INTRODUCTION
The outbreak of a novel coronavirus infection was first detected in Wuhan, China, in December 2019.
1 Globally, as of 9 June 2021, there have been 173,674,509 confirmed cases of coronavirus disease 2019 (COVID-19) and although the vaccination of populations is under way, the upward trend in infections continues.
2
A decrease in outpatient visits during an epidemic was observed with both the severe acute respiratory syndrome epidemic in 2003 and the Middle East respiratory syndrome epidemic in Korea in 2015.
3456 Regarding COVID-19 pandemic, it has been reported in the US and China that outpatient clinic visits also have decreased.
78 While the decline in outpatient visits may have resulted from attempts to avoid visiting hospitals out of fear of contagious diseases, there is the possibility that emphasis on nonpharmaceutical interventions to protect against the pandemic, such as observing social distancing and encouraging handwashing, have affected the incidence of diseases in the first place. Moreover, according to an analysis of the current status and trend of legal communicable diseases from January to April 2020 in Korea using the National Infectious Disease Surveillance of the Korea Disease Control and Prevention Agency (KDCA), the number of cases of second-class infections among waterborne and respiratory infections decreased over the most recent 3 years, including 2020.
9
Soldiers conscripted in South Korea are male and relatively homogeneous in terms of their age and physical condition, such as height and weight and show a similar disease distribution pattern every year. These soldiers are directly affected by governmental regulations regarding promotion of nonpharmaceutical interventions, such as control of vacation times and social distancing, and are also required to follow strict health guidelines including daily temperature measurements and emphasis on personal hygiene, such as handwashing. We expected to observe changes in outpatient visits and admissions to military hospitals for various diseases during the COVID-19 pandemic and we also expected to observe differences between the disease groups. We hypothesized that by analyzing the changes in outpatient visits and admissions to military hospitals, we would be able to identify the changes in medical demand due to the pandemic and construct a database for planning the supply of medical resources for future events. The aim of this study was to identify any differences in changes in medical resource use in military hospitals depending on disease type.
Go to :

METHODS
Data extraction and study population
Outpatient attendance and admission data from January 2016 to December 2020 were extracted from the Defense Medical Statistics Information System (DMSIS) database. The DMSIS is a database operated by the Armed Forces Medical Command (AFMC) to provide epidemiological information and increase its capability of situational awareness against natural and deliberate disease outbreaks.
10 DMSIS contains demographic information, such as sex, age, and rank and clinical information based on the 10th edition of the International Classification of Diseases (ICD-10), date and medical departments visited, and type of services used (outpatient and inpatient) from all 19 military hospitals across South Korea.
We analyzed the medical information of active enlisted soldiers (whose ranks ranged from trainee, private, private first class, corporal to sergeant), all male, from all the military hospitals in South Korea. To exclude error data such as medical use of reserves, the scope of our analysis was limited to individuals aged 18–32 years (i.e., men eligible for mandatory military service).
Definitions of variables according to diseases
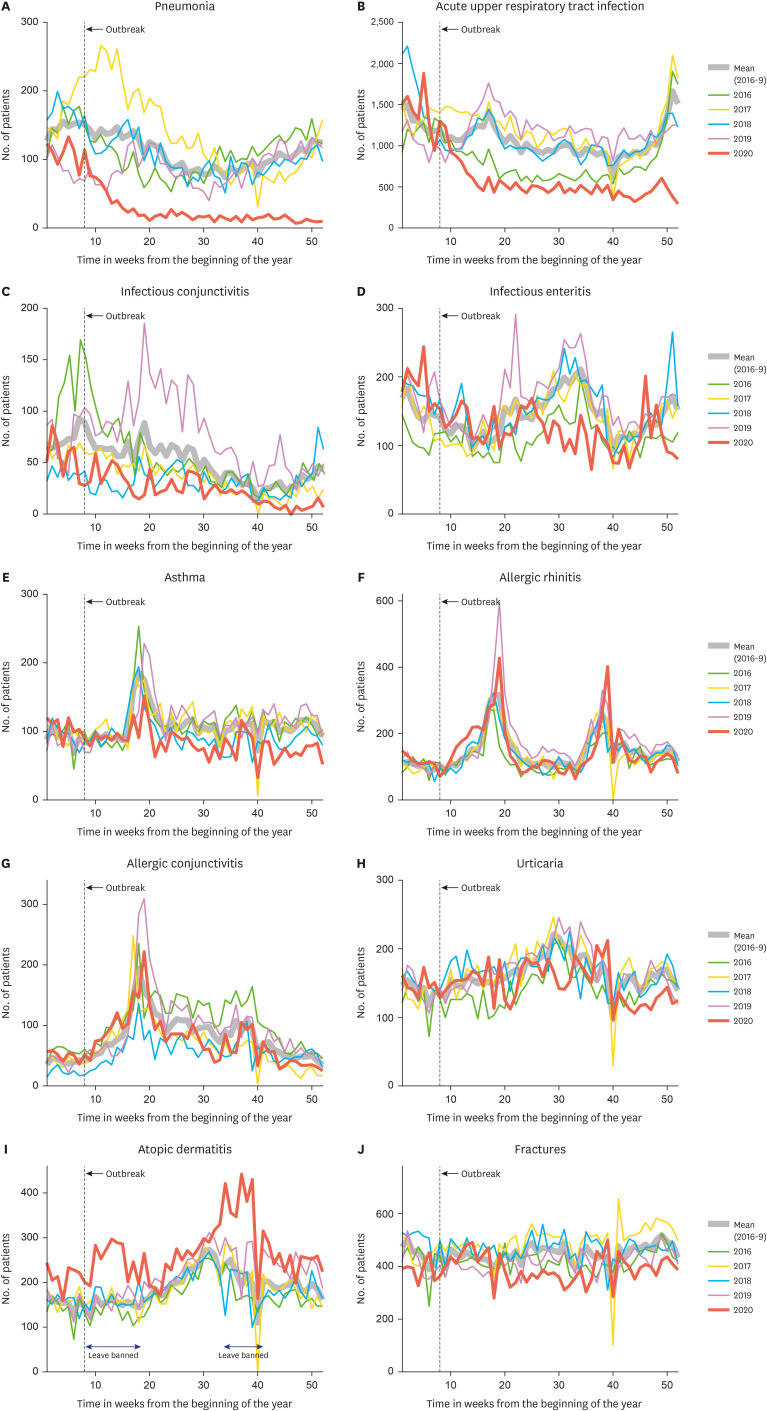
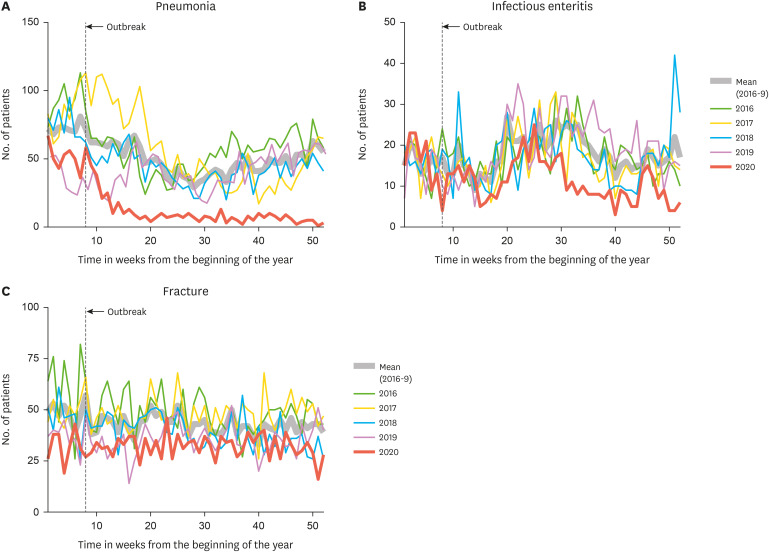
The data of infectious and noninfectious diseases for the analysis were selected using ICD-10 diagnostic codes. Pneumonia (J13-18, J10.0, J11.0), acute upper respiratory tract infection (J00-06), infectious conjunctivitis (B30, H13.1-06), and infectious enteritis (A00-09) were chosen as representatives of infectious diseases, and asthma (J45, J46), allergic rhinitis (J30), allergic conjunctivitis (H10.1), atopic dermatitis (L20), urticaria (L50), and fractures (Sx2, T02, T08, T10, T12) were chosen as representatives of noninfectious diseases.
The number of outpatient visits and admissions for each selected disease group was initially counted by date and then summed on a weekly basis to compare the number of visits over the same time period each year. A year consists of 52 weeks and the last day or two were not included in the analysis.
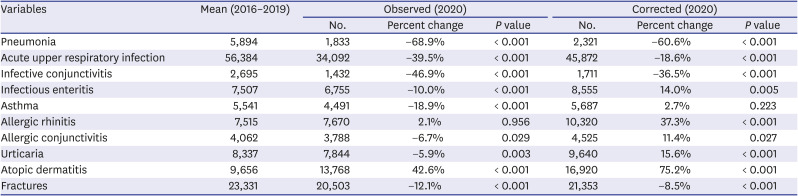
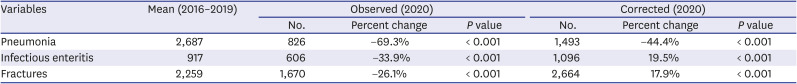
Additionally, to exclude the impact of the decrease in the total number of outpatient visits or admissions in 2020, we calculated the ratio of the total number of outpatient visits or admissions to the medical department treating each disease in 2020 to the average number of outpatient visits or admissions in 2016–2019 by week. The observed number in 2020 was corrected by this ratio. The medical departments involved were: internal medicine and emergency medicine for pneumonia, infectious enteritis and asthma; internal medicine, otorhinolaryngology, and emergency medicine for acute upper respiratory tract infections; ophthalmology and emergency medicine for infectious and allergic conjunctivitis; internal medicine, dermatology, and emergency medicine for atopic dermatitis and urticaria; and orthopedic surgery, rehabilitation medicine, and emergency medicine for fracture patients.
Statistical analysis
The weekly number and proportion of outpatient visits and admissions in 2020 for each disease group were compared with the average value of the 4 years from 2016 to 2019, for the same period. To consider seasonal variations, each weekly value was compared by paired t test. Since COVID-19 began to spread actively throughout Korea from the last week of February 2020, data from week 8 to week 52 in 2020 were compared with data averaged from the same weeks in 2016–2019 using a paired t test. Statistical analyses were performed with R software (version 4.0.2; R Foundation for Statistical Computing, Vienna, Austria).
Ethics statement
This study was conducted with the approval of the Ethics Review Committee of the AFMC (AFMC-20079-IRB-20-079). No informed consent was required from patients due to nature of the DMSIS database.
Go to :

DISCUSSION
The first COVID-19 case in South Korea was confirmed on January 20, 2020, while the pandemic started around the third week of February.
1112 To cope with the spread of the virus, a policy of social distancing—one of a number of nonpharmaceutical government interventions—was imposed from March 22. The Ministry of National Defense took quicker action and social distancing and soldiers' vacations and other leave were controlled from February 22. Vacations became available in May, although another restriction began on August 19 (ending on September 20). The ministry also mandated that all military personnel wear a facial mask and check body temperature before entering the base. Personnel with a temperature higher than 37.5°C were not allowed to pass the main gate of the base and were advised to visit the nearest military screening clinic to undergo a confirmatory test. Moreover, strict quarantine policies were applied in the military and personnel with or without symptoms who had traveled overseas, visited the country's outbreak hotspot areas, had had contact with suspected cases of COVID-19, or with confirmed cases of the virus were to be preventively isolated for 14 days from the very start of the pandemic.
13
Soldiers under mandatory military service are relatively homogeneous in age range, sex, and physical conditions, such as height and weight. They show a similar disease distribution pattern from year to year and are affected uniformly by the health policies of government. These characteristics of the group intensify the significance of this study, in which we have observed and analyzed the differences in medical use for a spectrum of diseases in the time of a pandemic.
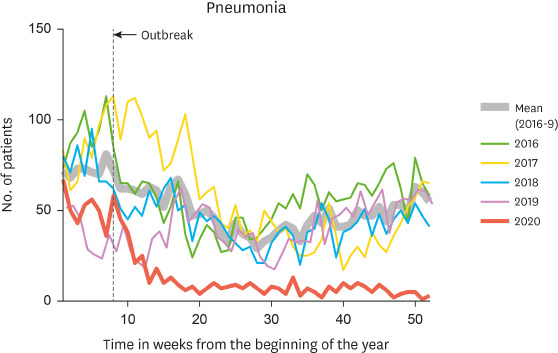
In this study, the most marked reduction of outpatient visits in 2020 was found for pneumonia. Although the reduction in incidence of pneumonia early in the pandemic period has been reported,
14 there may be an additional explanation for Korean soldiers. Since 2012, adenovirus has frequently been identified in respiratory specimens of patients with pneumonia in Korean military hospitals.
15 An epidemic occurred in late 2014 to 2015,
16 and it was reported that pneumonia was most commonly caused by adenovirus (79.3%), followed by influenza A virus (7.2%) and influenza B virus (3.2%) in a tertiary military hospital.
15 Prolonged viral shedding was observed in otherwise healthy adults with human adenovirus-55 infection;
17 the duration of viral shedding was estimated to be 55 days. This is considerably longer than the duration of other respiratory viruses, such as influenza virus, respiratory syncytial virus, and rhinovirus, which may contribute to the persistent incidence of adenovirus pneumonia in this military group. In this sense, we assume that nonpharmaceutical interventions such as encouraging handwashing and the mandatory wearing of masks have had an enormous effect on the transmission of adenovirus, resulting in a dramatic decrease in the incidence of adenovirus pneumonia in this group.
The number of outpatient visits for acute upper respiratory tract infections appears to have decreased for the same reason as for pneumonia. A recent report suggested that wearing masks reduces the emission of virus-laden aerosols and droplets,
18 and a meta-analysis indicated that the use of masks provides a significant protective effect (odds ratio = 0.35; 95% confidence interval, 0.24–0.51) in preventing respiratory virus transmission.
19 This evidence suggests that the transmission of respiratory viruses in general, not only adenovirus but also others including influenza virus, can all have been affected. As a result, there were astonishingly few cases of seasonal influenza in Australia, Chile, and South Africa between April and July 2020, and this has been attributed to these changed personal hygiene practices.
20
Changes in the number of outpatient visits for infectious conjunctivitis demonstrate the effects of increased handwashing and emphasis on social distancing more clearly than those of wearing masks in the COVID-19 pandemic. Infectious conjunctivitis is basically a disease transferred through contact directly by hand or sharing objects, such as towels. The results of our study correlate with those presented by the KDCA in which the proportion of infectious keratoconjunctivitis cases out of the total number of visits decreased in 2020.
21 While the infectious disease specimen monitoring data from the KDCA show that the incidence of keratoconjunctivitis peaks in autumn, the military data consistently show a peak in the springtime. This phenomenon can be explained by the fact that military training sessions start and are active in the spring, suggesting that increased contact between individuals results in the higher incidence of the disease.
The most common cause of acute gastroenteritis is norovirus.
22 Some reports have confirmed a decrease in norovirus cases during the COVID-19 pandemic.
2324 Our results show that the number of outpatient visits for this disease has decreased compared with the last 3 years, but proportionally less so. This may be a result of the soldiers' lifestyle in that they live and eat in groups, which makes acute gastrointestinal infections more likely to spread. Improved implementation of nonpharmaceutical interventions seems to have reduced gastrointestinal infectious diseases, but not to the same degree as for respiratory infectious diseases.
Compared with the reduction of outpatient visits for several infectious diseases in 2020, that for allergic diseases (except for atopic dermatitis) was only slightly decreased or unchanged. In the cases of allergic rhinitis, allergic conjunctivitis, and asthma, diminished air pollution due to lockdown, increased indoor activities, and frequent use of masks may have contributed to the decrease in outpatient visits. A recent study reported reduced health care use related to asthma, along with less systemic steroid administration and fewer rhinovirus infections during the pandemic in patients with childhood asthma, although with no marked change in the levels of air pollution before and after the pandemic.
25
In contrast, we found a significant increase in the number of outpatient visits for atopic dermatitis in 2020, as was the case for urticaria, although here there was an increased proportion of visits. Spending more time indoors may have increased exposure to indoor allergens (e.g., tobacco, organic compounds, house dust mites, etc.) leading to more visits to clinics that specialize in skin problems. However, the number of outpatient visits for atopic dermatitis rose markedly during weeks 10–20 and 30–40, which correspond to the period when leave was officially banned due to a social outbreak of COVID-19 in the military (
Fig. 1I). In this period, medical leave was not available as at other times, which required soldiers who were taking regular medicine for their chronic illness to visit military hospitals more frequently.
Fractures were chosen as a measure of the change in the number of injuries related to outdoor activities. Much of the outdoor training where many people gather was cancelled or downsized during 2020 and this likely led to a distinct reduction in outpatient visits for fractures in that year. Outdoor exercise such as soccer was not officially banned, but the mandatory wearing of masks could well have reduced the frequency of such activities, leading to a lower occurrence of fracture.
Some limitations of this study should be noted. First, we examined the number of outpatient visits and admissions rather than the incidence or prevalence. While the term incidence is applicable in infectious diseases, the number of visits does not mean incidence in allergic diseases. Due to the heterogeneity of disease categories, we selected and compared the actual number of outpatient visits and admissions, placing an emphasis on the burden of medical use. The total number of new enlisted soldiers was 261,204 in 2016, 227,115 in 2017, 222,517 in 2018, and 224,062 in 2019. Although the total number of enlisted soldiers registered in 2020 was not reported, it is apparent that the yearly number did not differ greatly during the study period; accordingly, we assume that the numbers of visits reflect incidence or prevalence.
Second, these data from a military hospital cannot assess the change in the number of moderate-to-severe forms of allergic disease. Soldiers undergo a check for their medical status when they enter the military and individuals with severe illness are not enlisted. For this reason, we mostly analyzed outpatient visits rather than the admissions in allergic diseases. The number of acute exacerbations or new occurrences requiring admission is relatively small in military hospitals compared with that in community hospitals.
In summary, during the COVID-19 pandemic, the numbers of respiratory and conjunctival infections, as well as fractures, were observed to have decreased, while allergic diseases did not change or increased in military hospitals. These results are important because they illustrate the changing patterns in lifestyle caused by encouraging the adoption of nonpharmaceutical interventions, and additionally for the military, by the mandatory containment strategies and quarantine policies implemented during the pandemic and their effect on medical needs for both infectious and noninfectious diseases. The results of this study may be useful for predicting military medical use in future pandemic events in this group.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download