the overall YLL rate per 100,000 people increased slightly. Also, one important thing to note is that the mortality rate relative to the annual population is at an average of 0.3% per year (
Fig. 1), so there was no difference between the mortality rates by year, but the increase of YLL rate per 100,000 people can be interpreted as the disease burden of premature death increasing.
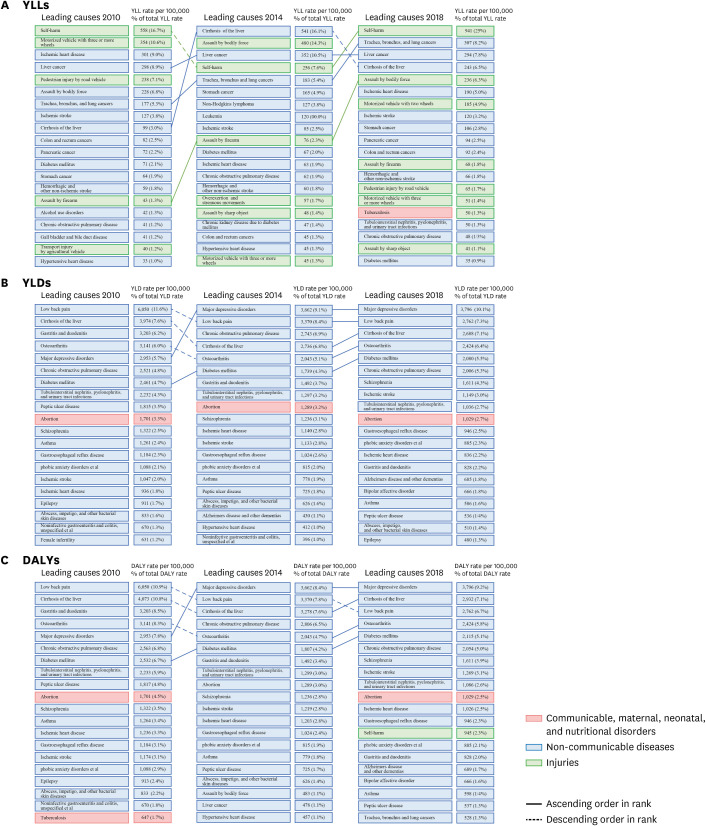
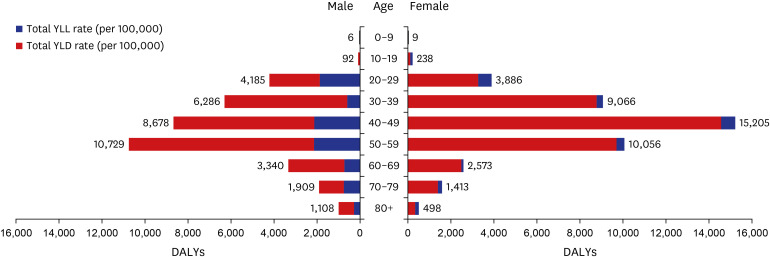
Therefore, when we analyzed the causes of disease burden due to premature death by specific sex, age, and disease at the lower level (levels 3 and 4) disease group, it showed that self-harm ranked highest (
Fig. 7A). Self-harm occupied the highest ranking in the YLL in 2010 and then showed a decreasing trend thereafter to rank fourth in 2014, but again reclaimed the highest rank in 2016. Self-harm occupied the highest ranking of the YLL in both males and females, although the YLL for males approximately twice that in females in 2018 (
Fig. 6B and C). Therefore, there is a need for a survey on self-harm and more in-depth research to establish customized health policies to prevent suicide of North Korean defectors.
Similarly, the crude YLD (the numerator) increased slightly by 1.1 times from 6,437 in 2010 to 8,574 in 2018, and the crude DALY (the numerator) increased by 1.4 times from 6,850 in 2010 to 9,430 in 2018 (
Fig. 3). However, the study population of North Korean defectors (denominator) increased 1.8 times from 12,363 in 2010 to 22,753 in 2018 (
Fig. 1). Therefore, the overall YLD and DALY rate per 100,000 people decreased somewhat (
Fig. 4).
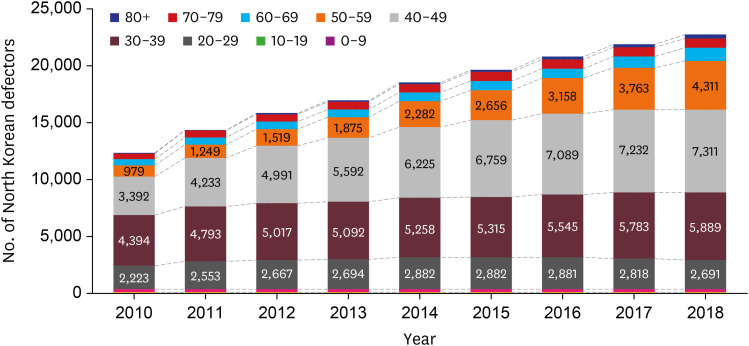
Further, compared to the increase in the population of North Korean defectors and in the crude YLD / DALY value, the tendency of the decrease in YLD and DALY per 100,000 can be considered the characteristics of the demographic structure by sex and age (
Fig. 2). We found on analysis that the number of North Korean defectors increased, but the ratio of females with relatively high disease burden was about 76% and the population in their 20s to 50s were about 88-89%, so the rate was increasing to the same level by year.
In particular, among the 88-89% of the age group in their 20s to 50s, the proportion of 20s and 30s was decreasing and the proportion of 40s and 50s was on the rise. Therefore, the decline in the disease burden of North Korean defectors is not caused by an increase in the population of males or young people (< aged 20) with relatively low disease burden.
However, in the case of South Koreans, the change in population number is not as large as for North Korean defectors, the sex ratio is at 100.4, which is slightly higher for in males than in females, and the number of people aged over 65 increased to 15.7% in 2020.
23 Therefore, disease burden of South Koreans due to premature death is decreasing and the comprehensive disease burden of South Korean increasing through increase in life expectancy due to the development of medical technology.
816
Therefore, if North Korean defectors are aging as the period of residence in Korea increases, it is predicted that the North Korean defectors will show a similar trend in disease burden to that of South Koreans in the future, while the number of North Korean defectors shows almost no change.
As this study is the first to measure the disease burden of North Korean defectors, it is necessary to consider other studies that measured the disease burden of North Koreans as a reference when interpreting the results. According to the GBD 2017 study, which targeted North Korea, NCD accounted for the largest portion of disease burden at 78.81%.
24 In addition, many studies have reported the NCD burden in North Korea.
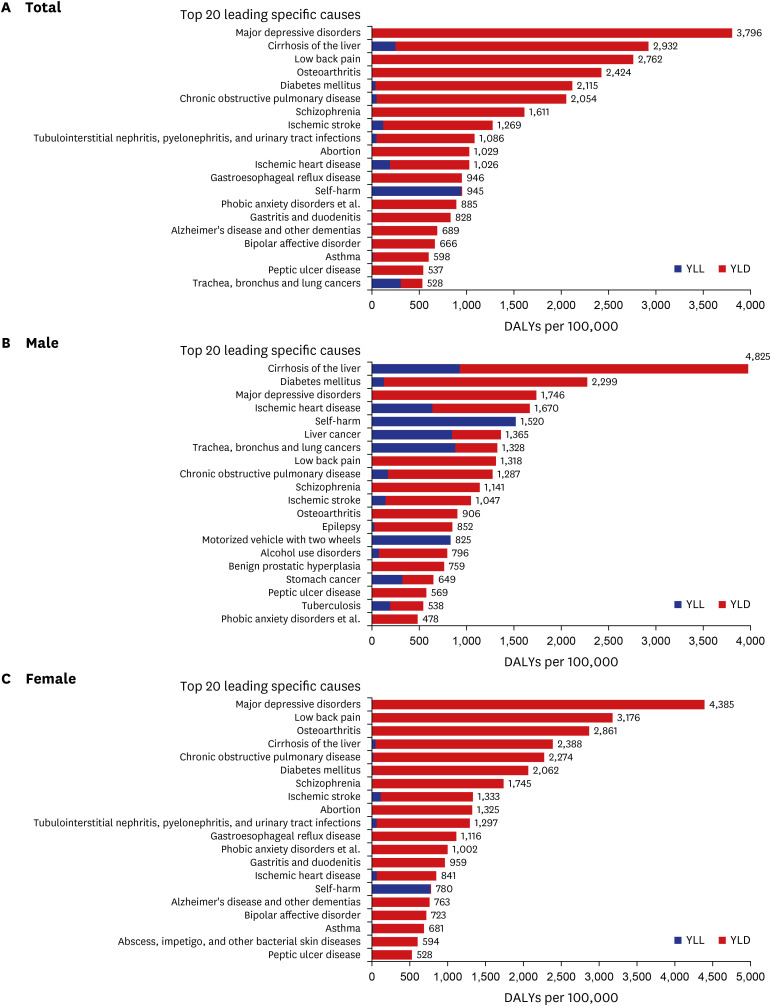
2526 A detailed analysis of disease burden ranking at the higher level (level 1) disease group is shown in
Supplementary Fig. 1.
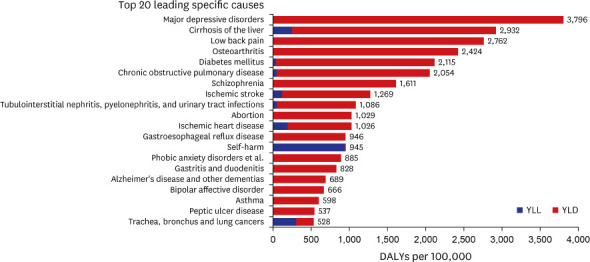
Specific analysis of the ranking of disease burden at the lower level (levels 3 and 4) disease group showed that major depressive disorders constituted a high-ranking disease burden for North Korean defectors in 2018 (
Fig. 7C). Despite the overall declining trend in the disease burden of North Korean defectors from 2010 to 2018 (
Fig. 4C), the proportion of major depressive disorders increased to 843 DALY (28.5%). In general, many studies reported that North Korean defectors have a higher prevalence of mental disorders (i.e., major depressive disorders, bipolar affective disorder, and post-traumatic stress disorder) compared to South Koreans.
2728 In addition, one study reported that the longer the period that North Korean defectors took to settle in South Korea, the less was the burden of post-traumatic stress disorder; however, the burden of depression increased.
29
Mental disorder is a well-known factor that is related to the quality of life.
28 Therefore, in future, it is necessary to analyze the changes in the disease burden of the North Korean defectors according to their period of residence in South Korea. In this regard, there is a need to establish a health policy to improve the mental health and quality of life of North Korean refugees.
Next, cirrhosis was ranked second highest in terms of disease burden in North Korean defectors in 2018, and held the same ranking as in 2010 (
Fig. 7C). The disease burden due to cirrhosis decreased by approximately −1,141 (−28%) from 2010 to 2018 while still ranking high in the disease burden of North Korean defectors. In particular, the disease burden due to cirrhosis was 2.0 times higher in males than in females in 2018 (
Fig. 6B and C). However, these results need to be interpreted with due consideration of the classification process for the categorized causes of death. In this study, when distributing the categorized causes of death, the sex- and age-stratified prevalence of the disease for the specific year was referenced, and the number of deaths due to the disease was distributed according to the corresponding ratio. As a result, most of the deaths for the category of viral hepatitis (B15–B19) codes were distributed toward liver cirrhosis (B19), which had a higher prevalence than Hepatitis A (B15), Hepatitis B (B16), Hepatitis C (B17), and Hepatitis E (B18). Thus, the comprehensive health-related disease burden (DALY), including the disease burden due to premature death (YLL), indicated that cirrhosis had a higher disease burden. Therefore, it is necessary to obtain the cause of death by specific diseases and to more precisely connect the NHIS customized database with the cause of death in the future.
Third, low back pain was ranked third in terms of the disease burden for North Korean defectors in 2018 despite having been ranked first in 2010 (
Fig. 7C). The disease burden of low back pain decreased by −3,288 (−54.4%) from 2010 to 2018, but it still ranked high in the disease burden of North Korean defectors. In particular, low back pain was 2.4 times higher in females than in males in 2018 (
Fig. 6B and C). The disease burden due to low back pain is increasing in high-income countries, particularly in high-income Asia-Pacific countries.
24 This increase appears attributable to sociocultural characteristics, including child-rearing and household chores for which women have the main responsibility, as well as physiological changes such as pregnancy, childbirth, menopause, and aging.
10
Osteoarthritis was ranked fourth in the disease burden for North Korean defectors in 2018, at the same ranking as in 2010 (
Fig. 7). Similar to that for low back pain, the disease burden of osteoarthritis was 3.2 times higher in females than in males in 2018 (
Fig. 6B and C), and it seems to be caused by sociocultural factors for which women have the main responsibility, as well as physiological changes. Therefore, there is a need to establish customized health policies by considering the characteristics of each disease by sex and age.
Lastly, diabetes mellitus was ranked fifth in terms of the disease burden for North Korean defectors, but was the seventh commonest disease in North Korean defectors in 2010 (
Fig. 7). Diabetes mellitus decreased by about −417 (−16.5%) from 2010 to 2018, but it still ranks high in the disease burden of North Korean defectors. In the case of diabetes mellitus, males were 1.1 times higher than females, both similarly high in 2018 (
Fig. 6B and C). According to the North Korean Refugee Health in South Korea (NORNS) Study, North Korean defectors have a high degree of normal weight obesity (the degree of obesity is not severe, but the risk of metabolic syndrome is similar to that of people with obesity), and the longer the period for North Korean defectors to settle in South Korea, the higher is the risk of metabolic syndrome compared to that of South Koreans.
3031
Thus, North Korean defectors can be considered to constitute a high-risk group in the future, and it is necessary to analyze the change in the disease burden of North Korean defectors according to their period of residence in South Korea. Therefore, there is a need to establish a health policy to decrease the disease burden of NCD due to diabetes mellitus and to improve the health level of North Korean defectors.
As more North Korean defectors are entering South Korea every year, the top 20 diseases in terms of disease burden are changing considerably. In 2018, most of the other top 20 diseases, excluding the above five diseases, were NCD. In this study, the disease burden of North Korean defectors was calculated from 2010 to 2018 using DALY, and characteristics were analyzed by sex, age, and disease. In future studies, if a 1:1 or 1:4 age- and sex-matched population of South Koreans can be compared with the population of North Korean defectors, a more meaningful understanding of the disease burden between North Korean defectors and the South Korean population can be obtained.
21 In addition, if it were possible to obtain variables for annual medical checkups in the NHIS database, it would be possible to analyze the relationship between the disease burden and risk factors, such as drinking and smoking.
32
This study has several limitations. First, in this study, we attempted to measure the actual disease burden of North Korean defectors who live in South Korea and have difficulty adapting due to actual injury, illness, and premature death. Thus, the study participant was defined as a person who received medical benefits as a North Korean defector and as a head of the household of medical aid beneficiary type 1 in the NHIS customized research database. This corresponds to approximately 69% of the total North Korean defectors, and the remaining 31%, comprising heads of households of local subscription, households of local subscription, head of household in employer insurance, household with employer insurance, and households of medical aid beneficiary type 1, were excluded. Therefore, North Korean defectors who lost their status as head of a household of medical aid beneficiary type 1 due to the fact that their recognized income exceeded the standard median income of the medical aid beneficiary type 1 were excluded from the measurement of disease burden. Thus, when the number of the remaining 31% of North Korean defectors is included, the results may be partially different.
Second, the disease burden could have been underestimated by the use of claims data as a main source of data because claim data are not created for the use of medical services, such as the non-reimbursement and diagnosis-related groups of diseases. In addition, claims data could pose some problems with regard to inaccuracies in the code of the diagnosis, as reported generally.
21 Furthermore, in order to more precisely calculate the disease burden of North Korean defectors, it is necessary to obtain additional data, such as data on cancer, injury from hospital discharge information, standard life expectancy, duration of disease, and DW, from the relevant organizations in the future.
Another limitation is due to the limitations of the analytical methodology. In this study, the disease burden of North Korean defectors was measured according to the incidence-based DALY developed in the KNBD study
10; however, as the study subjects were North Korean defectors, there could be some possible differences in the calculation of the DALY. For example, the disease burden due to premature death is directly related to the number of deaths by sex, age, and disease in a specific year. In particular, in the case of North Korean defectors, the number of deaths is very small; therefore, the YLL is greatly affected by the sex, age, and cause of death of the deceased in a specific year. Therefore, to calculate the YLL, the categorized death code of North Korean defectors that was obtained was redistributed based on the sex- and age-stratified disease prevalence in claims data for the year. When there was no prevalence data or death data for reference, the data were not distributed as the number of prevalence or deaths due to specific diseases. Individuals whose cause of death was unknown accounted for approximately one-third of the total dead among North Korean defectors. Thus, future studies should obtain the cause of death for specific diseases to more precisely connect the NHIS customized database with the cause of death.
Finally, it is necessary to develop a measurement methodology to calculate the standardized disease burden of North Korean defectors by incorporating their population-specific characteristics and the limitations of data sources in the future.
Despite these limitations, this study is meaningful as it is the first study to measure the disease burden of North Korean defectors in South Korea based on claims data for the use of medical services. With regard to the decreasing trends of disease burden or those with a substantially increasing disease burden, it is necessary to establish appropriate policies in a timely manner. The results of this study can provide the basis for customized public health and healthcare policies for North Korean defectors in South Korea.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download