INTRODUCTION
Heart failure (HF) is a complex clinical syndrome and a public health problem because of its high prevalence, huge socioeconomic burden and poor outcome.
1) People with HF are estimated to be more than 50 million worldwide and the prevalence of HF will continue to rise due to society aging, increased prevalence of cardiovascular risk factors and improved survival from cardiovascular diseases. The burden and cost of treating HF are primarily driven by high hospitalization and mortality rates despite recent significant progression of medical and surgical treatments.
2)3) Although the global economic burden of HF is not known exactly, overall treatment cost of HF comprises almost 2% of total health expenditures in most countries and is rapidly increasing.
4)5)6) For example, HF care cost was increased by 50% over last 5 years in Korea. HF imposes both direct costs to healthcare systems and indirect costs to society through morbidity, unpaid care costs, premature mortality and lost productivity. It is also reported that high-income countries spend a greater proportion on direct costs and a pattern reversed for middle- and low-income countries.
6) Thorough information of HF care costs and their determinants is not only valuable in optimizing HF management to reduce HF costs but also important to governmental policy makers to forecast a healthcare budget for a rapidly growing and aging population.
1)6)
It is a well-known fact that the onset of HF is strongly correlated with aging, and the burden of HF continues to rise in several countries as they enter an aging society. We previously published the prevalence of HF in Korea to be 1.53% in 2013, and this was expected to increase by 2-fold, from 1.60% in 2015 to 3.35% in 2040 by analyzing National Sample Cohort of the National Health Information Database.
7) According to Shimokawa et al.,
8) the prevalence of HF among hospitalized patients ranged from 3.4% to 6.7% based on estimates in Asia. To better manage the burden of HF in Asia, both primary prevention of the underlying disease and secondary prevention are important. Unfortunately, there is insufficient data on the current burden of HF to appropriately inform health policy makers. Based on a limited number of reports, the estimated prevalence of HF in Asia is 1.26–6.7%. However, the lack of standard definition of HF and appropriate surveillance systems make estimation of the HF burden in Asia challenging.
9) The present study aimed to understand and present the economic burden of HF among Asian populations treated at the hospital level under different healthcare systems in Asia.
METHODS
Ethical statement
The study was approved by the ethics committees of Chungbuk National University Hospital Institutional Review Board (IRB 2016-06-004), Seoul National University Bundang Hospital IRB (B-1606/352-105), Taipei Veterans General Hospital IRB (2016-08-003BC), Ramathibodi Hospital IRB (MURA2016/503), and Malaysia Medical Research & Ethics Committee (NMRR-16-1039-30990 [ISR]).
No identifiable personal information was provided, and no risk arose to any patient participating in this retrospective observational study. Therefore, the informed consent form was waived by the ethics committees.
Study design
This was a non-interventional, retrospective study conducted through medical chart and hospital record review of patients with HF, utilizing real-world patient-level data from 6 sites across 4 Asian countries: South Korea (2 sites), Taiwan (1 site), Thailand (1 site), and Malaysia (2 sites). Subjects were followed for 1 year after the first visit to the hospital due to HF (index date) (
Supplementary Figure 1). Criteria for selection of hospital sites for conducting the study were driven by the size of the hospital (national hospital in Taiwan and university hospital in Thailand; tertiary hospitals in Malaysia with established cardiology unit and feasibility to enroll HF patients), diverse geographical location (area coverage and feasibility to enroll required number of HF patients in South Korea) and the investigators (reputed investigators with experience in conducting studies). Primary outcomes of interest were costs attributed to HF and healthcare resource utilization. Secondary endpoints included analysis of clinical characteristics and resource use; in addition, subgroup analysis of assessment of cost of HF stratified by age and sex was conducted.
Patients who visited between January 1, 2014, and December 31, 2014 (index period: 1 year) and met the inclusion criteria were recruited in this study. Patients were followed for 1 year from the index date (study period: 2 years).
Eligible patients were over 19 years of age with diagnosis of HF (International Statistical Classification of Diseases and Related Health Problems [ICD] 9 or ICD 10 code) and had 1-year follow-up data from the index date. Patients who had experienced either ≥1 hospitalization or ≥2 outpatient visits were included in the study. Following patients were excluded: only 1 outpatient visit and no hospitalization during the follow-up period; received anticancer chemotherapy during the year after the index date; enrolled in an interventional clinical trial; determined to meet exclusion criteria by the investigator; and died during the study period.
Data for all variables (presented in
Supplementary Table 1) were logically collected via electronic-case report forms to minimize errors in data entry. Comorbidities of interest were atrial fibrillation, diabetes, hypertension, hypotension, dyslipidemia, chronic obstructive pulmonary disease (COPD), prior myocardial infarction, angina, cancer, stroke/transient ischemic attack, percutaneous coronary intervention, and coronary artery bypass graft. Resource use assessments included number of HF-related outpatient visits for follow-up within 1 year after the index date, hospitalizations, and emergency visits. HF-related costs were obtained by making enquiries with each hospital administration department, and costs for hospitalizations, outpatient visits, medication, laboratory tests, imaging tests, diagnostic tests, surgery and procedures, and other costs were deemed as direct medical costs. Medical costs consisted of costs borne by National Health Insurance (NHI-covered) and the patient (non-NHI covered). All costs were adjusted to 2015 US dollars by using the conversions given in
Supplementary Table 2.
10)
Statistical analysis
Analysis performed on subjects with non-missing data, and statistical comparisons were made using two-sided tests at α = 0.05 significance level (without adjustment of the threshold regarding the increase of tests). If relevant, 95% confidence interval was calculated. Patient characteristics, comorbidities of interest, healthcare use, and costs were descriptively summarized. Continuous variables were presented with mean and standard deviation (SD), while categorical variables were described with frequency and percentage of patients per response category. Missing values were not included in the calculation of percentage of responses per category.
Factors affecting costs associated with HF were analyzed using multivariate analysis. Cost was calculated on an annual basis for each patient. Annual cost was analyzed using a generalized linear regression model (GLM) with log link and gamma family distribution to estimate cost function. All statistical inferences were based on nonparametric clustered bootstrapped confidence intervals by using the percentiles approach. Age, sex, body mass index (BMI), left ventricular ejection fraction (LVEF), previous HF treatment, comorbidities (hypertension, COPD, and diabetes), annual outpatient visit frequency, hospitalization experience, emergency room (ER) visits, and country were analyzed as explanatory variables. Quantification of costs was performed considering NHI coverage. All statistical analyses were performed using the SAS 9.4 (SAS Institute, Cary, NC, USA) software. All results were provided for the full analysis set (FAS), comprising of all patients enrolled in the study.
RESULTS
Baseline clinical characteristics
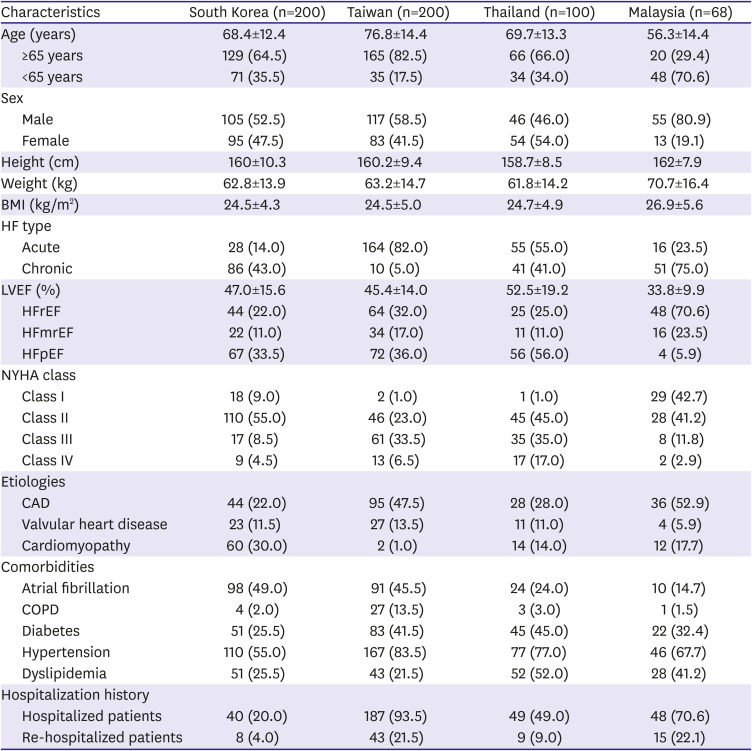
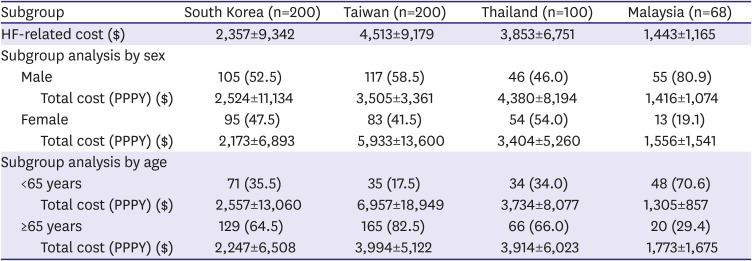
In total, 568 patients from six tertiary hospitals were included: 200 each from South Korea and Taiwan, 100 from Thailand, and 68 from Malaysia. The proportion of patients with hospitalization ranged from 20.0% to 93.5% (20.0% [40/200], 49.0% [49/100], 70.6% [48/68], and 93.5% [187/200] in South Korea, Thailand, Malaysia, and Taiwan, respectively). The mean LVEF (SD) ranged from 33.8% (9.9) to 52.5% (19.2), and the proportion of patients with LVEF ≤35% ranged from 17.0% to 69.1% in the 4 countries. Among HF patients with New York Heart Association (NYHA) classification data available, majority of Korean patients were NYHA class II (55.0%), whereas half of Taiwanese patients were class III at the index date. In case of Thailand, 45.0% of patients were class II, and patients from Malaysia were primarily in class I (42.7%) and class II (41.2%) at the index date.
The most frequent etiology reported across countries was cardiomyopathy in South Korea (30.0%), and coronary artery disease (CAD) in Taiwan (47.5%), Thailand (28.0%), and Malaysia (52.9%). The most frequent comorbidity in all countries was hypertension (South Korea 55.0%, Taiwan 83.5%, Thailand 77.0%, and Malaysia 67.7%), followed by atrial fibrillation (South Korea 49.0% and Taiwan 45.5%) and dyslipidemia (Thailand 52.0% and Malaysia 41.2%) (
Table 1).
Table 1
Baseline demographics
|
Characteristics |
South Korea (n=200) |
Taiwan (n=200) |
Thailand (n=100) |
Malaysia (n=68) |
|
Age (years) |
68.4±12.4 |
76.8±14.4 |
69.7±13.3 |
56.3±14.4 |
|
≥65 years |
129 (64.5) |
165 (82.5) |
66 (66.0) |
20 (29.4) |
|
<65 years |
71 (35.5) |
35 (17.5) |
34 (34.0) |
48 (70.6) |
|
Sex |
|
|
|
|
|
Male |
105 (52.5) |
117 (58.5) |
46 (46.0) |
55 (80.9) |
|
Female |
95 (47.5) |
83 (41.5) |
54 (54.0) |
13 (19.1) |
|
Height (cm) |
160±10.3 |
160.2±9.4 |
158.7±8.5 |
162±7.9 |
|
Weight (kg) |
62.8±13.9 |
63.2±14.7 |
61.8±14.2 |
70.7±16.4 |
|
BMI (kg/m2) |
24.5±4.3 |
24.5±5.0 |
24.7±4.9 |
26.9±5.6 |
|
HF type |
|
|
|
|
|
Acute |
28 (14.0) |
164 (82.0) |
55 (55.0) |
16 (23.5) |
|
Chronic |
86 (43.0) |
10 (5.0) |
41 (41.0) |
51 (75.0) |
|
LVEF (%) |
47.0±15.6 |
45.4±14.0 |
52.5±19.2 |
33.8±9.9 |
|
HFrEF |
44 (22.0) |
64 (32.0) |
25 (25.0) |
48 (70.6) |
|
HFmrEF |
22 (11.0) |
34 (17.0) |
11 (11.0) |
16 (23.5) |
|
HFpEF |
67 (33.5) |
72 (36.0) |
56 (56.0) |
4 (5.9) |
|
NYHA class |
|
|
|
|
|
Class Ⅰ |
18 (9.0) |
2 (1.0) |
1 (1.0) |
29 (42.7) |
|
Class Ⅱ |
110 (55.0) |
46 (23.0) |
45 (45.0) |
28 (41.2) |
|
Class Ⅲ |
17 (8.5) |
61 (33.5) |
35 (35.0) |
8 (11.8) |
|
Class Ⅳ |
9 (4.5) |
13 (6.5) |
17 (17.0) |
2 (2.9) |
|
Etiologies |
|
|
|
|
|
CAD |
44 (22.0) |
95 (47.5) |
28 (28.0) |
36 (52.9) |
|
Valvular heart disease |
23 (11.5) |
27 (13.5) |
11 (11.0) |
4 (5.9) |
|
Cardiomyopathy |
60 (30.0) |
2 (1.0) |
14 (14.0) |
12 (17.7) |
|
Comorbidities |
|
|
|
|
|
Atrial fibrillation |
98 (49.0) |
91 (45.5) |
24 (24.0) |
10 (14.7) |
|
COPD |
4 (2.0) |
27 (13.5) |
3 (3.0) |
1 (1.5) |
|
Diabetes |
51 (25.5) |
83 (41.5) |
45 (45.0) |
22 (32.4) |
|
Hypertension |
110 (55.0) |
167 (83.5) |
77 (77.0) |
46 (67.7) |
|
Dyslipidemia |
51 (25.5) |
43 (21.5) |
52 (52.0) |
28 (41.2) |
|
Hospitalization history |
|
|
|
|
|
Hospitalized patients |
40 (20.0) |
187 (93.5) |
49 (49.0) |
48 (70.6) |
|
Re-hospitalized patients |
8 (4.0) |
43 (21.5) |
9 (9.0) |
15 (22.1) |

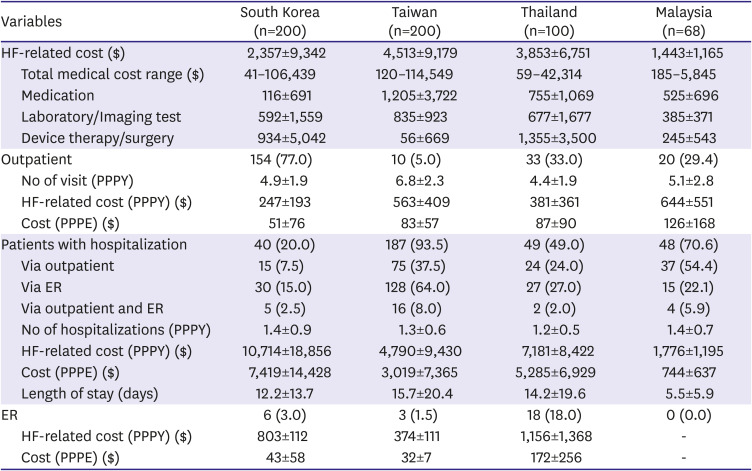
Heart failure-related cost and healthcare utilization
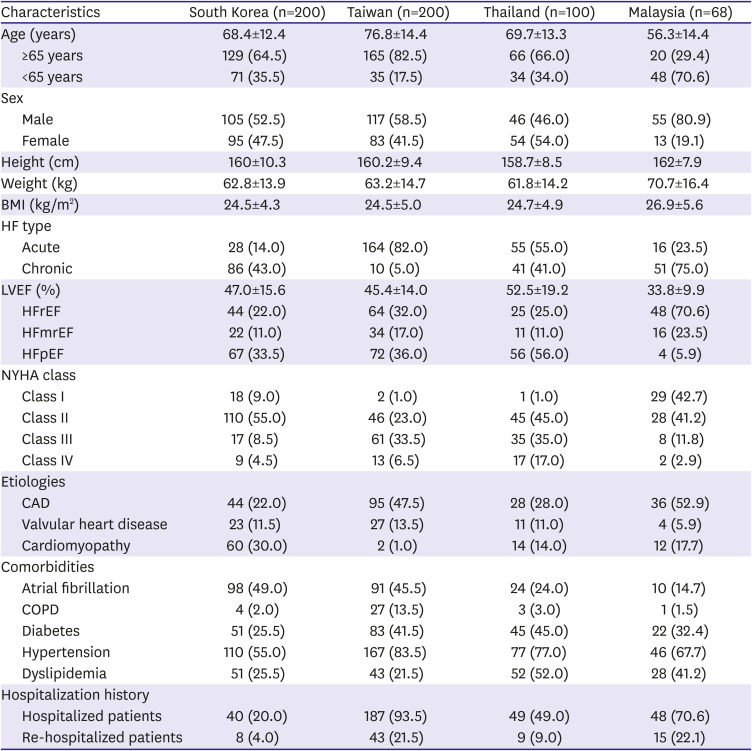
The HF-related cost per patient per year (PPPY) was $2,357 in South Korea, $4,513 in Taiwan, $3,853 in Thailand and $1,443 in Malaysia (
Table 2).
Table 2
HF-related costs and healthcare utilization
|
Variables |
South Korea (n=200) |
Taiwan (n=200) |
Thailand (n=100) |
Malaysia (n=68) |
|
HF-related cost ($) |
2,357±9,342 |
4,513±9,179 |
3,853±6,751 |
1,443±1,165 |
|
Total medical cost range ($) |
41–106,439 |
120–114,549 |
59–42,314 |
185–5,845 |
|
Medication |
116±691 |
1,205±3,722 |
755±1,069 |
525±696 |
|
Laboratory/Imaging test |
592±1,559 |
835±923 |
677±1,677 |
385±371 |
|
Device therapy/surgery |
934±5,042 |
56±669 |
1,355±3,500 |
245±543 |
|
Outpatient |
154 (77.0) |
10 (5.0) |
33 (33.0) |
20 (29.4) |
|
No of visit (PPPY) |
4.9±1.9 |
6.8±2.3 |
4.4±1.9 |
5.1±2.8 |
|
HF-related cost (PPPY) ($) |
247±193 |
563±409 |
381±361 |
644±551 |
|
Cost (PPPE) ($) |
51±76 |
83±57 |
87±90 |
126±168 |
|
Patients with hospitalization |
40 (20.0) |
187 (93.5) |
49 (49.0) |
48 (70.6) |
|
Via outpatient |
15 (7.5) |
75 (37.5) |
24 (24.0) |
37 (54.4) |
|
Via ER |
30 (15.0) |
128 (64.0) |
27 (27.0) |
15 (22.1) |
|
Via outpatient and ER |
5 (2.5) |
16 (8.0) |
2 (2.0) |
4 (5.9) |
|
No of hospitalizations (PPPY) |
1.4±0.9 |
1.3±0.6 |
1.2±0.5 |
1.4±0.7 |
|
HF-related cost (PPPY) ($) |
10,714±18,856 |
4,790±9,430 |
7,181±8,422 |
1,776±1,195 |
|
Cost (PPPE) ($) |
7,419±14,428 |
3,019±7,365 |
5,285±6,929 |
744±637 |
|
Length of stay (days) |
12.2±13.7 |
15.7±20.4 |
14.2±19.6 |
5.5±5.9 |
|
ER |
6 (3.0) |
3 (1.5) |
18 (18.0) |
0 (0.0) |
|
HF-related cost (PPPY) ($) |
803±112 |
374±111 |
1,156±1,368 |
- |
|
Cost (PPPE) ($) |
43±58 |
32±7 |
172±256 |
- |

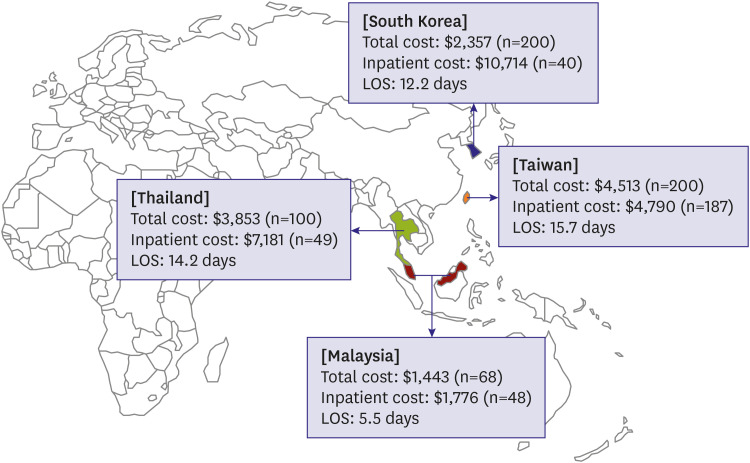
Country-wise analysis of data revealed hospitalization experience as one of the prominent cost drivers in most countries (
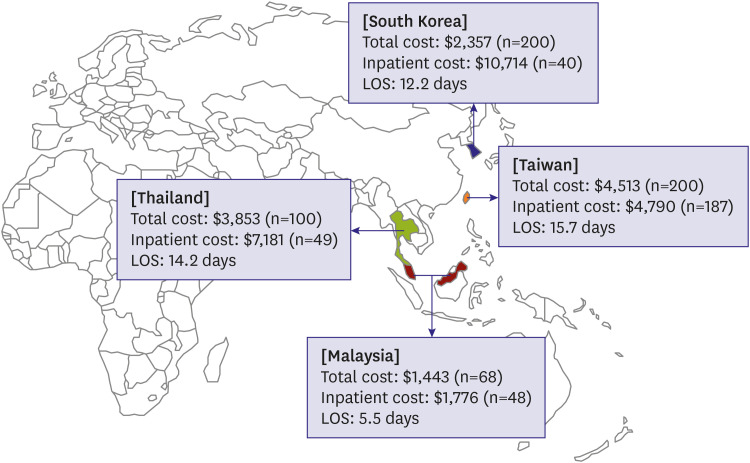
Table 2). This burden was highest in South Korea, where the annual HF-related cost incurred by patients due to HF-related hospitalization ($10,714) was about 4.5 times higher than the average annual cost incurred by all HF patients ($2,357). The average number of hospitalization was 1.4 per year, costing $7,419 per hospitalization, with an average length of stay of 12.2 days.
Almost all patients in Taiwan had hospitalization experience (93.5%), with an average of 1.3 admissions, costing $4,790 per year. Patients spent $3,019 and stayed for an average of 15.7 days per admission.
Similarly, in Thailand, the annual HF-related cost for patients with hospitalization was almost twice ($7,181) as high as that for all HF patients ($3,853). The average number of HF hospitalizations was 1.2 times per year, and hospitalization cost and length of stay were $5,285 and 14.2 days per event, respectively.
In Malaysia, patients were hospitalized 1.4 times per year, and for patients with HF hospitalization, the annual cost was $1,776.The average cost per admission was $744, and the average length of stay was 5.5 days per admission. In all countries except Malaysia, the average length of stay was >10 days.
A snapshot of the mean cost incurred and resource use associated with hospitalized patients in the four countries is presented in
Figure 1. Total cost estimates according to various variables are presented in
Supplementary Tables 3-
6.
Figure 1
Costs and resource use for hospitalized patients in four Asian countries.
LOS = length of stay.

Re-hospitalizations were noted for 4.0% to 22.1% of the patients across all countries, implying considerable burden attributed to the event (
Table 1).
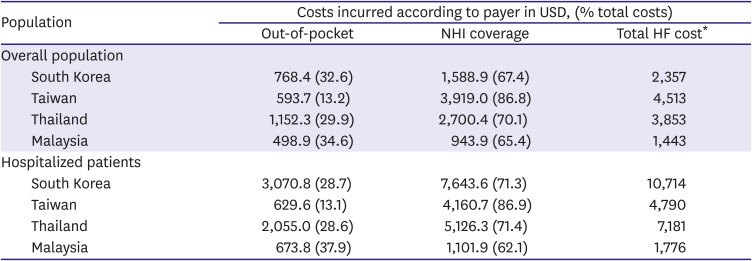
Out-of-pocket cost and National Health Insurance coverage in total HF costs in each country
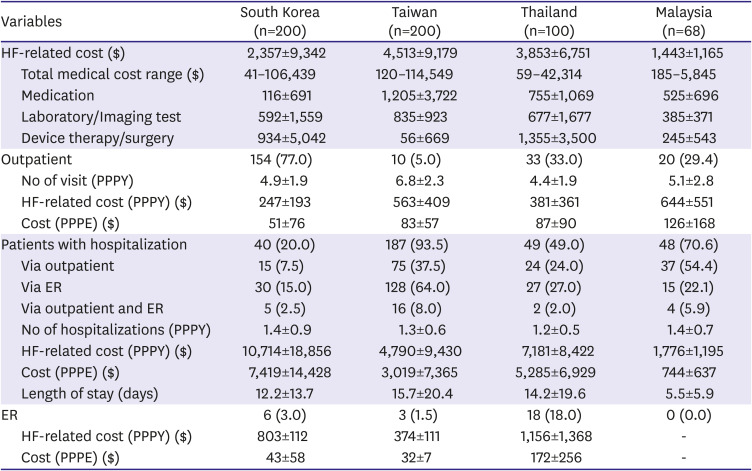
The costs were further divided according to the reimbursement status in the countries.
Table 3 represents total costs incurred according to the quantum paid by the government (NHI-covered) and by the patients in each country. Most of the burden of the healthcare cost was sustained by the government, which was found to be 67.4% for South Korea, 86.8% for Taiwan, 70.1% for Thailand and 65.4% for Malaysia. Similar results were observed for costs incurred by payers for patients with hospitalization (
Table 3).
Table 3
Fractions of total costs covered by NHI expenses and out-of-pocket expenses
|
Population |
Costs incurred according to payer in USD, (% total costs) |
|
Out-of-pocket |
NHI coverage |
Total HF cost*
|
|
Overall population |
|
|
|
|
South Korea |
768.4 (32.6) |
1,588.9 (67.4) |
2,357 |
|
Taiwan |
593.7 (13.2) |
3,919.0 (86.8) |
4,513 |
|
Thailand |
1,152.3 (29.9) |
2,700.4 (70.1) |
3,853 |
|
Malaysia |
498.9 (34.6) |
943.9 (65.4) |
1,443 |
|
Hospitalized patients |
|
|
|
|
South Korea |
3,070.8 (28.7) |
7,643.6 (71.3) |
10,714 |
|
Taiwan |
629.6 (13.1) |
4,160.7 (86.9) |
4,790 |
|
Thailand |
2,055.0 (28.6) |
5,126.3 (71.4) |
7,181 |
|
Malaysia |
673.8 (37.9) |
1,101.9 (62.1) |
1,776 |

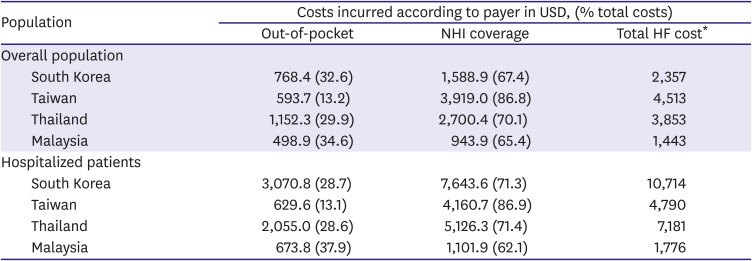
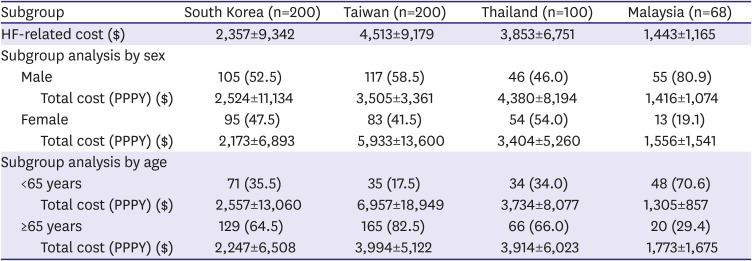
Annual heart failure-related cost by sex and age
In sex and age subgroup analyses of annual HF-related costs, no particular trend was noted among countries. The HF-related cost PPPY in men was the highest in Thailand; in contrast, women incurred higher costs in Taiwan. Moreover, the HF-related cost PPPY was higher for male patients versus female patients in South Korea ($2,524 vs. $2,173) and Thailand ($4,380 vs. $3,404), and was vice versa in Taiwan ($5,933 vs. $3,505) and Malaysia ($1,556 vs. $1,416). Younger (<65 years) Korean and Taiwanese patients incurred higher HF-related healthcare costs compared with their older counterparts, whereas HF-related costs in older patients (≥65 years) was much higher in Thailand and Malaysia (
Table 4).
Table 4
Annual HF-related cost by sex and age
|
Subgroup |
South Korea (n=200) |
Taiwan (n=200) |
Thailand (n=100) |
Malaysia (n=68) |
|
HF-related cost ($) |
2,357±9,342 |
4,513±9,179 |
3,853±6,751 |
1,443±1,165 |
|
Subgroup analysis by sex |
|
|
|
|
|
Male |
105 (52.5) |
117 (58.5) |
46 (46.0) |
55 (80.9) |
|
|
Total cost (PPPY) ($) |
2,524±11,134 |
3,505±3,361 |
4,380±8,194 |
1,416±1,074 |
|
Female |
95 (47.5) |
83 (41.5) |
54 (54.0) |
13 (19.1) |
|
|
Total cost (PPPY) ($) |
2,173±6,893 |
5,933±13,600 |
3,404±5,260 |
1,556±1,541 |
|
Subgroup analysis by age |
|
|
|
|
|
<65 years |
71 (35.5) |
35 (17.5) |
34 (34.0) |
48 (70.6) |
|
|
Total cost (PPPY) ($) |
2,557±13,060 |
6,957±18,949 |
3,734±8,077 |
1,305±857 |
|
≥65 years |
129 (64.5) |
165 (82.5) |
66 (66.0) |
20 (29.4) |
|
|
Total cost (PPPY) ($) |
2,247±6,508 |
3,994±5,122 |
3,914±6,023 |
1,773±1,675 |

Generalized linear model analysis in heart failure costs
While analyzing factors that affect cost of HF by use of GLM, the analysis was not extended to Korea and Taiwan settings owing to a large number of missing BMI, LVEF, and NYHA values. In Thailand, LVEF <40% was found to be a positive predictor of higher cost of HF, whereas in Malaysia, NYHA class IV was associated with higher costs compared with NYHA class II or III (details in
Supplementary Tables 7-
10).
DISCUSSION
The objective of this study was to understand and present the economic burden of HF among Asian populations treated at the hospital level. Findings of the study highlight hospitalization (and re-hospitalization) as a key driver of overall costs associated with HF. In addition, the authors assessed clinical characteristics of patients from various Asian countries alongside age- and sex-stratified analyses.
The clinical profiles of patients with HF were similar across all evaluated countries except Malaysia. Malaysian patients were younger, with a higher proportion of men, and with a clinical profile significantly different from those of patients from the other 3 countries. This difference in clinical profiles of patients can be partially explained by differences in age and sex. A higher percentage of Malaysian patients in this study were NYHA class I category, with a lower percentage of patients with previous HF and a high percentage of patients with chronic HF (but comparable to South Korea). The same study protocol was applied to all participating countries, and the differences observed did not seem to stem from methodological reasons.
According to Cook et al.,
6) globally overall HF cost was $108 billion per annum in total, with $65 billion as direct costs and $43 billion as indirect costs. The author concluded that diagnosis of HF could bear a substantial burden not only for patients but for the family, society, and country as a whole and, hence, emphasized a huge economic burden of HF.
Reyes et al.
11) reported the healthcare burden of HF in Asian countries compared with Europe and USA by using best available data of local researchers in each country. In the present analysis, longer length of stay was observed in Taiwan (15.7 vs. 12.5 days) and Thailand (14.2 vs. 7.5 days) whereas Malaysia had shorter length of stay (5.5 vs. 9.24 days), and baseline characteristics also showed higher burden in terms of comorbidities. Moreover, hospitalization costs were higher for patients with hospitalization experience (South Korea $10,714 vs. $8,887, Taiwan $4,790 vs. $2,388, and Thailand $7,181 vs. $3,606). Reyes et al.
11) studied the same countries but had different findings. The differences in our findings may be attributed to the methodology used as the data sources used varied considerably between the two studies. Moreover, Reyes et al.
11) did not mention the sample size for various countries and the cost-conversion year used for calculations. Similarly, when comparing costs of HF hospitalization in developed countries (e.g., USA) with Asian countries in this study, a huge economic burden on Asian nations is evident. In USA, the cost of HF hospitalization per patient (adjusted to 2015 USD) was $14,631,
12) and the gross domestic product (GDP) per capita in 2015 was $56,803.
13) The per-capita GDP for Asian countries in 2015 were $27,811, $22,639, $5,921 and $11,909 for South Korea, Taiwan, Thailand, and Malaysia, respectively. When comparing spend on hospitalization per patient versus GDP per capita, a large sum of money appears to be drained by healthcare in the Asian setting, thereby posing an enormous burden.
In South Korea, patients with HF routinely visit either clinics or tertiary hospitals for regular follow-ups, which is a trend seen with patients experiencing several minor conditions as well.
14) As HF patients with severe symptoms are usually hospitalized in tertiary hospitals, our findings are likely to be representative of the clinical reality in South Korea. Direct costs incurred by patients were similar between our study ($768.4) and that by Lee et al. ($868.2). The associated economic burden in patients with hospitalization ($4,101.4 vs. $422.9) versus those with no experience was highlighted in their study and underline the findings of our study as well.
15)
Since several patients with HF are unaware of the link between symptoms and HF, they usually wait until an acute exacerbation of symptom occurs in order to visit medical centers, thus requiring further treatment. This possibly explains the high hospitalization rates observed in Taiwan. A nationwide database study performed in Taiwan reported an increased incidence of hospitalization in patients with HF, possibly owing to increased incidence of HF in women.
16) In Taiwan, NHI covers 99% of the population.
17) In the present study, costs borne by NHI were up to 80% of the total costs, indicating the burden of treating HF to be mostly on the government. A majority of the study population was elderly (≥65 years) and had hospitalization experience during the study period, which could possibly be the reason for the high total cost of HF associated with Taiwan. One limitation of this study is that we included only one medical center, and our findings may not fully reflect the actual clinical situation in Taiwan.
In Thailand, medical reimbursement is financed by three institutes, wherein public employee benefit schemes (such as Civil Servant Medical Benefit Scheme) cover 7% of the population; Social Security Scheme, 15%; and the Universal Coverage Scheme, the rest (76%). Private insurances are uncommon in the country owing to high premiums and strict policies.
18) The total cost associated with HF was high in Thailand, possibly owing to the severity of the disease. We found that ER cost (both HF-related cost and cost per ER visit) was relatively high, probably because Thailand had the highest proportion of patients in NYHA class IV (17%), indicating that the patients may be more severely ill and have longer hospital stay. In addition, patients with HF in Thailand had longer ER stay and had received HF treatment in ER due to limited availability of inpatient beds. In general, patients with more severe HF are transferred to or admitted in medical schools/tertiary hospitals, and, thus, we believe that our findings are likely to be representative of the treatment reality of severe HF patients in Thailand.
HF is the third leading cause of hospitalization among circulatory system diseases in Malaysia. The hospitalized HF population may become a significant economic burden to Asian countries because of the growing elderly population and recurrent re-hospitalization. Similar to other countries,
19) hospitalization was associated with a higher cost of HF treatment in our countries of interest.
There was a high variability in the percentage of patients who experienced hospitalization during the observational period, ranging from 20.0% in South Korea to 93.5% in Taiwan. This discrepancy may be due to differences in HF patient management under the healthcare systems of participating countries. Moreover, decision criteria for admitting HF patients may be affected by budget allocation in each country.
The healthcare reimbursement system varies across countries. In Asian countries observed in this study, NHI system provides for the costs of medical services.
17)18)20)21) NHI, is a public health care system that receives budget for medical expenses as decided by the department of health of each country. A pool of private insurers exists within each setting, but their proportion and contribution vary in different countries. Since the healthcare system, hospitalization rate, and economic and wage levels vary among the countries of interest, interpretation and direct cross-country comparison of cost data is not desirable. However, we can conclude that the burden of HF is not limited to a specific country but is considerably a common issue in Asian countries overall. Hence, the real-world data collected in this study can perhaps be generalized.
The present study has several limitations. While functional class data were collected, the study might not have captured patients being treated for HF whose ICD code for the condition was not available. Furthermore, these patients may have fundamental differences in characteristics compared with those included in the study. Owing to the use of retrospective record review for data collection, certain values were missing and hence, results were analyzed using non-missing values. The study period of 1 year might have introduced certain limitations in data collection, considering the chronicity of the disease. Patients who did not survive the full year after the index date were excluded from analyses. In several instances, patients utilize extensive healthcare resources immediately before death. Thus, resource and cost estimates provided here might not be generalizable to all HF patients.
Future research in observational studies with longer follow-up periods and a larger population size, with inclusion of patients with short survival periods after HF, can provide additional insights regarding the economic burden of HF.
In conclusion, the economic burden of HF was considerably high in all four Asian countries included in this study. In particular, hospitalization accounted for a large proportion of HF costs. Therefore, a more streamlined treatment strategy is required to reduce hospitalization frequency and to lower the economic burden of HF. Furthermore, healthcare system support and standard treatment guidelines are also needed for the optimal management of HF in Asia.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download